CHAPTER 44 Radiology of the Nasal Cavity and Paranasal Sinuses
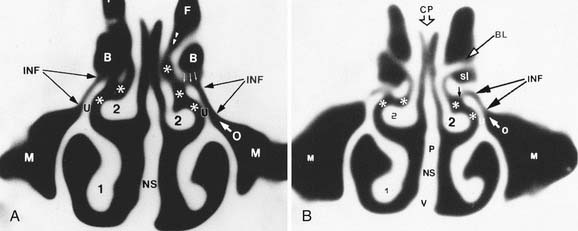
Radiologic examination of the sinuses is designed to give information that is complementary to clinical findings. Traditionally, conventional radiography was used to examine the paranasal sinuses. The standard radiographic sinus series consists of four views: lateral view, Caldwell’s view, Waters’ view, and submentovertex or base view.1 The lateral view shows the bony perimeter of the frontal, maxillary, and sphenoid sinuses. Caldwell’s view (Fig. 44-1) shows the bony perimeter of the frontal sinus. Waters’ view (Fig. 44-2) shows the outlines of the maxillary sinuses, some of anterior ethmoid air cells, and the orbital floors. The submentovertex view evaluates the sphenoid sinus and the anterior and posterior walls of the frontal sinuses.
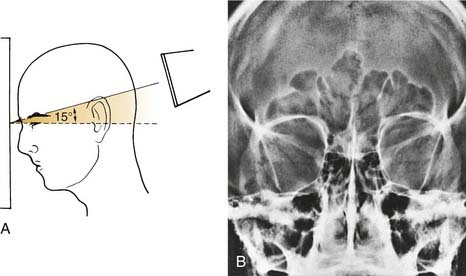
Figure 44-1. The modified Caldwell view. A, Positioning diagram. B, Sample radiograph.
(From Som PM, Curtin HD. Head and Neck Imaging. 3rd ed. St Louis: 1996; Mosby.)
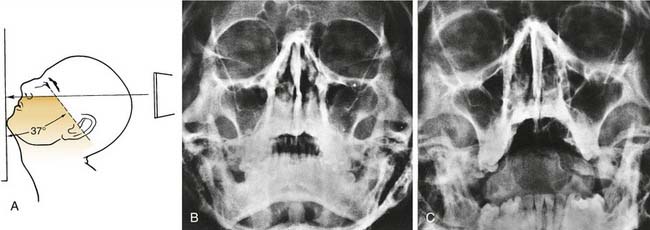
Figure 44-2. The modified Waters view. A, Positioning diagram. B, Sample closed-mouth radiograph. C, Sample open-mouth radiograph.
(From Som PM, Curtin HD. Head and Neck Imaging. 3rd ed. St Louis: 1996; Mosby.)
Standard radiography may be accurate in showing air and fluid levels in the frontal, maxillary, and sphenoid sinuses, but it significantly underestimates the degree of chronic inflammatory disease present, particularly in the ethmoid sinuses. Furthermore, the superimposition of fine bony structures on standard radiography precludes the accurate evaluation of the anatomy of the ostiomeatal channels.2–7
Computed Tomography
Computed tomography (CT) is currently the modality of choice in the evaluation of the paranasal sinuses and adjacent structures.2–7 Its ability to optimally display bone, soft tissue, and air facilitates accurate depiction of anatomy and extent of disease in and around the paranasal sinuses.2–57 In contrast to standard radiography, CT can clearly show the fine bony anatomy of the ostiomeatal channels.
Many writers stress the importance of initially performing CT after a course of adequate medical therapy to eliminate changes of mucosal inflammation and to better evaluate the underlying anatomic structures. To minimize mucosal edema and allow an improved display of the fine bony architecture, some writers also suggest routine management with a sympathomimetic nasal spray before scanning to reduce nasal congestion.8
Technique
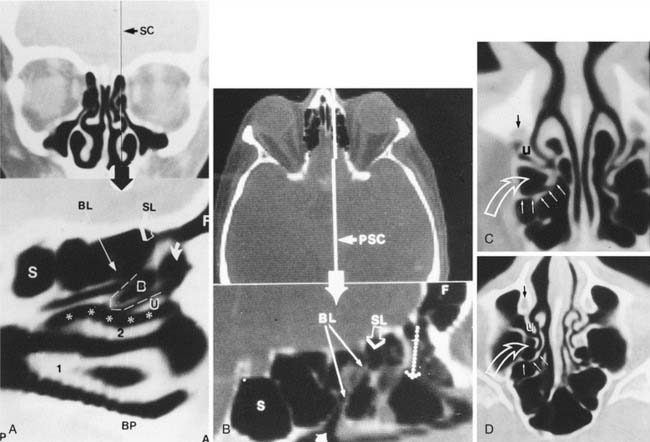
Because the coronal plane optimally shows the ostiomeatal unit, the relationship of the brain and ethmoid roof, and the relationship of the orbits to the paranasal sinuses, coronal reconstructions are routinely performed (Fig. 44-3).2–7 Coronal images correlate best with the surgical approach.9 Axial images are complementary to the coronal reformatted images when severe disease is present in the sphenoid and posterior ethmoid sinuses and surgical management is contemplated. Axial images can be helpful in displaying the position of the internal carotid arteries and optic nerves with respect to the bony margins of the posterior ethmoid and sphenoid sinuses, as well as in demonstrating the sphenoethmoid recess. Sagittal reconstructions can be obtained for a morphologic orientation. Various distances and angles can be measured to aid in the passage of instruments during surgery. The frontal recess is best visualized on the sagittal images.
If multi-slice multi-channel CT is not available, scanning is routinely performed in the coronal plane from the anterior wall of the frontal sinus through the posterior wall of the sphenoid sinus. Contiguous 3-mm-thick images are obtained. Scanning with contiguous images is important to avoid loss of information through “skipped” areas.10
Windows are chosen to highlight the air passages, the bony detail, and the soft tissues. A window width of 2000 Hounsfield units with a level of 200 Hounsfield units is the most advantageous.2–57
Radiation Exposure
See Chapter 11 for a general discussion of radiation exposure and CT scanning. Radiation-induced cataracts and thyroid cancer are the two specific concerns for paranasal sinus CT examinations. Imaging in the axial plane compared with the coronal plane results in a substantial reduction of radiation exposure to both of these structures. The average dose from a routine paranasal sinus CT examination is substantially less than the acute threshold dose of 0.5 to 2 Gy for detectable lens opacities, although the pediatric lens is more susceptible to radiation and the cumulative effects of radiation exposure to the lens is not well understood. A cumulative dose as small as 0.25 Gy can cause cataracts in children. The risk of thyroid malignancy from sinus CT examination is very low because the gland is not directly irradiated as it is with neck CT, but this small risk cannot be ignored. Furthermore, the dose received by the thyroid gland is substantially higher in young children, simply because the distance between the scanned region and the thyroid is less than in older children. In summary, a small but real risk of cataract and thyroid malignancy is associated with sinus CT examinations, particularly for children who undergo repeat studies.
Magnetic Resonance Imaging
Although magnetic resonance imaging (MRI) better visualizes soft tissue than CT,2,3 it does not visualize cortical bone. Because cortical bone and air have no mobile protons, they yield no MRI signal, resulting in an inability to discern the intricate anatomic relationships of the sinuses and their drainage portals. Thus, MRI is not a reliable operative road map to guide the surgeon during functional endoscopic sinus surgery (FESS).
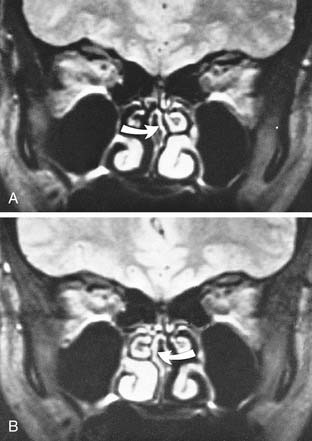
The side-to-side cyclic variation in the thickness of the nasal mucosa is known as the nasal cycle (Fig. 44-4). The signal intensity of the mucosal lining of the nasal cavity and the ethmoid sinuses varies with the nasal cycle.11,12 During the edematous phase of the nasal cycle, the mucosal signal intensity on T2-weighted MR images in these two areas appears similar to that of mucosal inflammation,5,8 limiting the usefulness of MRI (see Fig. 44-2). Interestingly, cyclic variation of the mucosal signal does not occur in the frontal, maxillary, or sphenoid sinuses. Increased mucosal thickness and higher signal intensity on T2-weighted images are always abnormal.11,12
With respect to sinus imaging, MRI has proved most helpful in the evaluation of regional and intracranial complications of inflammatory sinus disease and their surgical management, in the detection and staging of neoplastic processes, and in improved display of anatomic relationships between the intraorbital and extraorbital compartments. For example, MRI is helpful in diagnosing fungal concretions, which often show low or no signal on T2-weighted images.13–16 MRI also is useful in the evaluation of mucoceles and cephaloceles.17
Ostiomeatal Unit and Sinus Physiology
The mucosal lining of the paranasal sinuses is made up of a ciliated cuboidal epithelium. In turn, a mucous blanket is found on the surface. The cilia are in constant motion and act in concert to propel the mucus in a specific direction. The pattern of flow is specific for each sinus and will persist even if alternative openings are surgically created in the sinus.18–21 Therefore, FESS has gained widespread acceptance because it restores drainage of the sinuses through their anatomic drainage pathways.
In the maxillary sinus, the mucus flow originates in the antral floor, with the flow being directed centripetally toward the primary ostium. This pattern of mucus movement persists even after a nasal antrostomy is created.18,20,22–26
In the frontal sinus, mucus flows up along the medial wall, laterally across the roof, and medially along the floor. As the flow approaches the medial aspect of the floor, some mucus is directed into the primary ostium while the remainder is recirculated. The cleared mucus travels down the frontal recess and into the middle meatus, where it joins the flow from the ipsilateral maxillary sinus.18,20,23–26
Normal Anatomy
An understanding of the anatomy of the lateral nasal wall and its relationship to adjacent structures is essential (Fig. 44-5).6,27,28 The lateral nasal wall contains three bulbous projections: the superior, middle, and inferior turbinates (conchae). The turbinates divide the nasal cavity into three distinct air passages: the superior, middle, and inferior meati. The superior meatus drains the posterior ethmoid air cells and, more posteriorly, the sphenoid sinus (through the sphenoethmoidal recess). The middle meatus receives drainage from the frontal sinus (through the frontal recess), the maxillary sinus (through the maxillary ostium and subsequently the ethmoidal infundibulum), and the anterior ethmoid air cells (through the ethmoid cell ostia). The inferior meatus receives drainage from the nasolacrimal duct.
On CT, the first coronal images display the outline of the frontal sinuses (Fig. 44-6). The frontal sinuses are funnel-shaped. Their aeration varies among patients. They can be small and occupy only the diploic space of the medial frontal bone, or they can be large and extend through the floor of the entire anterior cranial fossa posteriorly to the planum sphenoidale. In general, a central septum separates the left and right sides; however, several septa are often present. The floor of the frontal sinus slopes inferiorly toward the midline.
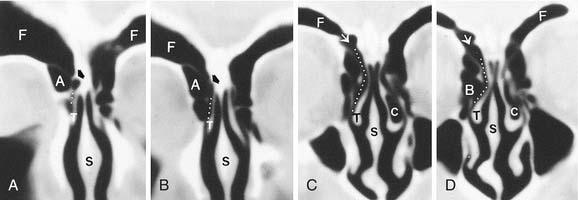
Close to the midline, the primary ostium is located in a depression in the floor. The frontal recess is an hourglass-like narrowing between the frontal sinus and the anterior middle meatus through which the frontal sinus drains (Fig. 44-7).4
The uncinate process is a superior extension of the lateral nasal wall (medial wall of the maxillary sinus).3,4 Anteriorly, the uncinate process fuses with the posteromedial wall of the agger nasi cell and the posteromedial wall of the nasolacrimal duct. The uncinate process has a free (unattached) superoposterior edge. Laterally, this free edge delimits the infundibulum (Fig. 44-8), the air passage that connects the maxillary sinus ostium to the middle meatus. Posterior to the uncinate is the ethmoid bulla, usually the largest of the anterior ethmoid cells. The uncinate process usually courses medial and inferior to the ethmoid bulla. The ethmoid bulla is enclosed laterally by the lamina papyracea.
The gap between the ethmoid bulla and the free edge of the uncinate process defines the hiatus semilunaris. Medially, the hiatus semilunaris communicates with the middle meatus, the air space lateral to the middle turbinate.3,4 Laterally and inferiorly, the hiatus semilunaris communicates with the infundibulum, the air channel between the uncinate process and the inferomedial border of the orbit. The infundibulum serves as the primary drainage pathway from the maxillary sinus.3,5
In most individuals, the posterior wall of the ethmoid bulla is intact, and an airspace is usually found between the basal lamella and the ethmoid bulla. This airspace is called the retrobullar recess or suprabullar recess, depending on its extent, and usually drains to the frontal recess (Fig. 44-9). Dehiscence or total absence of the posterior wall of the ethmoid bulla is common and can provide communication between these two usually separated airspaces.
The posterior ethmoid sinus consists of air cells between the basal lamella and the sphenoid sinus. The number, shape, and size of these air cells vary significantly among individuals.2,4,5,29
The sphenoid sinus is the most posterior sinus. It is usually embedded into the clivus and bordered superoposteriorly by the sella turcica. Its ostium is located medially in the anterosuperior portion of the anterior sinus wall, which in turn communicates with the sphenoethmoidal recess into the posterior aspect of the superior meatus. The sphenoethmoidal recess lies just lateral to the nasal septum and can sometimes be seen on coronal images but is best seen in the sagittal and axial planes (Fig. 44-10).2–3
The relationship between the aerated portion of the sphenoid sinus and the posterior ethmoid sinus must be accurately represented so the surgeon can avoid operative complications. Usually in the paramedian sagittal plane, the sphenoid sinus is the most superior and posterior airspace. More laterally, the sphenoid sinus is located more inferiorly, and the posterior ethmoid air cells become the most superior and posterior airspace. This relationship is well seen on axial and sagittal images. The number and position of the septa of the sphenoid sinus vary. Some septa can adhere to the bony wall covering the internal carotid artery, which frequently penetrates the sphenoid sinus.30
Anatomically, the paranasal sinuses are in close proximity to the anterior cranial fossa, the cribriform plate, the internal carotid arteries, the cavernous sinuses, the orbits and their contents, and the optic nerves as they exit the orbits.31–35 The surgeon should be cautious when maneuvering instruments in the posterior direction to avoid inadvertent penetration and drainage of these structures.3,7,33,34
Anatomic Variations and Congenital Abnormalities
Although the nasal anatomy varies significantly among individuals, certain anatomic variations are common in the general population and are often seen more frequently in patients with chronic inflammatory disease. The significance of an anatomic variant is determined by its relationship to the ostiomeatal channels and nasal air passages. The ability of the variation to obstruct the air passages may imply a role in the development and recurrence of sinusitis, although such a causal relationship has never been documented. The most common variations are discussed in the following paragraphs.10,27,28,37–40
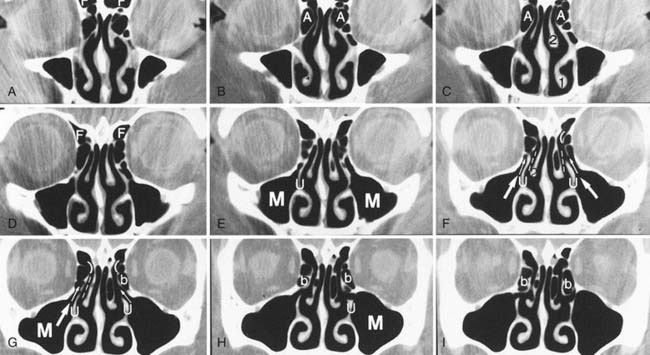
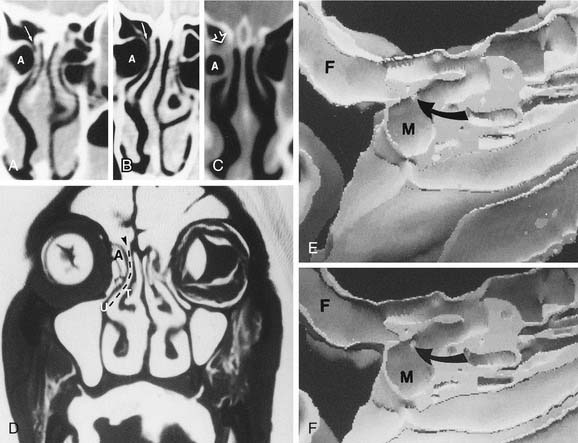
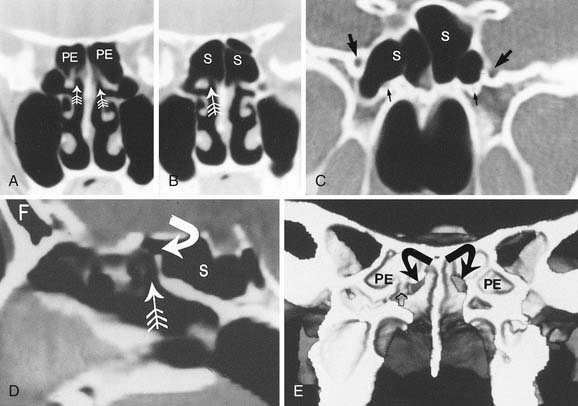
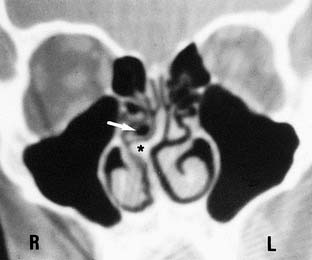
Concha Bullosa
Concha bullosa is defined as an aeration of the middle turbinate (Fig. 44-11). It may be unilateral or bilateral. Less frequently, aeration of the superior turbinate can occur, whereas aeration of the inferior turbinate is uncommon. A concha bullosa in the middle turbinate may enlarge to obstruct the middle meatus or the infundibulum. The air cavity in a concha bullosa is lined with the same epithelium as the rest of the nasal cavity; thus, these cells can undergo the same inflammatory disorders experienced in the paranasal sinuses. Obstruction of the drainage of a concha bullosa can lead to mucocele formation.
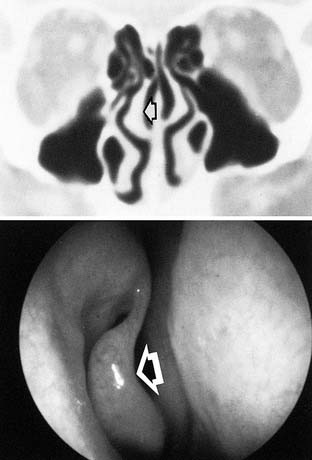
Nasal Septal Deviation
Nasal septal deviation is an asymmetric bowing of the nasal septum that may compress the middle turbinate laterally, narrowing the middle meatus (Fig. 44-12). Bony spurs are often associated with septal deviation, which may further compromise the ostiomeatal unit. Nasal septal deviation is usually congenital but may be a posttraumatic finding in some patients.
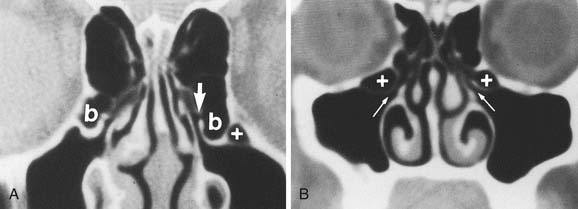
Paradoxic Middle Turbinate
The middle turbinate usually curves medially toward the nasal septum. However, its major curvature can project laterally and, thus, narrow the middle meatus and infundibulum. This variant is called a paradoxic middle turbinate (Fig. 44-13). The inferior edge of the middle meatus can assume various shapes with excessive curvature, which in turn can obstruct the nasal cavity, infundibulum, and middle meatus.
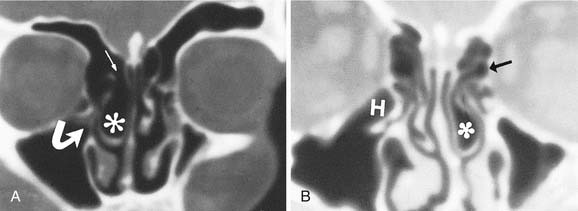
Variations in the Uncinate Process
Sometimes, the free edge of the uncinate adheres to the orbital floor or the inferior aspect of the lamina papyracea, which is termed an atelectatic uncinate process (Fig. 44-14). This variant is usually associated with a hypoplastic, and often opacified, ipsilateral maxillary sinus resulting from closure of the infundibulum. It is important to note this variant in the planning for surgery because there is an increased risk of orbital penetration when it is present.
Haller or Infraorbital Cells
Infraorbital cells are ethmoid air cells that extend along the medial roof of the maxillary sinus (Fig. 44-15). Their appearance and size vary. Large Haller cells may cause narrowing of the infundibulum. These cells may exist as discrete cells or may open into the maxillary sinus or infundibulum.