Re-exploration of the neck for residual or recurrent hyperparathyroidism or thyroid cancer is technically challenging and preoperative imaging is very useful for guiding surgery. For both pathologies, nuclear medicine techniques have emerged as the primary preoperative imaging modalities. The precise techniques used continue to evolve as new equipment and technology (fusion imaging) become available. The role of
Every attempt is made at the initial operation to ensure complete removal of the offending lesions in patients who undergo parathyroid or thyroid surgery. Reoperation in the neck is technically challenging and associated with higher complication rates. Preoperative imaging before re-exploration of the neck is useful to help guide surgery, with the goal of decreasing associated morbidities. This article reviews the role of nuclear medicine imaging in the evaluation of patients undergoing reoperation in the neck for persistent or recurrent hyperparathyroidism (HPT) and thyroid cancer. The discussion is limited to well-differentiated pathologies because the role of reoperative surgery for medullary thyroid cancer is controversial; anaplastic thyroid cancer is not iodine avid and there are very limited data on use of 2-[ 18 F]-fluoro-2-deoxy-D-glucose (FDG) positron emission tomography (PET) in this disease.
Parathyroid scintigraphy
Primary HPT, or inappropriate excess of parathyroid hormone secretion, is caused by a solitary parathyroid adenoma in 80% to 85% of patients, parathyroid hyperplasia in 10% to 15%, and multiple parathyroid adenomas and parathyroid carcinoma in 2% to 3% each . Secondary and tertiary HPT occurs in patients with chronic renal failure. Parathyroidectomy is the treatment of choice for primary HPT and may be indicated in patients with secondary or tertiary HPT if medical intervention is insufficient . The cure rate is high (>90%) when an experienced surgeon performs the operation .
Preoperative nuclear medicine imaging facilitates successful localization of the adenoma by the surgeon and has become increasingly critical with the recent growth of minimally invasive parathyroidectomy, which uses a targeted surgical approach. Most of the literature focuses on the use of nuclear medicine imaging before initial parathyroid surgery, but imaging is also useful for evaluating patients who present for reoperation because of persistent or recurrent disease.
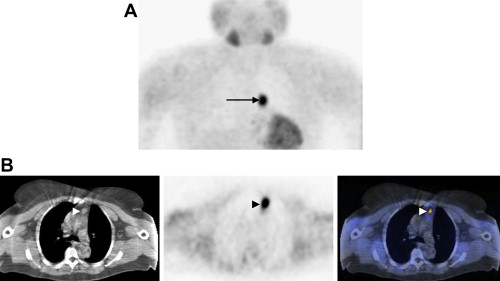
Several radiotracers are available for parathyroid scintigraphy. Thallium-201 ( 201 Tl)-technetium-99 m ( 99m Tc)-pertechnetate subtraction scanning is of historical interest. At present, the radiotracer of choice for parathyroid scintigraphy is 99m Tc-sestamibi. 99m Tc-sestamibi is a lipophilic cation that is ultimately sequestered in mitochondria because of electrical potentials. The presence of larger numbers of mitochondria-rich oxyphil cells in parathyroid adenomas is thought to be responsible for slower release of 99m Tc-sestamibi from hyperfunctioning parathyroid tissue versus adjacent thyroid tissue, which allows distinction between the two ( Fig. 1 ) .
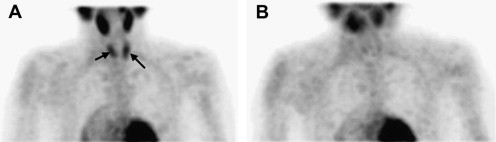
Overall, 99m Tc-sestamibi parathyroid scintigraphy has good sensitivity (4%–96%) for the detection and localization of single adenomas in patients with primary HPT ( Fig. 2 ) . For tertiary HPT, the sensitivity for preoperative adenoma localization is about 76% . Most authors defined a true-positive study not only as adenoma detection, but correct localization to a quadrant in the neck as related to the thyroid gland. The sensitivity of 99m Tc-sestamibi is not as high for the detection of double adenomas (30%–83%) or parathyroid hyperplasia (45%–62%) ( Fig. 3 ). In all histopathology types, however, 99m Tc-sestamibi parathyroid scintigraphy has been shown to have higher sensitivity than ultrasound, CT, or MRI, which have reported sensitivities ranging from 45% to 80% . Because most cases of secondary and tertiary HPT have some component of multigland disease , this is welcome news.
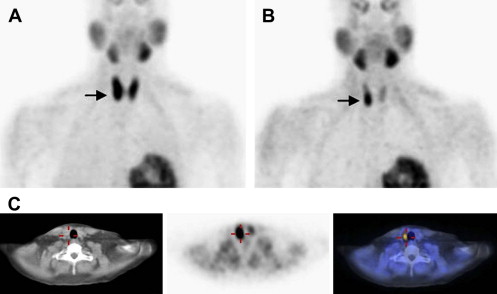
The wide range of reported sensitivities is caused by the various imaging techniques used ( Table 1 ). The choice of technique is in part determined by the available nuclear medicine cameras at an imaging center. A limited number of studies have directly compared three-dimensional single-photon emission CT (SPECT) with two-dimensional planar imaging for detection of parathyroid adenomas. The false-negative rate is reported to be lower for SPECT and SPECT allows better detection of small parathyroid adenomas immediately posterior to the thyroid gland ( Fig. 4 ) . Hybrid SPECT-CT, which provides fusion of functional and anatomic information, may offer even better localization of adenomas, especially in patients with ectopic glands ( Fig. 5 ) .
| Author | N a | Technique | % Sensitivity (specificity) | Comments | |
|---|---|---|---|---|---|
| Planar | SPECT | ||||
| Taillefer, et al | 23 | Dual-phase planar (15 m and 2–3 h) | 90 | ||
| Billotey, et al | 43 |
| 86 | 90.5 |
|
| Perez-Monte, et al | 52 |
|
| ||
| Blanco, et al | 41 | Dual-phase planar (10 m and 3 h) | 92 |
| |
| Sfakianakis, et al | 62 | Immediate and delayed (2–5.5 h) planar and SPECT | 84 (95) | 94 (92) | |
| Ishibashi, et al | 20 | Dual-phase planar (10 m and 2–3 h) | 83 (83) | Sensitivity and specificity MRI and US: 78%–80% and 40%–60% | |
| Hindie, et al | 30 |
|
|
| |
| Moka, et al | 92 |
| 87 | 95 | 11 thyroid adenomas with 99m Tc sestamibi uptake |
| Civelek, et al | 338 | Delayed SPECT | 87 |
| |
| Lorberboym, et al | 52 |
|
| For the SPECT study: pertechnetate subtraction imaging also done | |
| Ruda, et al | 20,225 | Various | 88 |
| |
| Lavely, et al | 110 |
| 57 |
|
|
a Patients with primary hyperparathyroidism. Studies by Ishibashi et al, Billotey et al, and Blanco et al included patients with secondary hyperparathyroidism.
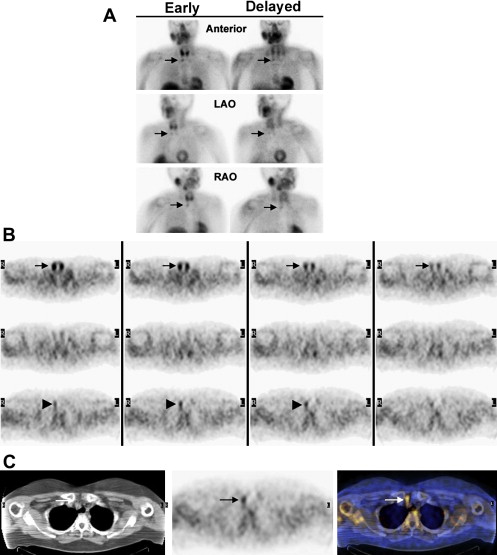
Lavely and colleagues have reported the most comprehensive study of 99m Tc-sestamibi parathyroid scintigraphy in the recent years of minimally invasive parathyroidectomy. The authors studied 110 patients with primary HPT and no prior neck surgery and compared the performances of the various modalities (planar, SPECT, SPECT-CT), techniques (single- and dual-phase), and combinations of modalities and techniques that are currently available. SPECT-CT imaging 15 to 30 minutes after injection in combination with any delayed imaging method, approximately 2 to 3 hours after injection, emerged as the best technique for preoperative parathyroid adenoma localization. The early imaging provided the functional anatomy of the thyroid gland versus the parathyroid adenoma. The accuracy of early SPECT-CT plus any delayed imaging for precise localization of parathyroid adenomas was 86% versus 67% to 82% for all other combinations of modalities and techniques .
Despite its apparent advantage for parathyroid scintigraphy and other nuclear medicine studies, hybrid SPECT-CT is not yet widely available, limiting the clinical impact of the findings by Lavely and colleagues . Most nuclear medicine practices, however, do use gamma cameras with planar and SPECT capabilities. When SPECT-CT is not an option, dual-phase planar or SPECT imaging is probably the best alternative for localization of parathyroid adenomas. SPECT imaging tends to be more accurate than planar imaging .
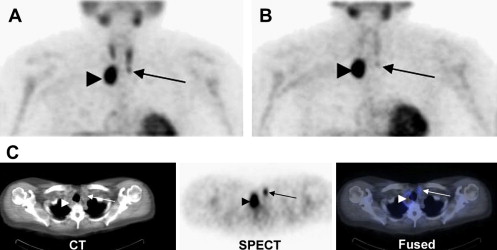
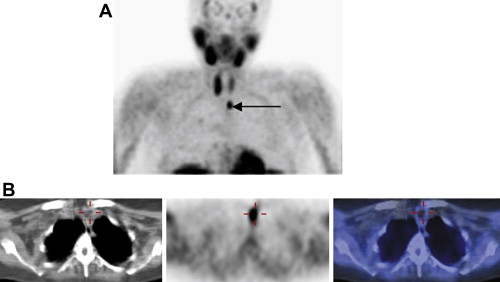
The most common cause for a false-positive 99m Tc-sestamibi study is accumulation of the radiotracer in thyroid adenomas . Thyroid carcinomas and inflammatory thyroid disease may also result in false-positive studies. Dual-isotope subtraction imaging with a thyroid imaging agent or fusion imaging with hybrid SPECT-CT may lower false-positive results caused by thyroid disease ( Fig. 6 ). Inflammatory and malignant lymphadenopathy also has resulted in false-positive findings.
Falsely negative 99m Tc-sestamibi parathyroid studies have been reported to be caused by multigland hyperplasia, small adenoma size, obscuration of the adenoma by unusually high uptake in the thyroid gland, and prior thyroid surgery with resultant prominent muscle uptake . These etiologies for false-negative scans are highly relevant as the discussion is turned to the use of imaging in the reoperation setting.
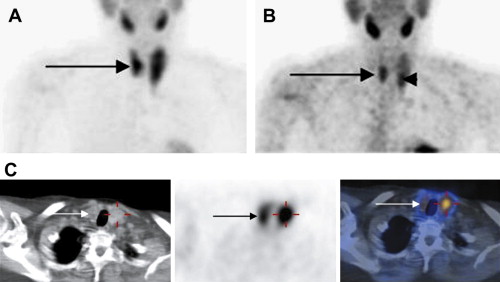
Recurrent primary hyperparathyroidism
Understanding of the diverse etiologies for recurrent HPT is crucial to understanding the use of imaging in the reoperative setting. Persistently elevated parathyroid hormone levels after curative therapy may be caused by progression of underlying disease after response to bone mineralization or failure of the initial surgery. Failure to recognize and adequately resect multigland disease at the time of initial surgery is one of the most common causes for failed initial surgery . This remains a challenge because detection of multigland disease is a limitation of 99m Tc-sestamibi parathyroid scintigraphy. Another significant cause of failed initial surgery is lack of detection of an ectopically located gland . The frequency of multiple or ectopic glands, often coexisting, as the cause for recurrence has been reported to range from 44% to 70% . In one study, 99m Tc-sestamibi parathyroid imaging was reported to have a sensitivity of 65% for localizing these recurrences .
Ectopic parathyroid adenomas can be located in the paraesophageal region (28%); (nonthymic) mediastinum (26%); intrathymic (24%); intrathyroidal (11%); carotid sheath (9%); and high cervical position (2%) . 99m Tc-sestamibi parathyroid imaging has been shown to be extremely useful for localization of ectopic adenomas. The value of this technique increases with the use of SPECT and SPECT-CT. SPECT-CT allows visualization of corresponding anatomy, for differentiation of thyroidal from nonthyroidal tissue and determination of the relationship to adjacent structures. The precise localization of mediastinal and intrathyroidal adenomas is a great aid to surgical management ( Fig. 7 ).