Chapter 106 Prevention of Retinal Detachment
Introduction
Rhegmatogenous retinal detachment continues to be an important cause of reduced visual acuity and blindness. In consecutive series, initial surgical attempts to reattach the retina currently fail in approximately 10–20% of cases, and reoperations are unsuccessful in as many as 5% of cases.1–3 Anatomical success is significantly less common in consecutive series of eyes with features suggesting an increased risk of proliferative vitreoretinopathy (PVR).4 Following anatomically successful surgery, visual acuity returns to 20/50 or better in only approximately 50% of cases.5 Thus, the prevention of retinal detachment is a worthy goal, and a variety of prophylactic methods have been investigated since Jules Gonin, in 1920, first identified the pathogenesis and treatment of this previously incurable disorder. However, despite a long-standing interest in the ophthalmologic community regarding prophylactic therapy, there have been no optimal clinical trials to test the legitimate value of any form of preventive treatment.6–8
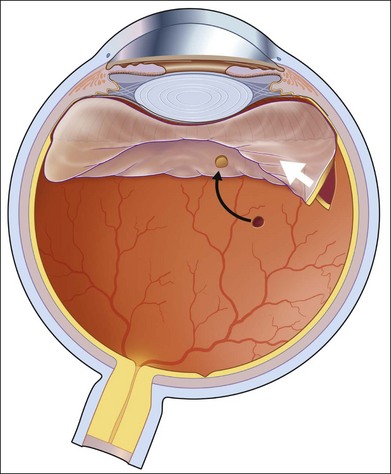
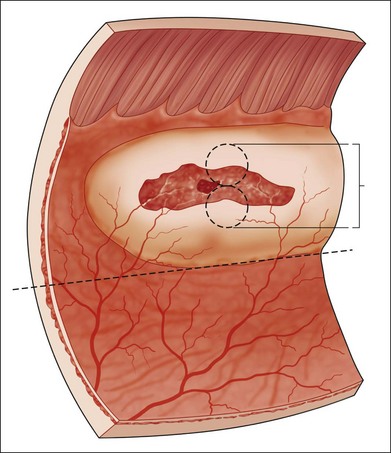
Vitreous liquefaction and a retinal break are prerequisites for rhegmatogenous retinal detachment, and the usual pathologic sequence is vitreous liquefaction followed by some degree of posterior vitreous detachment (PVD). This results in vitreoretinal traction at the site of a vitreoretinal adhesion and in the production of a retinal tear (Fig. 106.1). Alternatively, traction may be exerted upon areas of lattice degeneration containing atrophic retinal holes. Continued vitreoretinal traction near retinal breaks appears to be necessary to cause the vast majority of clinical retinal detachments. Thus, retinal detachment might be avoided by: (1) preventing vitreous liquefaction and associated PVD; (2) relieving vitreoretinal traction; or (3) creating a chorioretinal adhesion around vitreoretinal adhesions and retinal breaks.
No means are available to prevent vitreous liquefaction and later PVD in most eyes, although maintaining an intact posterior lens capsule after extracapsular cataract surgery may reduce or delay these changes.9,10 Vitreoretinal traction can be relieved by vitrectomy or by scleral buckling. However, prophylactic vitrectomy is not performed because there are technical difficulties in completely removing the peripheral vitreous gel, and it is relatively hazardous. Scleral buckling is only rarely employed, such as in particularly high-risk cases in which a nontraumatic giant retinal tear has already occurred in a fellow eye11 or in cases of posterior segment open globe injuries.12 Thus, the primary method of preventing retinal detachment involves the use of laser photocoagulation or cryotherapy to create a chorioretinal adhesion around both visible sites of vitreoretinal adhesion and retinal breaks. Although this is frequently successful in sealing the treated lesion and preventing it from causing a clinical retinal detachment, the genuine value of such therapy related to simple observation remains unclear in most situations, since most visible asymptomatic retinal breaks and vitreoretinal degenerative lesions do not cause retinal detachments. Instead, breaks causing detachment usually occur in regions of the peripheral retina that appear normal before PVD.6,7 In addition, relatively extensive prophylactic therapy may cause vitreous changes that actually increase the chances of subsequent vitreoretinal traction and retinal detachment.6,13
Risk factors for retinal detachment
In any eye with visible retinal breaks or vitreoretinal adhesive lesions that predispose to retinal detachment, a number of additional factors are considered to be associated with a relatively high risk of subsequent retinal detachment (Table 106.1). Symptoms and signs of acute PVD place an eye at particularly high risk. Additional factors include a variety of hereditary, congenital, acquired, and iatrogenic problems.
Table 106.1 Risk factors for rhegmatogenous retinal detachment
| Hereditary/congenital/developmental/degenerative Prior ocular surgery Prior ocular trauma Inflammatory Other Fellow-eye nontraumatic retinal detachment |
In evaluating the natural history or risk of retinal detachment in these cases, particular attention must be paid to the way in which both natural history and postoperative data, regarding a variety of retinal lesions, have been collected. The risk of retinal detachment is substantially different among subgroups of eyes, a fact that influences interpretation of both natural history data and treatment results. For example, since an acute PVD is the primary cause of most retinal detachments, and since most retinal tears occur during or soon after PVD, it is likely that eyes without a PVD have a higher risk of later retinal detachment than eyes with a history of prior PVD and no subsequent retinal breaks, regardless of additional risk factors.14 Similarly, vitreous liquefaction and PVD occur with greater frequency in older patients and in myopic and nonphakic eyes.15 Thus, data regarding lesions in otherwise normal, young, nonmyopic eyes are not comparable with data from cases with other risk factors that greatly increase the likelihood of PVD. Since more than one factor is often present, data analysis is difficult if all features are not recorded. For example, myopic aphakic eyes with lattice degeneration and with a history of retinal detachment in the fellow eye have a substantially greater risk of retinal detachment than otherwise normal eyes with lattice degeneration. No prospective randomized trials of therapy to prevent retinal detachment have been performed.6–8 The few published studies of treated and untreated comparable eyes have been retrospective, and most reports regarding prophylactic therapy have simply described results of a treatment series.
This chapter briefly discusses published outcomes regarding both the natural course of lesions that predispose an eye to retinal detachment and results of prophylactic therapy for these retinal breaks and vitreoretinal adhesive lesions. The topic of “subclinical retinal detachment” (for definition, see Fig. 106.4) will not be discussed as a separate entity because of the nonspecific nature of the term. This chapter distinguishes symptomatic from asymptomatic cases and is organized according to the type of retinal break or vitreoretinal adhesive disorder and also according to the presence of other high-risk factors. A brief discussion of treatment methods precedes the review of treatment results and complications.
Symptomatic eyes
Patients are considered symptomatic if they describe photopsia and/or increased vitreous floaters associated with an acute posterior vitreous detachment. Approximately 15% of eyes with a symptomatic PVD develop retinal tears of various types.16–18 The risk of retinal tears is directly related to the amount of vitreous hemorrhage associated with symptoms, and the finding of pigmented cells in the vitreous is a sign associated with a particularly high chance of associated retinal tear(s).19 In symptomatic eyes, retinal tears associated with persistent vitreoretinal traction are especially likely to cause retinal detachment, and the likelihood is even higher in cases with additional high-risk factors.
Retinal tears resulting from a symptomatic PVD should be distinguished from pre-existing retinal breaks detected after the PVD but not caused by it. Thus, atrophic retinal holes within areas of lattice degeneration are not considered “symptomatic,” even if they were first observed during an examination prompted by symptoms of an acute PVD. Symptomatic retinal tears are subdivided into those with persistent vitreoretinal traction and those in which all traction in the region of the retinal defect has disappeared (Fig. 106.1).
Tears with persistent vitreoretinal traction
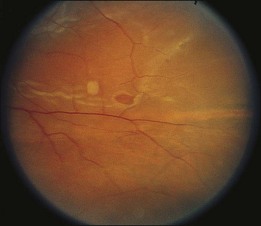
Most symptomatic tears with persistent vitreoretinal traction are horseshoe-shaped and have a high risk of causing clinical retinal detachment. Rarely, a retinal tear with a free operculum may have persistent vitreoretinal traction as a result of a residual vitreoretinal adhesion near the retinal break, most frequently at the location of a retinal blood vessel (Fig. 106.2).
Horseshoe-shaped tears
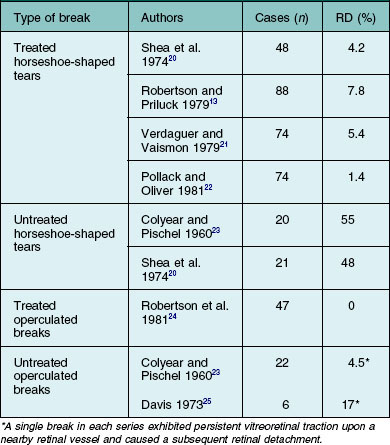
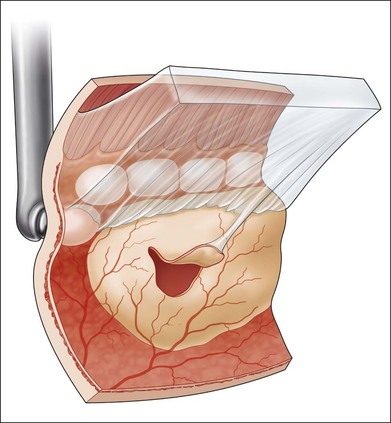
Untreated symptomatic retinal tears with persistent vitreoretinal traction have been reported to cause retinal detachment in 33–55% of cases (Table 106.2). Treatment of this type of break substantially reduces the risk of retinal detachment (Table 106.2),20 and immediate therapy for these lesions is indicated to prevent an accumulation of subretinal fluid.7,26 A chorioretinal adhesion is created in flat retina immediately adjacent to localized subretinal fluid (Fig. 106.3). Reviews of treatment techniques have been provided elsewhere in the literature,27 and these are briefly discussed later in this chapter.
Round tears
The percentage of operculated retinal tears that are associated with persistent vitreoretinal traction in the vicinity of the retinal break is unknown, but it is quite low. Only two symptomatic operculated retinal breaks have been reported to progress to retinal detachment, and both were associated with persistent vitreoretinal traction on a nearby retinal vessel.23,25 In unusual cases in which an operculated retinal hole is the only retinal break associated with a clinical retinal detachment, it is presumed that anomalous persistent vitreoretinal adhesions are located in the vicinity of the retinal tear (Fig. 106.2). Failures following treatment of operculated retinal holes have not been reported (Table 106.1).
Tears unassociated with persistent vitreoretinal traction
Symptomatic operculated retinal tears unassociated with persistent vitreoretinal traction in the vicinity of the retinal break have not been reported to progress to clinical retinal detachment (Table 106.1). Similarly, although large numbers of these breaks have been treated prophylactically, there are no reports in the literature of a treatment failure (Table 106.1). Treatment of this type of retinal break appears to be unnecessary unless the possibility of persistent vitreoretinal traction cannot be excluded.
Retinal holes and precursors of retinal detachment
Eyes with symptoms and signs of acute PVD frequently contain atrophic retinal breaks that are not due to acute vitreoretinal traction. For the purposes of this discussion, these lesions are considered to be pre-existing and not symptomatic.17 Similarly, precursors of retinal detachment, including lattice degeneration, cystic retinal tufts, and age-related retinoschisis, are managed as if they were originally discovered in asymptomatic eyes.
Asymptomatic eyes without high-risk factors
Vitreoretinal precursors of retinal breaks
Lattice degeneration
Lattice degeneration is present in approximately 30% of retinal detachments, and approximately 94% of these detachments occur in primary (nonfellow) eyes.6 Because lattice lesions are visible and occur in approximately 8% of the population, they have commonly been considered as candidates for prophylactic therapy. However, Byer’s natural history study of 276 patients and 423 involved eyes, followed an average of almost 11 years, indicated that lattice lesions in phakic nonfellow eyes were not particularly dangerous.28 At the end of the follow-up period, atrophic retinal holes were present in 150 (35%) eyes. Subclinical retinal detachments, defined as subretinal fluid extending more than one disc diameter (DD) from the break but not posterior to the equator (Fig. 106.4), were observed in ten of the eyes with holes. In six of these eyes, the subclinical detachment developed during the observation period, whereas four eyes exhibited the changes at the initial examination. Only one subclinical detachment was considered in need of treatment after a small asymptomatic posterior extension of subretinal fluid.
Four asymptomatic tractional retinal tears were observed in three of these 423 eyes at the initial examination, and symptomatic tractional tears without clinical detachment developed in five additional eyes during follow-up periods of 1.5–18 years.28 Three of five symptomatic and all asymptomatic breaks occurred adjacent to lattice lesions. All symptomatic breaks were successfully treated; no asymptomatic tractional tears were treated, and none changed over follow-up periods of 7, 10, and 15 years.
Clinical retinal detachments developed in three of the 423 eyes.28 Two were due to round retinal holes in lattice lesions of patients in their mid-20s, and one was due to a symptomatic tractional tear. These figures clearly indicate that patients with lattice degeneration in a phakic nonfellow eye should not be treated prophylactically unless symptoms occur. However, retinal detachments associated with vitreoretinal traction upon lattice lesions containing atrophic retinal holes are relatively common in eyes with significant amounts of myopia.29,30 A discussion regarding self-examination of peripheral visual fields and periodic follow-up examinations are in order in myopic patients to reduce chances of macular involvement by slowly progressive detachments resulting from round holes in lattice lesions.
Cystic retinal tufts
Retinal tears at sites of cystic retinal tufts may be responsible for as many as 10% of clinical retinal detachments associated with posterior vitreous detachment,31 and they are also associated with asymptomatic small horseshoe-shaped tears and minimal subretinal fluid in the absence of PVD.32 Byer31 calculated the chances of clinical retinal detachment in eyes with cystic retinal tufts to be one in 357, and these lesions are not worthy of prophylactic therapy in otherwise normal eyes.
Degenerative retinoschisis
Clinical retinal detachments occur in association with degenerative retinoschisis in up to 6% of consecutive detachment cases,33 and the presence of retinoschisis and outer layer breaks has sometimes been considered an indication for prophylactic therapy.34 However, a natural course study of 218 eyes in 123 patients demonstrated no clinical retinal detachments during a follow-up period averaging 9.1 years.33 The vast majority of small subclinical detachments that develop in association with outer layer breaks remain small, and prophylactic therapy is indicated only in the presence of obvious significant progression of subretinal fluid posterior to the equator.
Asymptomatic retinal breaks
In phakic nonfellow eyes, asymptomatic retinal breaks that are routinely discovered during an evaluation of the peripheral retina are extremely unlikely to lead to clinical retinal detachment, even if they are flap tears and even if posterior vitreous detachment occurs.35 During a follow-up period averaging 11 years, asymptomatic retinal breaks in 235 eyes of 196 patients were studied, and horseshoe-shaped tears were present in 45 cases. Acute PVD occurred in nine eyes without adversely affecting the pre-existing breaks, although new horseshoe-shaped tears developed in three cases, and these were promptly treated. Subclinical retinal detachments were observed in 19 (8%) eyes. Modest extension of subretinal fluid required therapy in two of these cases, and in a third case, a peripheral clinical retinal detachment slowly developed after 14 years of observation.
Prophylactic therapy for asymptomatic retinal breaks in phakic nonfellow eyes is usually not recommended. An occasionally observed exception to this rule is an inferior retinal dialysis. These breaks can cause slowly progressive retinal detachments that frequently become symptomatic only after macular involvement.36
Asymptomatic nonfellow eyes with high-risk factors
Myopic nonfellow eyes
Myopia is obviously associated with an increased risk of retinal detachment, and there is a direct correlation between amount of myopia and rate of retinal detachment.37 Lattice degeneration associated with retinal holes did not correlate with degree of myopia in the natural course study of Byer,28 although most slowly progressive clinical retinal detachments associated with lattice degeneration and an absence of extensive posterior vitreous detachment occur in young myopic patients,29,30 as noted above. There appears to be no increased value for treatment of myopic eyes with lattice degeneration in nonfellow eyes, and it is noteworthy that the small favorable effect of preventive treatment of lattice lesions in phakic fellow eyes could not be demonstrated if the degree of myopia exceeded 6 diopters.38
Asymptomatic retinal breaks are more common in myopic eyes than in emmetropic or hyperopic cases.5 However, clinical retinal detachments in these cases are rare in the absence of new symptoms, and prophylactic treatment is usually not advised in nonfellow eyes.
Aphakic and pseudophakic nonfellow eyes
Removal of the crystalline lens is associated with a substantial increase in the rate of later retinal tears and detachments,39 regardless of the method of cataract surgery, and this probably is due to vitreous changes in the nonphakic eye. An intact posterior lens capsule appears to be associated with a reduced rate of retinal detachment following cataract surgery, whereas Nd:YAG capsulotomy is clearly associated with an increased risk of subsequent detachment.9,10
Asymptomatic retinal breaks in nonfellow nonphakic eyes or eyes undergoing cataract surgery have sometimes been regarded as an indication for prophylactic therapy. However, Friedman et al.40 followed 18 retinal breaks in nonmyopic aphakic eyes for 3–7 years, and none detached. Hyams et al.41 studied 103 myopic aphakic eyes and discovered 25 asymptomatic retinal breaks in 19 eyes. Although six of the 25 were horseshoe-shaped tears, later retinal detachment occurred in no cases. More thorough reviews of the literature regarding the natural course of asymptomatic nonphakic retinal breaks and therapy for them have been published elsewhere,6,27 and there are not sufficient data to provide firm guidelines for management of asymptomatic retinal breaks in nonfellow eyes that are nonphakic or scheduled for cataract surgery. Treatment of horseshoe-shaped tears in these cases appears to be frequently recommended despite the lack of appropriate information in the literature.7,26
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree