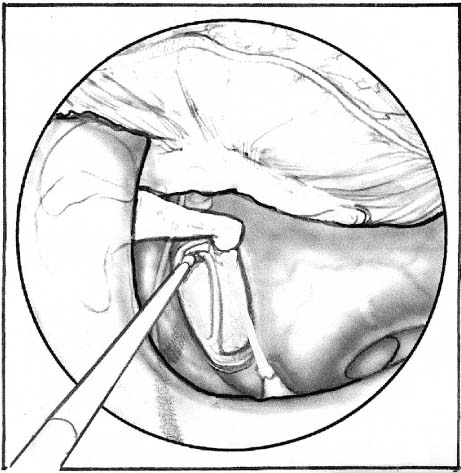
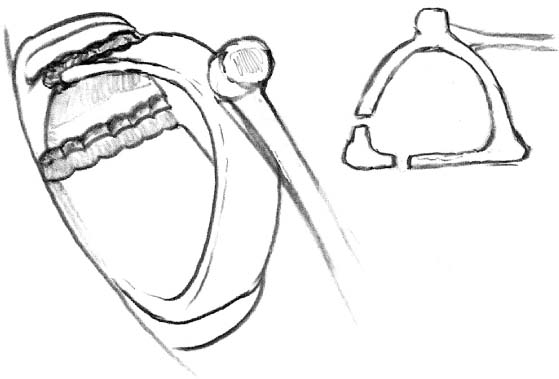
Chapter 17 Over the past decade the emphasis on surgery has been to find ways of performing minimally invasive techniques using lasers and endoscopes. Many otologic procedures already fit the category of minimally invasive, or are already being done in the surgeon’s office operating room, thus avoiding hospitalization and all the associated costs that accompany it. The advantages of minimally invasive procedures are many and include the fact that procedures can be performed safely in an office operating room or surgery center. Patients especially like procedures that are done in the office, because both patient and surgeon time is minimized, the large expense of inhospital surgery is saved, all procedures are performed using topical or infiltrative local anesthesia, and the results are as good as those of more extensive procedures. Starting with laser stapedotomy minus prosthesis (laser STAMP), a variety of minimally invasive procedures including laser-assisted tympanostomy (LAT), endoscopic middle ear exploration, inner ear perfusion, and fat myringoplasty are described here, and the necessary equipment and anesthesia are presented. Minimally invasive surgical procedures can be an enormous addition to the otologist’s armamentarium. The minimum size of the minor surgery room should be 150 square feet, although a larger room is preferable. Two instruments that are not standard to all otologic offices but contribute tremendously to the success of office-based otologic surgery are the CO2 laser and the 1.7-mm rigid otoendoscope (Smith-Nephew Richards, Memphis, TN). The laser is instrumental in creating an instant, bloodless, and nearly painless myringotomy for middle ear aeration or other procedures. The otoendoscope provides near microscope-quality images of the middle ear, allowing the surgeon to see areas not visualized by the operating microscope. The Lumenis CO2 laser (Lumenis Ltd., Yokneam, Israel) is used with a Microslad optical delivery system (Lumenis Ltd.,Yokneam, Israel) attached to the microscope. A remote foot pedal allows the surgeon to fire the laser with precise control. The laser allows variable spot size (0.65 to 3.4 mm), power (5 to 30 W), and pulse duration (0.05 seconds to continuous). The Surgi-Touch CO2 flash scanner (Lumenis Ltd.) is used to make a circular opening in the tympanic membrane. The flash scanner beam moves in a spiral pattern at a constant velocity and must be in sharp focus. The laser beam never lingers at any given point longer than the thermal relaxation time of the tissue, resulting in char-free ablation and minimal depth of laser energy penetration. This provides the ad-vantage of creating a controlled tympanostomy of a predictable size and depth with a single burst of focused laser energy. Pulse duration of 0.15 seconds and a power of 10 to 20 W are typically used to penetrate the tympanic membrane. Note that laser safety precautions must be followed at all times when using any laser. All persons in the procedure room (including the patient) are required to wear eye protection in the form of laser safety goggles when the laser is being fired. Two different-angled otoendoscopes are used, with 0-degree and 30-degree views. The 30-degree angled scope is the most commonly used scope and provides visual perspectives of the middle ear not seen with direct microscopic visualization. These scopes are shorter and narrower than standard nasal rigid endoscopes usually seen in an otolaryngology office, with a length of 10 cm and a diameter of 1.7 mm. The 2.7-mm endoscopes are too large to be useful. The otoendoscopes have excellent optics and produce images of superior quality comparable to the operating microscope. An Olympus camera is attached to the otoendo-scope (Olympus America Inc., Melville, NY). The camera is connected to color monitors, which allows the surgeon, assistants, patient, and patient’s family members to view the procedure. The procedure can be documented with video and/or photos; the authors employ a super-VHS recorder and a color video printer. Multiple copies of the still photos can be immediately produced for placement in the office chart, for explaining the procedure to the patient, and for the patient’s personal medical records. The otoendoscope can also be used without the camera if the surgeon prefers to look directly through the eyepiece of the endoscope. An essential component of almost all forms of otologic surgery is the operating microscope. It is preferable to use a standard wall-mounted microscope that is stable and frees both of the surgeon’s hands for operating. The microscope has a 300-mm objective lens and adjustable magnification. The speculum holder can be very useful at stabilizing the speculum while freeing both of the surgeon’s hands for the procedure. A standard foot-pedal operated suction is also essential for otologic surgery. Instruments that are usually found in a minor surgical procedure set are frequently needed, including No. 15 blades and handles, skin scissors, skin hooks, forceps, and so on. Standard otologic instruments should be available and sterile if needed. These instruments include various-sized speculums and a full range of hand-held suction tips, picks, hooks, curettes, cup forceps, alligator forceps, Bellucci scissors, sharpened sickle knives, round knives, and so forth. Anesthetic options for minimally invasive office-based otologic surgery include topical anesthesia or local (injected) anesthesia. These options are usually sufficient to keep almost all adults and many pediatric patients comfortable and relaxed during otologic surgery. In 1968, Silverstein developed a technique of anesthetizing the tympanic membrane utilizing topical tetracaine without the use of injections.1 Since that time, over 3000 cases have been successfully performed using this topical anesthesia. The method is well tolerated by patients because needle injections are avoided. It also allows the anesthetization of younger children who otherwise would not cooperate with conventional injections.1 The topical tetracaine adequately anesthetizes the tympanic membrane, and the effects last for approximately 1 hour after removal of the liquid from the ear canal. The surgeon must be aware that the ear canal and middle ear mucosa are not anesthetized. Consequently, topical tetracaine anesthesia should be used for procedures involving the tympanic membrane only, such as LAT, ventilation tube insertion, and minor middle ear exploration where the mucosa is not traumatized. To avoid pain during the procedure, instrumentation of the ear canal must be avoided. More extensive middle ear work, including exploration of the middle ear using otoendoscopes or chemical perfusion of the inner ear, generally requires additional anesthesia in the form of injections. The technique of topical anesthesia using tetra-caine solution is as follows. A single-use vial is created by measuring 160 mg of tetracaine powder and placing it into a 1-cc vial. The greatest efficacy is obtained when the solution is prepared just prior to use. Isopropyl alcohol (0.2 cc) is added to the vial, and the contents are shaken until the tetracaine powder is completely dissolved, producing an 80% solution. The patient’s ear is inspected with an otoscope or microscope to ensure that the tympanic membrane is unobstructed and that no perforation of the tympanic membrane exists. Any defect in the tympanic membrane precludes the use of topical tetracaine solution. Cerumen and other debris are removed if necessary. The patient is placed on his or her side on the procedure table with the affected ear facing upward. Using a 27-gauge needle on a tuberculin syringe to direct the flow, the surgeon places 0.2 cc of tetracaine solution into the ear canal to be anesthetized. Do not inject! It is best to visualize the tympanic membrane to ensure that the medicine has covered the drum. The patient is then instructed to remain in the lateral decubitus position for a minimum of 8 minutes. No ill effects are encountered if the medication is left in place longer than this minimum allotted time period. The patient is then instructed to turn his or her head to drain the ear of the medication by gravity. The surgeon then aspirates any remaining solution from the ear canal and tympanic membrane with a suction tip. It is imperative that no tetracaine is left behind that could enter the middle ear and diffuse into the inner ear, causing transient violent vertigo lasting several hours. At the same time, the surgeon can verify adequate anesthesia by touching the tympanic membrane with the suction tip and assessing for residual sensation. The surgeon is free to perform the procedure within 1 hour of the medication’s removal. For younger children who cannot remain still in the lateral decubitus position for a full 8 minutes, an alternate technique is used. A few drops of tetra-caine are instilled in the ear canal as above. Then a 9 × 15 mm Merocel Pope ear wick (Medtronic Xomed Inc., Jacksonville, FL) is gently inserted into the canal so that it nearly touches the tympanic membrane. The remainder of the solution is used to expand the wick so that it touches the tympanic membrane and fills the canal. The child is then free to move about for 10 minutes until the wick is removed for the procedure. It is important first to review the history of surgery for otosclerosis, which is marked with major breakthroughs by a number of pioneering otologists. In the 1950s, Rosen2 developed the stapes mobilization procedure. In patients with stapes fixation due to otosclerosis, the stapes footplate was fractured with chisels or picks. Hearing was improved, though only temporarily. Refixation of the stapes usually occurred after several months. Fowler3 introduced the anterior crurotomy technique of stapes mobilization in 1956 with results similar to those of Rosen. In 1958, Shea4 developed the stapedectomy procedure, which produced long-lasting results. Since that time, Shea’s procedure or modifications of the technique have remained the most popular method for improv-ing hearing in patients with otosclerosis and stapes fixation. In 1980, Perkins5 introduced the laser for stapes surgery, which allowed the surgeon to vaporize the stapes footplate without instrumentation. Stapedotomy could be performed on a mobilized footplate, reducing the danger of a floating footplate. Stapes mobilization procedures have been largely abandoned because of the possibility of refixation of the stapes. In 1969, Rosen and Siegal6 studied the long-term results of 154 patients who had undergone a stapes mobilization procedure, yielding a 42% complete closure of the air bone gap and 32% closure within 10 dB at 4 years. Myers et al’s7 report of a 50-year-old man who had a mobilization procedure done 7 years before his death supports the theory that the footplate does not refix. On histologic examination, a fibrous union to a normal and mobile footplate was noted without evidence of otosclerosis, despite extensive otosclerosis elsewhere.7 Thus, it can be assumed that even if there is a significant amount of otosclerosis at the fissula ante fenestram, a linear defect across an uninvolved footplate should heal with a fibrous union. In 1998, Silverstein8 reintroduced the concept of partial stapedotomy surgery for otosclerosis without the use of a prosthesis. It can be performed when stapes fixation is localized to a focus of otosclerosis at the fissula ante fenestram. A linear laser stapedotomy at the anterior one third of the footplate with vaporization of the anterior stapes crus allows the stapes to become mobile while allowing stapes and stapedius tendon preservation with avoidance of the need for a prosthesis. The success of the laser STAMP procedure depends on the proper selection of patients. A candidate should have a blue footplate free of otosclerosis, except for the area adjacent to and involving the fissula ante fenestram. These characteristics can be assessed only at the time of surgery after entering the middle ear. Interestingly, it is difficult to predict candidacy based solely on preoperative audiogram. Rather, the patient is prepared for the possibility of laser STAMP versus conventional stapedotomy with prosthesis insertion. The surgeon should be prepared to do a stapedotomy with prosthesis, if the stapes is not completely mobilized after isolating the posterior two thirds of the stapes. If hearing should deteriorate in the future, the patient should be informed that a stapedotomy with prosthesis can be performed. Standard stapes surgery setup and patient positioning is used. One percent lidocaine with adrenaline 1:100,000 is injected subcutaneously into the external auditory canal. A tympanomeatal flap is elevated in the standard fashion. A portion of the scutum is removed with a diamond bur while preserving the chorda tympani nerve, thus providing a good view of the horizontal facial nerve and stapes. The stapes is inspected and palpated to determine if the otosclerosis is localized to the fissula ante fenestram. If the patient is confirmed to be a laser STAMP procedure candidate, the laser endoprobe hand piece with the HGM argon laser (Lumenis Ltd., Yokneam, Israel) is used to vaporize the anterior crus of the stapes using 2.0 W at 0.2-second duration. Routinely, the metal laser probe tip is bent to a 30-degree angle using a small hemostat without breaking the laser fiberoptic cable, to create the proper angle for vaporizing the anterior crus (Fig. 17–1). By direct vision, palpation with the tip of the laser probe, or visualization with a 30-degree, 1.7-mm-diameter otoendoscope, the anterior crus is cut by placing the laser probe tip against the crus (Fig. 17–2). A 1.5-mm right-angle pick or the fiberoptic laser tip is passed through the area of the anterior crus to document complete transection of the crus. FIGURE 17–1 Vaporizing the anterior crus. Next, the thin blue footplate is vaporized in a linear fashion across the anterior one third of the footplate (Fig. 17–3). The laser is set from 0.8 to 1.0 W at 0.2-second duration with at least 3-second pauses between laser bursts to prevent overheating the perilymph, which can cause transient vertigo for up to several days after the surgery. Small picks are used to be sure there is complete transection of the footplate and that the posterior two thirds of the footplate is completely mobile. If fixation has occurred because of otosclerosis at the fissula ante fenestram, and there is a blue footplate free of otosclerosis, the stapes should become completely mobile. After laser vaporization of the linear stapedotomy, there should be a half-millimeter separation between the fixed anterior one third and movable posterior two thirds of the footplate. A 2 × 3 mm piece of ear lobe adipose tissue is placed over the footplate to seal the perilymph space (Fig. 17–4). The most difficult part of the procedure is the transection of the anterior crus when it cannot be directly visualized with a microscope. Use of a 20-gauge CeramOptic probe (Ceramoptics, Naas, Ireland) with a 200-μm fiber that is bent to a 30-degree angle by the surgeon makes this part of the procedure easier. More bony exposure may be needed than with a traditional stapedotomy to manipulate the probe tip onto the anterior crus. One should be able to visualize the tympanic portion of the facial nerve and the pyramidal eminence prior to attempting to laser. Before vaporization, the anterior crus should be palpated with the laser probe. The probe tip can be inserted between the incus and the malleus handle over the horizontal portion of the facial nerve, or from inferiorly over the promontory of the cochlea. FIGURE 17–2 Cut the anterior crus.
LASER STAPEDOTOMY MINUS PROSTHESIS (LASER STAMP) AND OTHER MINIMALLY INVASIVE OTOLOGIC PROCEDURES
PROCEDURE ROOM SETUP AND EQUIPMENT
ANESTHESIA
LASER STAPEDOTOMY MINUS PROSTHESIS (LASER STAMP)
HISTORY
INDICATIONS
SURGICAL TECHNIQUE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree