Preoperative CT Evaluations and Their Influence in Surgical Planning
High-resolution computed tomography (CT) continues to play a pivotal role in temporal bone imaging in general and in diagnosis of a cholesteatoma in particular. Preoperative CT scans can depict the anatomy of the middle ear and mastoid, and accurately predict the involvement of the sinus tympani and facial recess in cases of cholesteatoma.11 In addition, CT scanning has excellent spatial resolution, allowing delineation of small soft tissue masses against bony structures, and air, and can be a useful tool in the diagnosis of attic cholesteatoma.12 However, CT of the temporal bones is mostly performed when the ear is inflamed, and CT has been demonstrated to have poor value in distinguishing a cholesteatoma from the inflammatory tissue, granulations, fibrosis, or mucoid secretions in 20% to 70% of cases with opacification of the middle ear and mastoid.13–20 This is the main reason that it is sometimes impossible to diagnose or exclude the presence of a cholesteatoma or to predict the extension of the disease on the basis of CT findings alone, and why there is a little or no benefit of CT in managing these patients. Aoki15 reported that there was the need in transmastoid antrostomy to achieve complete removal of the cholesteatoma in only 6 out of 24 patients, whose preoperative CT scans demonstrated shadowing of the epitympanum, antrum, and mastoid air cells. Total resection of the cholesteatoma was possible by transcanal atticotomy combined with the use of a rigid endoscope in the other 18 patients. ▶ Fig. 6.1 and ▶ Fig. 6.2 depict the cases of retraction pocket cholesteatoma (RPC) correctly diagnosed by CT and operated purely endoscopically. These patients presented with a retraction pocket filled with a small cholesteatoma and a “dry” ear, and there was no need for additional imaging for surgical technique planning and appropriate patient counseling. In contrast, ▶ Fig. 6.3 portrays a case in which the coronal CT scan indicated that it would be possible to remove the cholesteatoma transmeatally by means of an endoscope, while axial images showed relatively large opacification in the mastoid. In retrospect this was due to the mild inflammation associated with the cholesteatoma, and the entire lesion was ultimately accessible and excised by endoscope alone. In some cases of partial or complete opacification of the middle ear and mastoid when the cholesteatoma cannot be distinguished from the reactive changes but it is actually possible to eradicate it solely by EES, magnetic resonance imaging (MRI) can provide essential information on the extension of the lesion and be used in planning a minimally invasive transmeatal endoscopic approach (▶ Fig. 6.3).
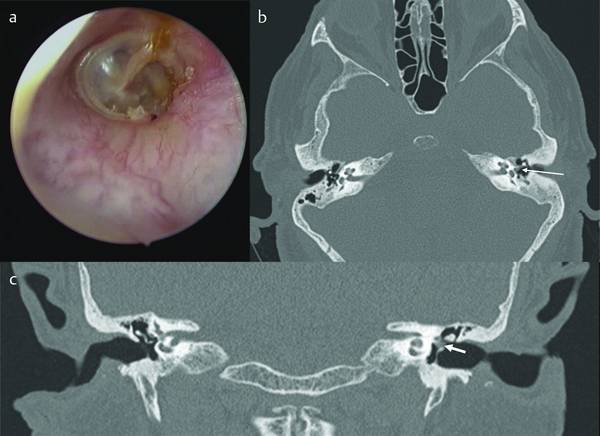
Fig. 6.1 a–c Retraction pocket cholesteatoma (arrow) correctly diagnosed by CT and operated entirely endoscopically (case 1).
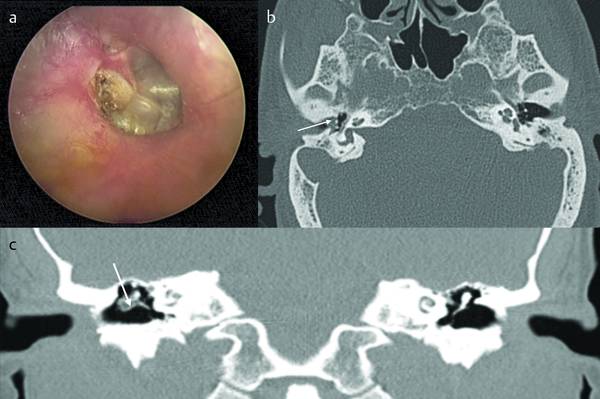
Fig. 6.2 a–c Retraction pocket cholesteatoma (arrow) correctly diagnosed by CT and operated entirely endoscopically (case 2).
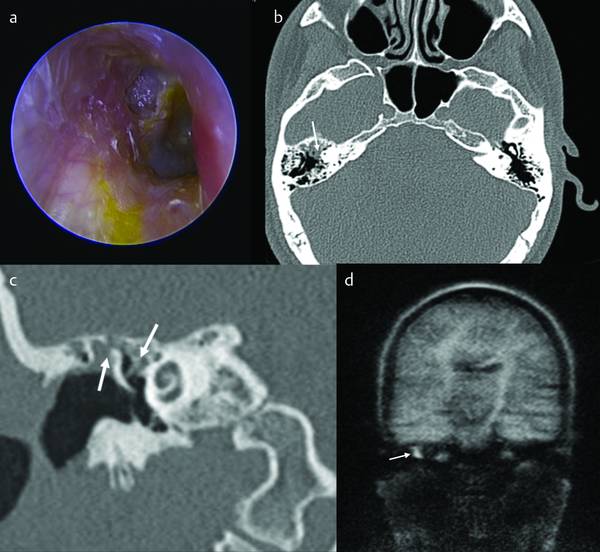
Fig. 6.3 In this case the coronal CT scan indicated that it would be possible to remove the cholesteatoma transmeatally by means of an endoscope (part c, the left arrow shows where the cholesteatoma starts, involving the epitympanum up to the geniculate ganglion area (right arrow), while axial images (b) showed relatively large opacification in the mastoid (arrow). In retrospect this was due to the mild inflammation associated with the cholesteatoma, and the entire lesion was ultimately accessible and excised by endoscope alone. The MRI appearance of the isodense tissue identified in the CT image (d).
6.2.1 The External Ear Canal
The dimensions of the external ear canal (external auditory canal; EAC) represent a fundamental consideration for endoscopic procedures. The practicability of the EAC for the procedure can be evaluated radiologically, in both axial and coronal CT scans. It is difficult to stipulate any definite cut-off of dimensions, since the suitability of the EAC should also be evaluated clinically. Irregularity or tortuosity can be better evaluated in preoperative endoscopy of the EAC by otoendoscopy and represent important information for the indication of an exclusively endoscopic approach. The surgeon must always consider the opportunity to drill the external ear canal, even endoscopically, to increase exposure of the surgical field in patients with small canals to facilitate surgical maneuvering.
6.2.2 Sinus Tympani
As already described in Chapter ▶ 4, the depth of the sinus tympani can vary, and this detail is very important because the deeper the sinus tympani the more difficult it is to achieve a radical removal of cholesteatoma. The clinical and radiological classification of the sinus tympani may help in preoperative surgical planning and in the choice of the approach (i.e., whether endoscopic or microscopic) (▶ Fig. 6.4). In particular, in HRCT scan axial slices, information about the sinus tympani depth can be obtained and classified as follows:
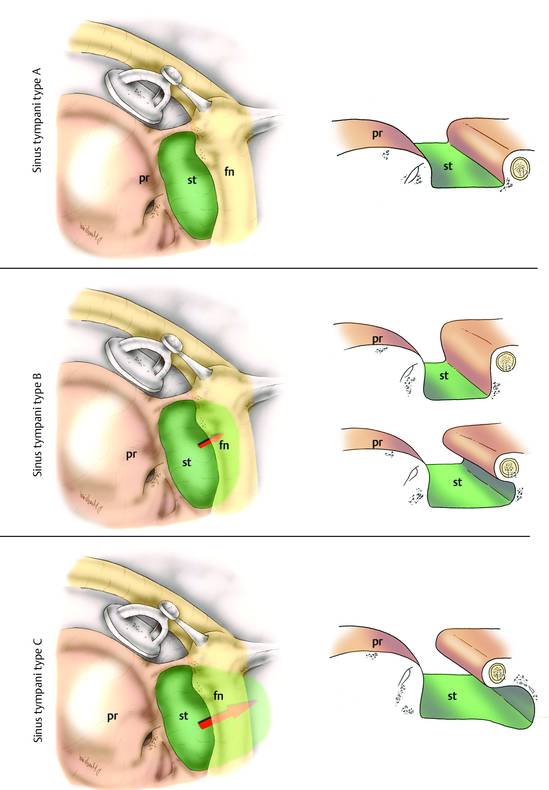
Fig. 6.4 The clinical and radiological classification of sinus tympani. pr, promontory; st, sinus tympani; fn, facial nerve.
Type A: (▶ Fig. 6.5) small sinus tympani. The medial limit of the third portion of the facial nerve corresponds to the depth of the sinus. In these cases, the sinus tympani is small and does not present a medial and posterior extension to the facial nerve.
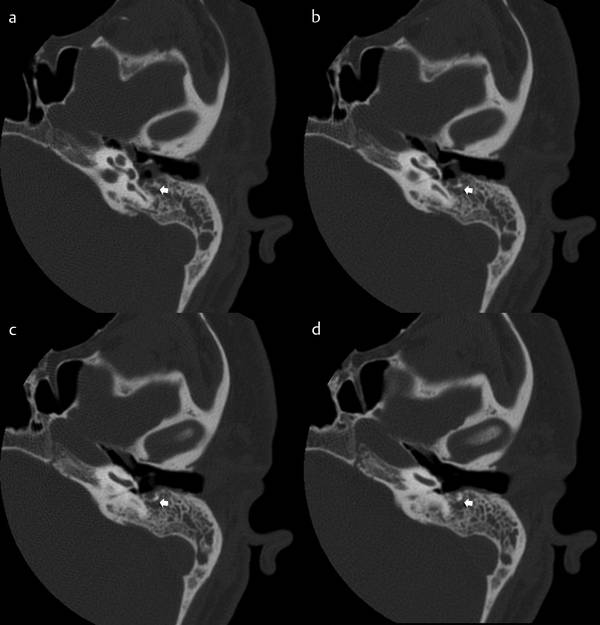
Fig. 6.5 a–d Small sinus tympani. The medial limit of the third portion of the facial nerve corresponds to the depth of the sinus (arrow). In these cases, the sinus tympani is small and does not present a medial and posterior extension to the facial nerve.
Type B: (▶ Fig. 6.6) deep sinus tympani. The medial boundary of the sinus tympani lies medially with respect to the third portion of the facial nerve and does not present a posterior extension to the facial nerve.
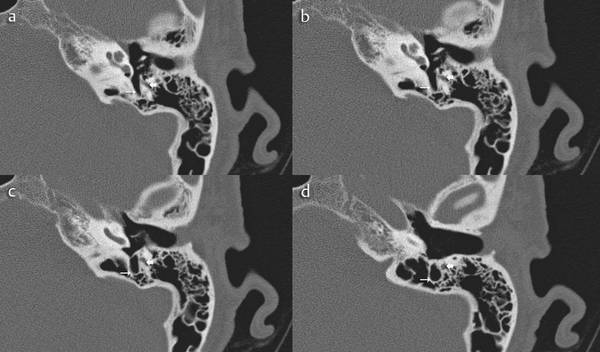
Fig. 6.6 a–d Deep sinus tympani (thin arrow). The medial boundary of the sinus tympani lies medially with respect to the third portion of the facial nerve (thick arrow) and does not present a posterior extension to the facial nerve.
Type C: (▶ Fig. 6.7) deep sinus tympani with posterior extension. The medial boundary of the sinus tympani lies medial and posterior to the third portion of the facial nerve. In these cases, the sinus tympani is very large and deep and all these patients have a well-developed mastoid.
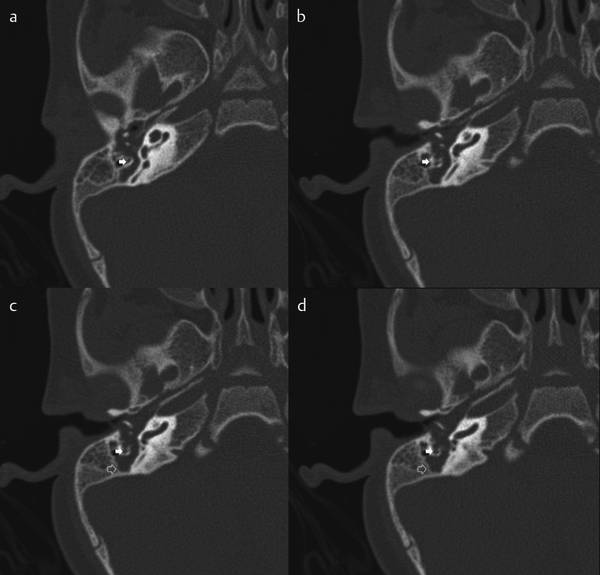
Fig. 6.7 a, b Deep sinus tympani with posterior extension. The medial boundary of the sinus tympani (open arrow) lies medial and posterior to the third portion of the facial nerve (solid arrow). In these cases, the sinus tympani is very large and deep and all these patients have a well-developed mastoid.
In our experience, the transcanal endoscopic approach is indicated in patients with sinus tympani types A and B. When the patient has a type C sinus tympani it is not possible to explore the entire depth of the sinus, even with the endoscope, especially when it is associated with well-developed mastoid cells. In these cases it may be necessary, when the site is involved by the pathology, to carry out a combined approach involving a microscopic retrofacial tympanotomy.
6.2.3 Antral and Mastoid Involvement
Some authors consider that cholesteatoma is endoscopically accessible when the lesion does not extend beyond the level of the lateral semicircular canal; although mastoid involvement may generally represent a contraindication to exclusively endoscopic approaches, improvements in instrumentation, diagnostics, and techniques are somewhat eroding these rules. In the case of mastoid involvement of the cholesteatoma, these authors would still recommend aborting endoscopic procedures in favor of microscopic techniques, to obtain adequate control of the mastoid extension of the pathology. In several selected cases, in the case of sclerotic mastoids and of antral or periantral involvement of cholesteatoma, removal can anyway be achieved exclusively endoscopically.21
Of course, the presence of a sclerotic mastoid is a fundamental prerequisite for endoscopic open tympanoplasty; we would not recommend performing an endoscopic open tympanoplasty in the case of well-pneumatized mastoids, since, in the absence of reconstruction, the air cells of the mastoids would have a blockage of ventilation due to the exclusion of the mastoid cavity from the middle ear cleft.
For this reason it is important to preoperatively stage the antral and periantral extension of cholesteatoma by CT, so as to preoperatively inform the surgeon of the feasibility of an exclusively endoscopic approach. This would clearly also be of importance in patient counseling. The antral and periantral involvement could influence not only the approach but also the technique, whether closed or open. Signs of antral and periantral involvement are the presence of isodense tissue in those regions, with significant bone erosion or mastoid cells (▶ Fig. 6.8, ▶ Fig. 6.9).
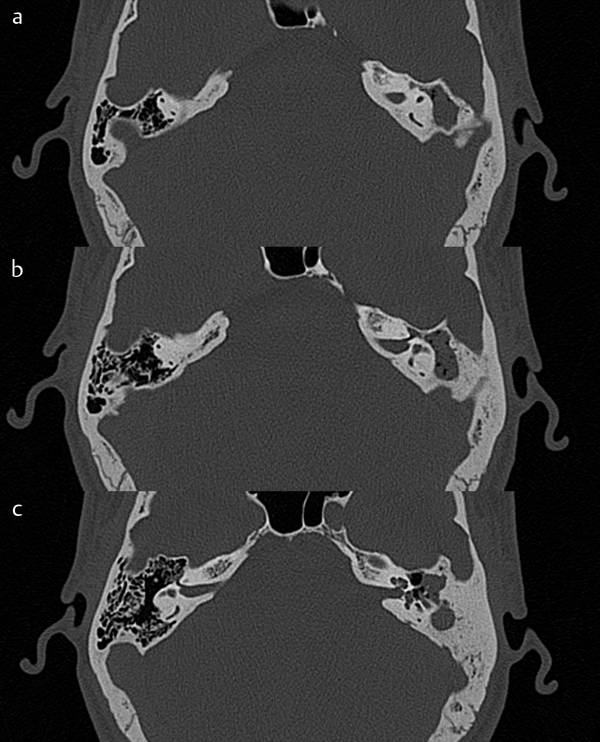
Fig. 6.8 a–c Left ear. Signs of antral and periantral involvement are the presence of isodense tissue in those regions, with significant bone erosion or mastoid cells.
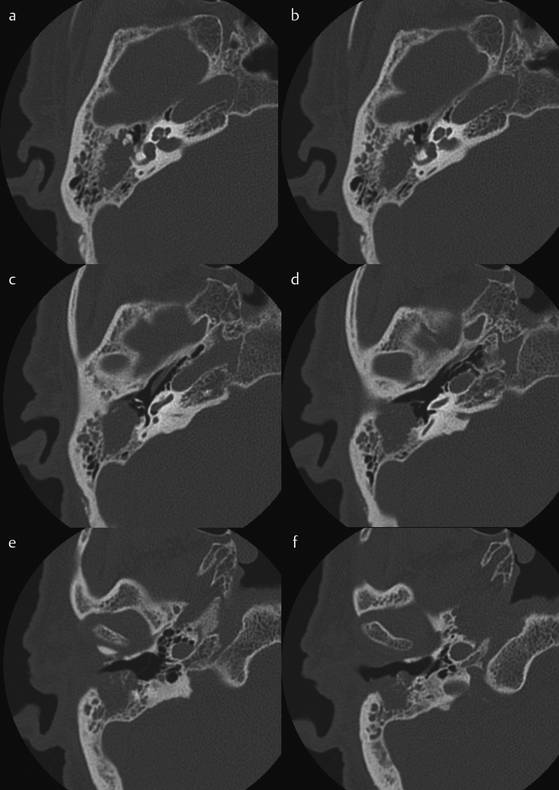
Fig. 6.9 a–f CT scan in axial view of cholesteatoma with mastoid involvement. In this case a microscopic approach is required.
6.2.4 Dural Plane Assessment
In the case of a low middle cranial fossa dura, access to the antrum will be increasingly difficult by classic canal wall down tympanoplasty in most cases, even to the extent of necessitating a higher displacement of the dura to obtain adequate visualization of the antral, periantral, and epitympanic region to remove the pathology.21 In contrast, in the case of a low middle cranial dura plane, the endoscope can allow a quite comfortable visualization of the most superior portion of the epitympanum without dural displacement.
Another characteristic of the dural plane that can be considered in evaluation of preoperative CT scans is the presence of tegmen dehiscence, which would represent a contraindication to endoscopic procedures since a two-handed technique would be necessary during surgical maneuvering for repair procedures (▶ Fig. 6.10).
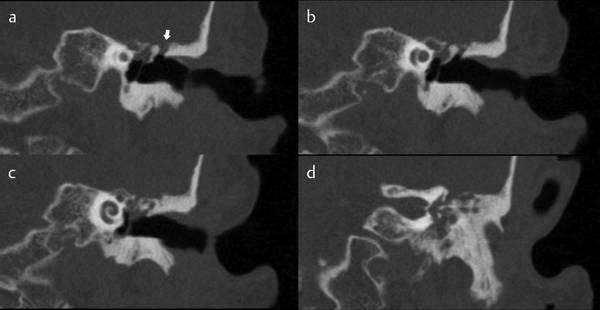
Fig. 6.10 a–d Coronal CT scan: tegmen dehiscence is present in a patient with a small attic (arrow).
6.2.5 Involvement of Subsites
The extent of cholesteatoma can be analyzed from the preoperative temporal bone CT scan. We stage cholesteatoma as follows (▶ Fig. 6.11, ▶ Fig. 6.12).22
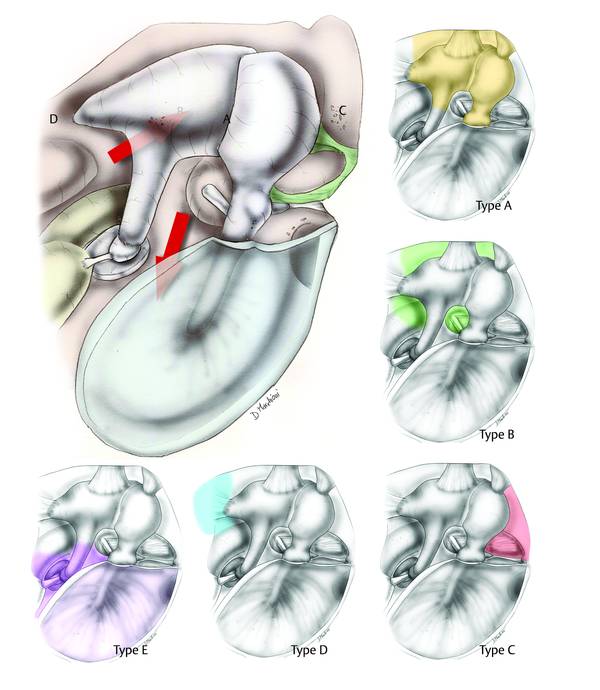
Fig. 6.11 Attic cholesteatoma staging based on subsite involvement.
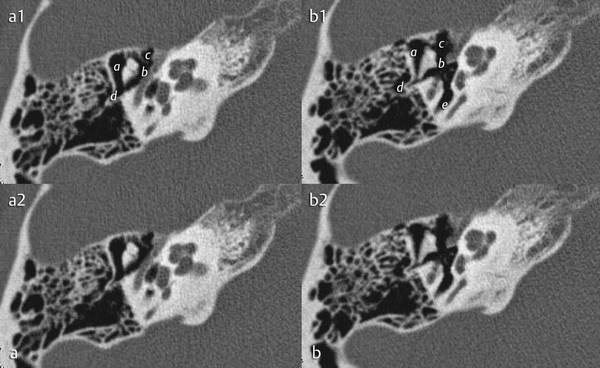
Fig. 6.12 a, b Attic cholesteatoma staging based on involvement of subsites a to e illustrated in two CT evaluations (a1,2 and b1,2).
Type A: Cholesteatoma involving the posterior lateral attic (the cholesteatoma lies between the lateral aspect of the incudomalleolar joint medially and the lateral bony wall of the attic).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


