Chapter 63 Pupil anomalies and reactions
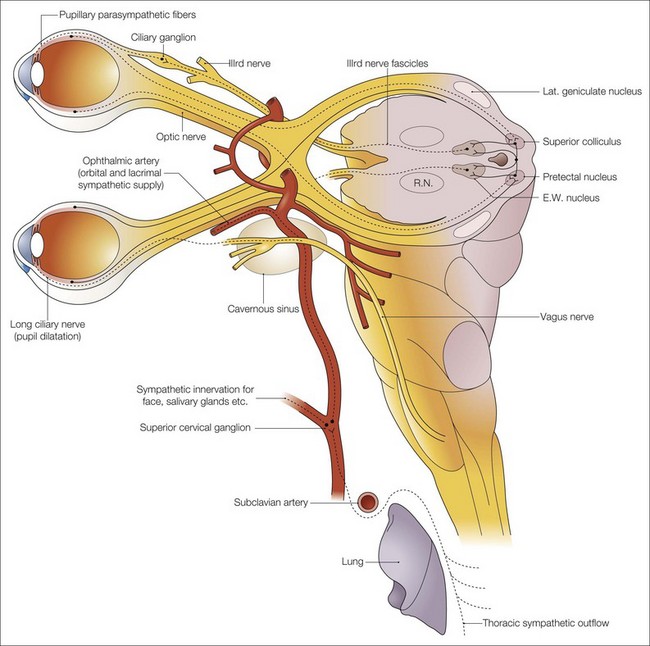
The anatomy (Fig. 63.1), physiology, and pathophysiology of the pupillary pathways are important to the pediatric ophthalmologist but they are dealt with so excellently elsewhere that only aspects relevant to children will be discussed here.
Development (see Chapter 2)
The pupillary light response is absent in infants of 29 gestational weeks or less, but is usually present by 31 or 32 weeks.1 At birth the pupil is small. It enlarges in the first months of life and is probably at its largest at the end of the first decade, gradually becoming miotic in old age. The pupil reactions of term or premature infants are often of small amplitude and, because of their small resting size, may be difficult to elicit clinically especially in infants with brown irises. The failure of the pupil grating response in infants under 1 month of age is further evidence of the immaturity of the pupil responses in infancy.2 Cocaine and hydroxyamphetamine are less potent in infants than in older children, suggesting that miosis of the newborn is due to decreased sympathetic tone.3 In very premature babies the pupil may not have fully formed; during the seventh month of gestation, the vascular pupillary membrane atrophies and the pupil appears. Before 32 gestational weeks, mydriasis should not be taken as necessarily indicating a central nervous system lesion and an unresponsive pupil does not necessarily indicate an afferent defect.3
Dynamic retinoscopy indicates that infants from 6 days to 1 month of age have no accommodation, but that normal function is achieved by 3 to 4 months.4 The effect of this is defocus of the higher spatial frequencies, the detection of which requires a greater discrimination than the younger infant is capable of. However, photorefraction studies have demonstrated an ability to accommodate of over 1 diopter in the neonate, and this increases rapidly in the first month and to a lesser extent in the first few years of life, with high amplitudes from 4 years onward until presbyopia sets in.
Congenital and structural abnormalities
Congenital, structural, and developmental anomalies in the pupil include the following (many are found in Chapters 32 and 38):
Afferent abnormalities of pupil reactivity
Afferent pupil defects
Relative afferent pupil defect
When one afferent pathway is affected, or if bilateral afferent pathways are affected asymmetrically, the relative afferent pupil defect (RAPD) in the afferent pupil pathway can be detected clinically with the “swinging flashlight” test (see video 106.1).5![]()
Testing for a RAPD
The presence of an RAPD is objective evidence for a defect in the afferent pathway from the retina to the optic tract and the intercalated neurons in the midbrain to the efferent pupil pathway. Although uncommon, a small RAPD may occur in deeply amblyopic eyes.6 In older children, a useful subjective addition to the test for the RAPD is to ask the child which eye sees the light brightest. The child may be asked a question, “if the light in the good eye is worth 1 pound/dollar how much is the other one worth?”, which may give a rough subjective quantification.
Efferent pupillomotor defects
Argyll Robertson pupils
In 1869, Douglas Argyll Robertson described a type of light−near dissociation seen classically with tertiary syphilis. The pupils are small, irregular, and constrict more fully and more briskly to a near stimulus than to light. The iris is often seen to be atrophic on slit-lamp examination. The lesion in the Argyll Robertson pupil is presumed to be located in the dorsal midbrain,7 and patients with such pupils should undergo serologic testing for syphilis.
Adie’s syndrome (tonic pupil syndrome)
Adie’s syndrome, unusual in young children, is typically idiopathic, but may occur with chicken pox or other viral infections,8 ophthalmoplegic migraine, and measles vaccination.9,10 It is more frequent in young female adults.11 It is usually unilateral but many cases become bilateral.11 Children rarely have symptoms related to the onset, but they may fail a school near vision test, or complain of blurred near or, if they are hyperopic, distant vision or photophobia. They may develop anisometropic amblyopia. Many patients are asymptomatic and parents may be the first to notice.
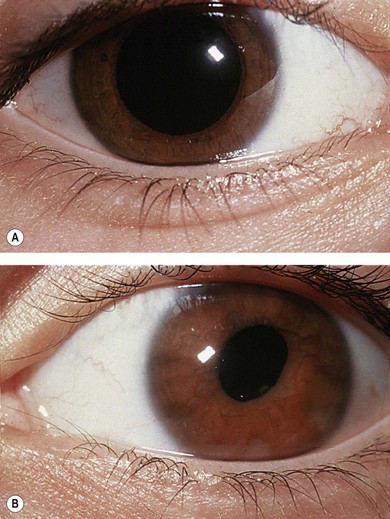
The acutely affected pupil is usually larger than the uninvolved eye (Fig. 63.2), but over time the Adie’s pupil tends to become miotic (“little old Adie”). There is typically a segmental paralysis of the iris sphincter which might be more extensive or diffuse. Once constricted, the pupil remains consticted longer (the “tonic” pupil). There may also be a transient defect in accommodation, which is often marked at first but gradually improves over 2 or more years.11 Corneal sensation may be reduced when tested with an aesthesiometer or even with a wisp of cotton, but is generally asymptomatic. This is probably due to damage to the trigeminal fibers that also pass through the ciliary ganglion. Patients with Adie’s pupil may also have hyporeflexia or areflexia in their extremities but no other neurologic findings are usually present. Although the Adie’s pupil is a clinical diagnosis, denervation hypersensitivity of the pupil may be demonstrated by finding pupillary constriction compared to the fellow eye 20 minutes after instillation of pilocarpine 0.0625%. Pharmacological hypersensitivity may occur with post- as well as pre-ciliary ganglionic lesions (Fig. 63.3).


Fig. 63.2 Left Adie’s pupil. (A) In light, (B) in dark. The pupil size difference is less in the dark.
Loewenfeld and Thompson proposed that the site of the lesion of the tonic pupil is in the ciliary ganglion and that many of its features can be explained by aberrant regeneration.12 The cause is unknown but it may be due to a neurotropic virus. Most patients do not require treatment, but they may be helped with their photophobia and occasionally with symptoms due to accommodation paresis by pilocarpine (0.1% three times daily) or another dilute miotic. In distinction to adult patients, young children with Adie’s or other tonic pupils should have the unaffected or better eye occluded for a short period each day to avoid amblyopia. Spectacle correction of hyperopia in the affected eye may be necessary to prevent anisometropic amblyopia.
Iris abnormalities
Damage to the iris by trauma, irradiation, uveitis, ischemia or hemorrhage, or involvement with a tumor such as lymphoma, leukemia, juvenile xanthogranuloma, leiomyoma, or neurofibroma, may all give rise to anisocoria, corectopia, and/or impaired pupil reactions (Fig. 63.4). Slit-lamp examination of the iris can demonstrate the disruption of the iris architecture from the underlying cause.
Benign episodic unilateral mydriasis (“springing pupil”)
The syndrome of idiopathic episodic mydriasis is likely a heterogeneous group of conditions that result in parasympathetic insufficiency of the iris sphincter or sympathetic hyperactivity of the iris dilator.13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree