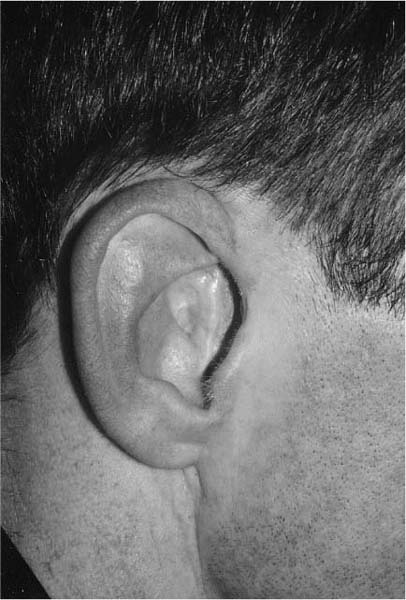
Chapter 12 The canal-wall-down (CWD) mastoidectomy finds favor with otologists primarily for one reason: the technique reduces the risk of persistent or recurrent cholesteatoma. Whether one takes the posterior canal wall down or not, there is a significant incidence of epithelial pearls that remain behind and can form the nidus of new disease.1 These pearls may or may not cause clinically detectable findings. Smythe1 reported that recurrent cholesteatoma from a retraction pocket occurred in 14% of intact canal-wall ears as compared with 1% of ears treated with mastoid obliteration and tympanic reconstruction. He concluded that the best way to reduce the incidence of cholesteatoma complications to the greatest possible degree long-term was to remove the posterior canal wall. Nevertheless, after a CWD mastoidectomy, a patient is left with several problems inherent in the open cavity. The exposed bone of the mastoid leaks tissue fluid, which is a rich medium for bacterial growth. Unlike other areas of the head and neck, the mastoid, and in particular the sclerotic mastoid, is not particularly well vascularized.2 The combination of mediocre blood supply and weeping tissue fluid means that control of bacterial ingrowth can be challenging. Not only may healing be marginal or delayed, but also the patient may need to avoid moisture for life. Recurrent aural discharge afflicts 10 to 60% of patients with an open mastoid cavity.3,4 Other complications, such as perichondritis of the pinna, have been reported.4 It is widely taught that the incidence of discharge or other infectious complications can be minimized by lowering the facial ridge, making the cavity large, and providing a generous meatal opening,3 but these maneuvers also have their drawbacks. For one, hearing aids are often required in these patients. Although it is undesirable to fit a hearing aid in a discharging mastoid cavity, it is also a problem to construct a mold for an enlarged meatus.3,5 In addition, lowering of the facial ridge may decrease the depth of the middle ear space, which makes ossicular reconstruction difficult and hearing less than optimal.6 Although a large meatus may reduce the incidence of postoperative drainage, it is often cosmetically unappealing (Fig. 12–1). A large mastoid cavity can draw the pinna inward, causing a noticeable deformity of the auricle. It may also draw the medial concha inward and displace the pinna laterally. The dizziness associated with caloric stimulation is another drawback of a large open mastoid, and patients sometimes have to limit their exposure to water and wind. The ear loses its natural ability to clean itself, and wax and squamous debris build up over time. A foul smell can develop, which can be an irritation and source of embarrassment. In most cases, the mastoid bowl needs to be cleaned on a routine basis every 6 to 12 months. Water exposure can lead to infection. This is especially disappointing to patients who wish to swim regularly. In fact, it is not the size of the cavity that is crucial. In a comparative study, ears with a small open mastoid bowl have fared no worse than those with an obliterative flap.1 It is believed that the critical issue is the adequacy of the meatal opening as determined by the ratio of the meatal circumference to the volume to the mastoid cavity. One must have an opening sufficient to allow free circulation of air. Therefore, many reasons exist not only for CWD mastoidectomy, but also for reconstruction of the posterior ear canal and obliteration of the mastoid. Hearing aids are easier to fit into an obliterated cavity than into an open cavity. The obliterated cavity is also more likely to retain its epithelial migratory potential and be self-cleaning because it is smaller.3 Obliteration of the mastoid cavity leaves a smaller surface area. Healing is therefore theoretically faster, and there is a reduced likelihood of developing granulations. Obliteration has been shown to significantly reduce the symptoms associated with the open mastoid. In a survey of patients with recurring mastoid disease, groups were treated either with revision mastoidectomy or obliteration.3 The preoperative symptom scores were not significantly different, but the patients treated by obliteration had a significantly lower postoperative symptom score.3 Some recommend mastoid obliteration as a routine procedure in all mastoid surgery.7 FIGURE 12–1 Typical appearance of an ear following canal-wall-down mastoidectomy with large meatoplasty. Nevertheless, mastoid obliteration should not be undertaken lightly, because it carries a risk of enclosing cholesteatoma within the cavity. Computed tomography (CT) may or may not be effective in detecting these residua. A study was conducted in cadaver temporal bones in which cholesteatoma pearls were covered either with hydroxyapatite or muscle.8 Scanning was effective in detecting small pearls within the cavity obliterated with hydroxyapatite, but not so effective when muscle was used. In practice, however, obliteration has been safe. When CT was performed on 31 ears after mastoid obliteration with hydroxyapatite, there was no residual cholesteatoma in the obliterated area.8 A muscle flap may have an advantage over hard tissue replacement because an epithelial cyst may present as a swelling beneath the flap. Mastoid obliteration may be contraindicated if there has been removal of a malignant tumor, if there are otogenic intracranial complications, if cholesteatoma has not been totally removed, or when air cell removal has been incomplete.9 Although there are many options for mastoid obliteration, all depend on a rich blood supply for success. Well-vascularized flaps are the best options when there has been extirpative surgery for cancer or osteoradionecrosis. The goal of reconstruction of the posterior external auditory canal is to provide a safe, dry mastoid and restore hearing to near-normal levels. No single procedure has yet been devised that entirely accomplishes these purposes consistently. Various materials have been used to fill the mastoid, including fascia, fat, muscle, cartilage, bone paste, cancellous bone strips, bioactive glass ceramics, Proplast (a combination of polytetrafluoroethylene and glassy carbon fibers) methylmethacrylate, and ionomer-based bone substitutes.5 Most biologic tissues have a tendency to atrophy over time, and some otologists recommend overfilling the cavity to compensate for the expected loss of the volume of the obliterating tissues over time.10 Because the final shape and size of the obliterated mastoid cavity cannot be predicted, using biologic tissues for obliteration can be a drawback. The earliest obliteration techniques involved flaps of local tissue. One of the early methods was that of Mosher11 in 1911. He used soft tissues from the back of the auricle and pedicled toward the temporalis muscle. Mosher always performed a simple mastoidectomy first, and then lowered a greater part of the posterior canal wall, leaving a bridge of bone external to the aditus in place. Popper12 described another early method in which he used periosteum to line the mastoid. He made a postauricular incision through the skin and subcutaneous tissues, retracting the posterior skin flap as far back as possible. He then made a horseshoe-shaped incision through the periosteum, creating an anteriorly based flap. Popper’s aim was not to entirely obliterate the cavity but to provide a viable lining with good blood supply to facilitate healing. Meurman and Ojala13 described filling the lower part of the cavity by using an inferiorly and caudally based postauricular musculoperiosteal flap. Guilford14 attempted a more complete obliteration by combining the Meurman and Ojala flap with a superiorly pedicled postauricular flap. These early flaps all demonstrated variable viability and some atrophy of tissue over time. In an effort to provide more consistent and longer-lasting results, Palva15 in the early 1950s began using a meatally based musculoperiosteal flap for obliteration and simultaneous reconstruction of the posterior canal wall. This flap retained the essential form of Popper’s flap but included all the tissues between the skin and bone. For the Palva flap, the skin incision is made 1.0 to 1.5 cm behind the postauricular fold to facilitate liberation of the tissues posteriorly (Fig. 12–2). The horseshoe-shaped incision includes all the subcutaneous tissues from the retroauricular area down to the bone, theoretically preserving the facial nerve branches to the postauricular muscles and forestalling atrophy of the tissues.7,15 The flap could be made broad and long to allow obliteration of even large mastoid cavities. Despite its good viability, the Palva flap demonstrated gradual atrophy in patients over years of follow-up. New methods of obliteration were sought. The soft tissue flaps mentioned above are all based on a random-pattern blood supply. If they are raised with a length-to-width ratio of greater than 1:1, ischemia of the distal portion is a risk, and subsequent necrosis and contraction of the flap would result in inadequate coverage and fill of the cavity.4 Another drawback to these local flaps is that they rarely have sufficient bulk or plasticity to completely line and fill a large mastoid.4 Another flap used to obliterate the mastoid has been the temporalis muscle flap, which is pedicled anteriorly. Experience has shown that these flaps have a tendency to undergo atrophy, and the majority shrink down to the point that the resulting cavity is as large as it was originally.9 This is probably because the muscle becomes denervated and the blood supply becomes compromised, making the flap in effect a free muscle graft.4 In an effort to overcome such problems, practitioners have advocated the use of vascularized temporalis fascia. Both the deep and superficial temporalis fascia have been used. The deep temporalis fascial flap, “the Hong Kong flap,” is based on the middle temporal artery. It is thin, strong, and pliable, with more than adequate surface area to line the entire mastoid cavity.16 Its proponents claim that because it is translucent in nature, detection of recurrent disease is not compromised.16 Although the flap is adequate for achieving a healthy dry ear, it does not completely obliterate the mastoid or reconstruct the posterior canal wall. The superficial temporalis or temporoparietal fascial flap is a good option for mastoid obliteration. The flap is thin, pliable, and can accept skin grafts.17 It also provides enough bulk for the obliteration of large mastoid defects.17 To avoid compression on the pedicle of the flap when it is rotated into the cavity, the middle fossa dura can be skeletonized above the ear canal at the ridge formed by the root of the zygomatic arch.4 A vertical incision is made through the scalp in the temporal area. Dissection is carried out just deep to the hair follicles, and bipolar cautery is used to avoid damage to the vessels. Care must be taken not to damage the frontal branch of the facial nerve. The flap incorporates an area of temporoparietal fascia 8 × 7 cm.4
RECONSTRUCTION OF THE POSTERIOR EAR CANAL
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree