Chapter 127 Pharmacology at Surgery
Pharmacologic vitreolysis
Rationale for pharmacologic vitreolysis
Posterior vitreous detachment (PVD) is a progressive physiological process, involving both syneresis (liquefaction) and synchysis (separation). However, spontaneous PVD is very often incomplete and remnants of the vitreous adhere firmly either to areas in the periphery of the retina or to the macular area in some conditions. Tractional forces exerted by vitreous collagen fibers and/or cellular proliferations at the vitreoretinal interface also play an important role in the pathogenesis of tractional maculopathies such as macular holes, vitreomacular traction syndrome or epimacular membranes. In addition, focal abnormal vitreoretinal adhesions may be implicated in certain types of diabetic macular edema and exudative age-related macular degeneration.1,2
Our present therapeutic approach in these tractional maculopathies is to relieve tractional forces surgically by mechanical means inducing a more or less complete PVD using suction exerted by the vitrectomy probe, followed by a removal of remnants of vitreous collagen fibers and cellular proliferations using endgripping forceps. As we have learned that cellular proliferations tend to recur using remnants of collagen at the internal limiting membrane (ILM) as a scaffold for cellular proliferation, most surgeons tend to remove the ILM during the surgical intervention as well, in order to remove all epiretinal tissue. However, it may be hypothesized that direct manipulation in the area of the macula and the removal of the ILM itself may somehow have an impact on function in the macular area or interfere with the morphological integrity of the retinal layers, especially when being removed with the aid of visualizing agents.3 Therefore, although ILM peeling appears safe from a clinical point of view, it may not be the optimum treatment option with regard to the best possible functional results.
Given this background, a pharmacological liquefaction of the vitreous gel and simultaneous enzymatic separation of vitreous fibrils from the inner aspect of the ILM may result in a resolution of focal vitreomacular adhesions, and this represents an alternative approach to treat traction-related retinal and macular diseases. Leaving the ILM in place and cleaving the vitreoretinal interface at the vitreal side of the ILM, may offer a more complete PVD, and be less traumatic as compared with vitrectomy. This pharmacologic induction of a PVD, if achieved early in the course of retinal or macular diseases, may have also a potential as a prophylactic treatment against advanced stages of potentially sight-threatening conditions such as diabetic retinopathy or AMD.4 This concept is referred to as “pharmacologic vitreolysis,” and was initially introduced by Sebag in 1998.5 Additional potential indications include vitreoretinal procedures for retinal detachment in children, in whom firm adherences of the vitreous often complicate surgery, especially in retinopathy of prematurity or ocular trauma with intraocular foreign body in young persons. The hope is to make vitreoretinal surgery procedures more safe and effective using the concept of pharmacologic vitreolysis.
The following substances have been evaluated or are currently under investigation.
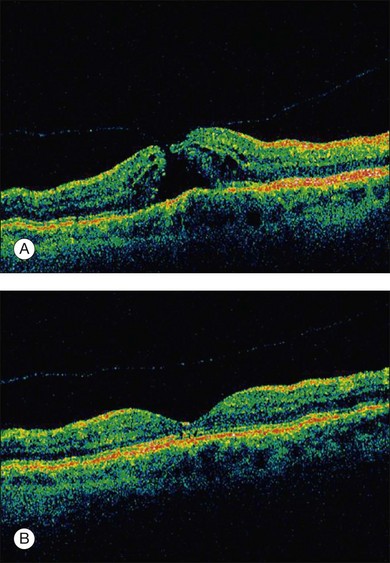
Enzymatic vitreolysis – microplasmin, plasmin, and others
Microplasmin
Microplasmin represents a recombinant protein that contains the catalytic domain of human plasmin but is much more stable as compared to the latter; both plasmin and microplasmin are nonspecific serine proteases cleaving a variety of glycoproteins such as fibronectin, laminin, fibrin and thrombospondin.6 These glycoproteins are involved in the adherence of the vitreous cortex to the ILM. Thus cleavage of these enzymes potentially induces a PVD: experimentally, microplasmin has been shown to increase vitreous diffusion coefficients in vitro using the non-invasive technique of dynamic light scattering7 and caused simultaneous vitreolysis and posterior vitreous separation in ex vivo and in vivo animal eye models in an apparent dose- and time-dependent fashion8,9 without morphological alterations in the retina.10 In a human, double-masked, Phase II trial 60 patients were randomized in four treatment cohorts either receiving increasing doses of microplasmin (75, 125, and 175 µg) or an initial injection of 125 µg followed by an injection of 125 µg if no release of adhesion occurred 1 month later or sham injection.11 The study revealed that within 28 days of sham, 75, 125, and 175 µg microplasmin administration, a nonsurgical resolution of vitreomacular adhesion was observed in 8, 25, 44, and 27% of patients; when the 125 µg dose was repeated up to 3 times, adhesion release was observed in 58% of patients 28 days after the final injection.11 Another phase 2, placebo-controlled, double-masked, dose-ranging clinical trial analyzed the effect of a single injection of microplasmin (25, 75, or 125 µg) 7 days prior to scheduled vitrectomy for vitreomacular traction and observed that 125 µg microplasmin was associated with a greater likelihood of induction and progression of PVD than placebo injection.12 Further randomized clinical trials are now ongoing to evaluate the safety and efficacy of microplasmin in association with vitrectomy or even as a monotherapy replacing the need for surgical intervention small macular holes (Fig. 127.1).
Plasmin
Plasmin was initially used by Verstraeten and coworkers to facilitate a PVD during vitrectomy in rabbit eyes. They found a positive effect but also mentioned a transient reduction of the b-wave amplitude in the electroretinogram as a potential adverse effect.13 This study was followed by other experimental trials confirming the proteolytic activity of plasmin on the vitreoretinal junction. Autologous plasmin was then used in clinical case series investigating the effect of a single injection without vitrectomy as a treatment for refractory diffuse diabetic macular edema,14 tractional diabetic macular edema15 or macular edema associated with branch retinal vein occlusion.16 The reduction of retinal thickness and improvement of visual acuity in these series supported an effectiveness of plasmin and the need for further trials. Autologous plasmin-assisted vitrectomy was performed for stage 3 macular holes, traumatic macular holes, diabetic macular edema and stage 5 retinopathy of prematurity17–22 and all of these trials underlined the potential of plasmin to facilitate vitrectomy and its good safety profile.
Hyaluronidase
Hyaluronidase has a potential to liquefy the vitreous, but does not induce a PVD in animal models.23 Therefore, its value in humans to relieve vitreoretinal traction seems limited. A phase III trial in diabetic humans suffering from vitreous hemorrhage showed a faster resorption of the vitreal hemorrhage as compared to a control group with no treatment-related relevant side-effects noted.24 However, a potential effect on the induction of a complete PVD in these patients was not further evaluated.
Dispase
Dispase represents a neutral protease that preferentially cleaves fibronectin and type IV collagen.25 Although initially shown to induce a PVD without damage to underlying tissue,26 subsequent trials brought up evidence for retinal bleedings, epimacular membrane formation, abnormalities in the electroretinogram responses and ultrastructural retinal damage.27 Thus, this enzyme was not further evaluated for clinical use.
Antiproliferative agents in the management of proliferative vitreoretinopathy
Proliferative vitreoretinopathy (PVR) is a serious and major complication of primary rhegmatogenous retinal detachment, severe diabetic retinopathy, and severe intraocular trauma. The pathophysiology of this disease implies a very complex cascade of events resulting in a subsequent proliferative response within the retina (see Chapter 97, Pathogenesis of PVR). Experimental studies described an intraretinal cellular response to retinal detachment, which is triggered by serum and growth factors present in the vitreous cavity28 and includes all types of non-neural cells such as RPE cells, astrocytes, microglia, macrophages, but predominantly Muller cells29–32 which is then followed by a fibrocellular growth on the subretinal or epiretinal surface.33 Both, subretinal fibrosis and epiretinal proliferation, have an impact on functional results and anatomical failure of retinal detachment surgery.33,34 As these cellular responses to retinal detachment may occur early in the development of the disease and may continue even in the longer term following (successful) surgical intervention, pointing to the need for an early pharmacological intervention and a long-term drug release or pharmacological effect.35
Other contributing factors include a relative hypoxia due to the distance between the neurosensory retina and the choriocapillaris,36 which leads to glial changes and photoreceptor deconstruction. These mechanisms are the target of recent and current approaches for an adjuvant pharmacologic intervention in PVR as these cellular responses can not be controlled by surgery alone.
Antiproliferative and anti-inflammatory agents have been the subject of in vitro investigations including substances such as colchicine, daunomycin and 5-fluorouracil.37,38 However, none of these agents have become part of any standardized procedure to treat or prevent PVR. Only daunomycin and 5-fluorouracil combined with low-molecular heparin were tested in clinical studies, which revealed no clinically relevant impact on PVR.39 Some 20 years ago, steroids applied intravitreally were used to suppress the process of PVR in clinical settings and in experimental studies.40 However, the effect was not lasting enough to avoid PVR.
New concepts include other agents such as alkylphosphocholines (APCs), which are synthetic phospholipid derivatives that have been shown to effectively inhibit cellular proliferation.41 Their mechanism of action involves binding to the membrane-bound G-protein PKC (protein kinase C), which is part of a major intracellular second-messenger system that regulates cell attachment, spreading, migration and proliferation. It was described in the literature that APCs have a potential to inhibit RPE cell spreading and migration as well as proliferation and cell-mediated membrane contraction at nontoxic concentrations in vitro and did not display any toxic effect of APCs to retinal tissue in in-vivo animal models.42 Besides prevention and treatment of PVR, APCs might have the potential for topical application as a single-dose agent to prevent posterior capsule opacification formation following cataract surgery.43
Tissue plasminogen activator in vitreoretinal surgery
This may be related to toxic effects of iron released from subretinal hemoglobin as well as an increased physical barrier for retinal diffusion and fibrotic changes.44–46 To date, there is no consensus on how to treat subretinal hemorrhages associated with neovascular age-related macular degeneration and most surgical treatment strategies seem insufficient to restore or improve vision.47
A displacement of the hemorrhage may be achieved by intravitreally applied expansile gas combined with intravitreal injection of recombinant plasminogen activator (rtPA). However, the subretinal lytic effect of intravitreally applied rtPA was challenged by some authors due to its molecular size and the reduced retinal diffusion.48,49 Therefore, a combination of intravitreal VEGF inhibitors to treat the underlying neovascular process combined with an injection of expansible gas is favored by some authors.50
In our own experience, intravitreal rtPA in combination with expansile gas was in the long-term more effective if combined with subsequent anti-VEGF treatment than intravitreal bevacizumab in combination with expansile gas alone (data submitted). Other groups have suggested triple therapies using rtPA, bevacizumab or ranibizumab and have shown a successful management of the disease with this approach.51,52 If rTPA and pneumatic displacement combination is contraindicated, an anti-VEGF monotherapy may be performed to prevent further visual loss.53 However, after intravitreal injection of any agent combined with expansible gas a vitreous hemorrhage may occur, very often due to a displacement of the subretinal blood into the vitreous cavity. In these cases, vitrectomy is indicated and may lead to good functional results.
It has also been suggested to perform a vitrectomy and apply rtPA subretinally followed by fluid gas exchange54 to displace the hemorrhage. This approach led to visual improvement in some cases. The authors also reported that vitrectomy with subretinal injection of rtPA and intravitreal gas tamponade was more effective than vitrectomy with intravitreal injection of rtPA and gas in terms of complete displacement of the submacular blood.55 Although functional improvement in the majority of patients suggests the absence of direct retinal toxicity of subretinally applied rtPA, vitrectomy and subretinal injection of rtPA bares a greater risk for postoperative complications.55
Despite good experiences in clinical use, experimental studies demonstrated dose-dependent negative effects of rtPA as seen by a significant and potentially irreversible reduction of the b-wave amplitude in ERG examination in bovine retinas.56
Visualization of the vitreoretinal interface
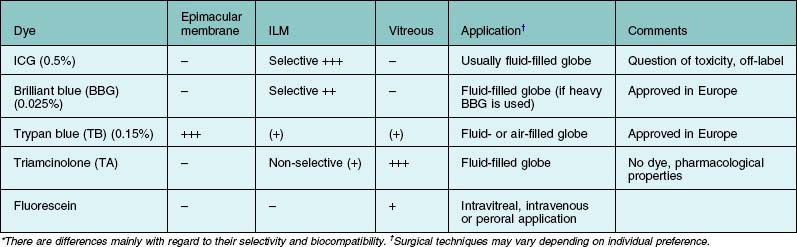
The application of vital dyes to visualize transparent and sometimes barely visible target structures such as the internal limiting membrane (ILM), epimacular membranes or vitreous has become very popular among vitreoretinal surgeons. The ILM is the main target structure for “chromodissection.” This is related to the fact that the ILM has been identified as an important scaffold for cellular proliferation. In order to remove all cellular proliferations, vitreous collagen remnants and relieve all relevant tractional forces, the ILM is dissected from the underlying tissue using the retinal surface of the ILM as a cleavage plane. The ILM can be removed without further visualization. A slight whitening of the retinal surface can be used as an indicator where ILM has been successfully peeled. However, this maneuver requires a lot of surgical experience and skills. The introduction of visualizing agents made ILM peeling accessible even to the less experienced surgeon. Several dyes are in clinical use and can be applied to selectively visualize the target structure (Table 127.1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree