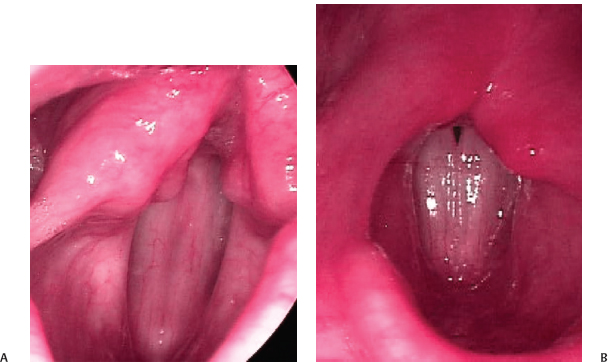
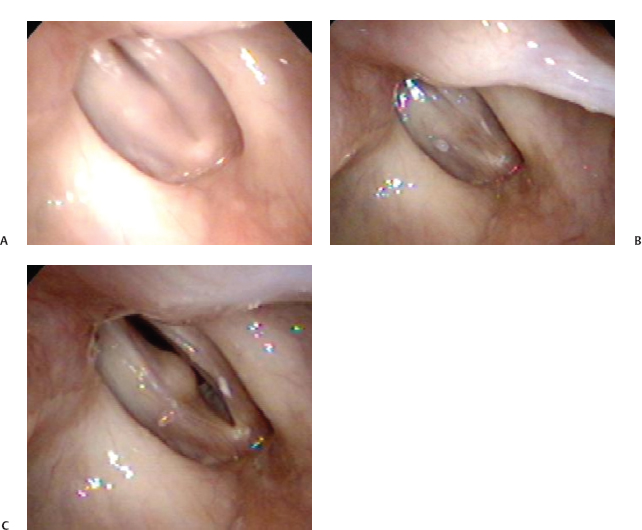
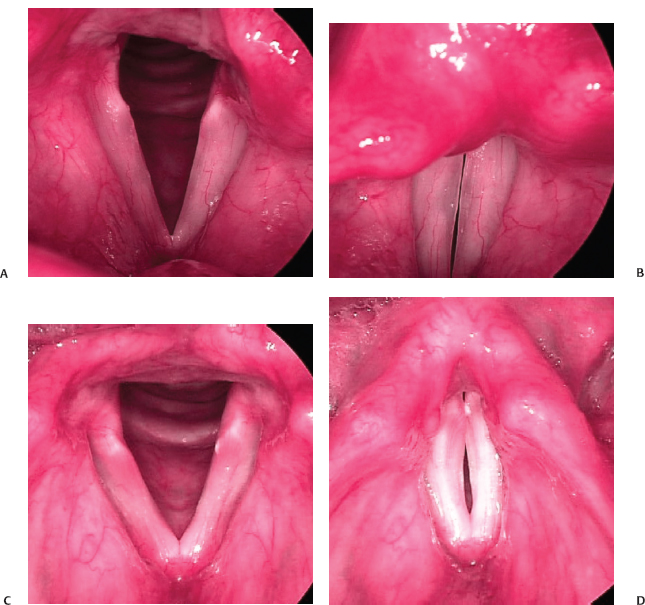
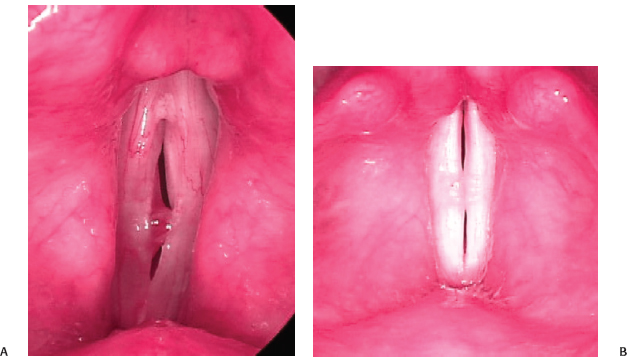
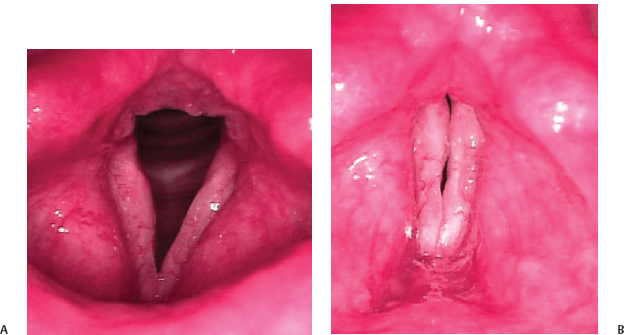
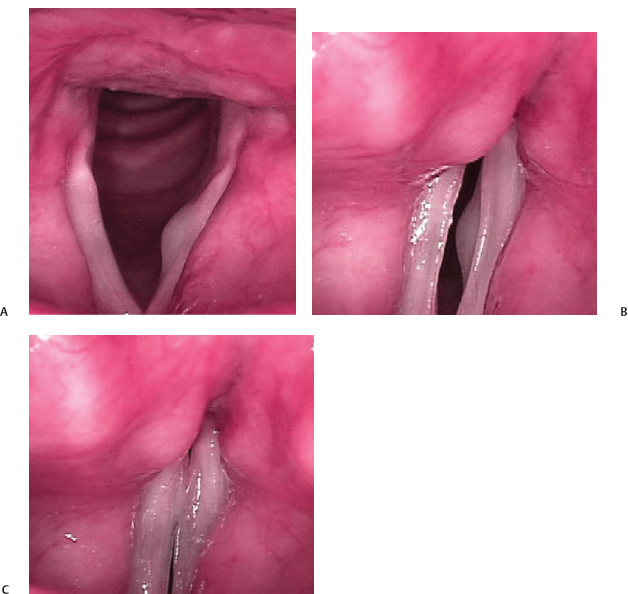
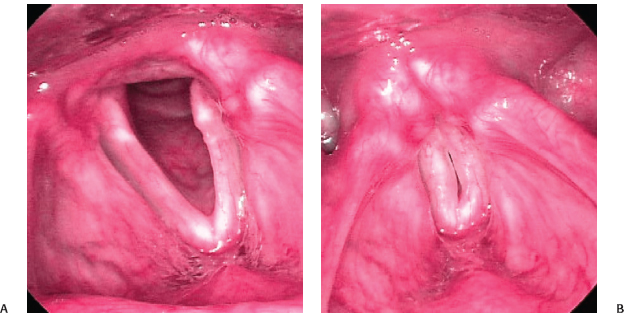
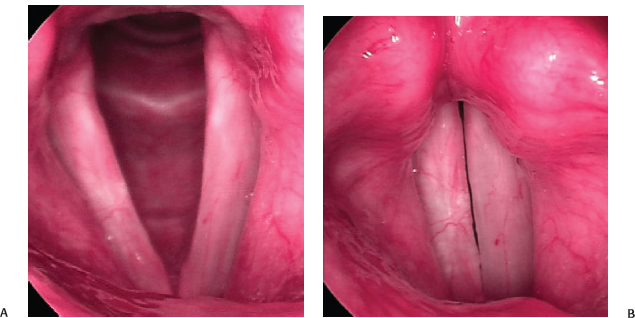
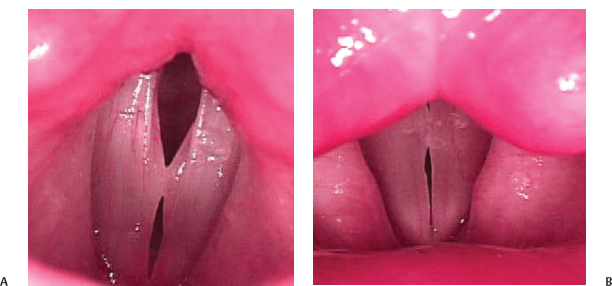
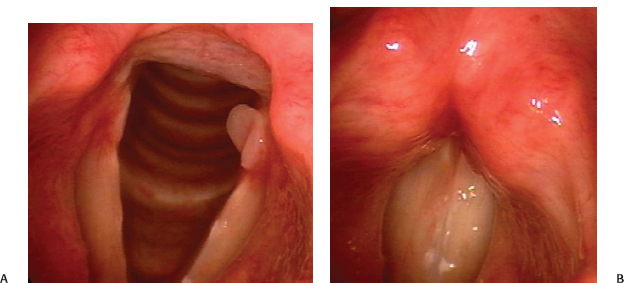
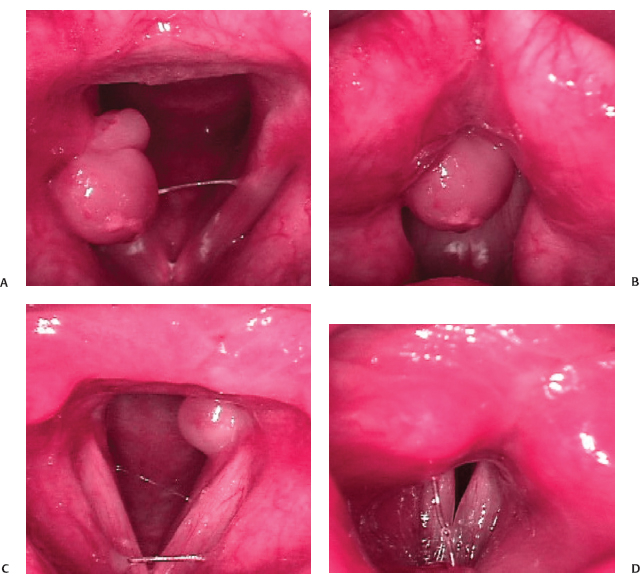
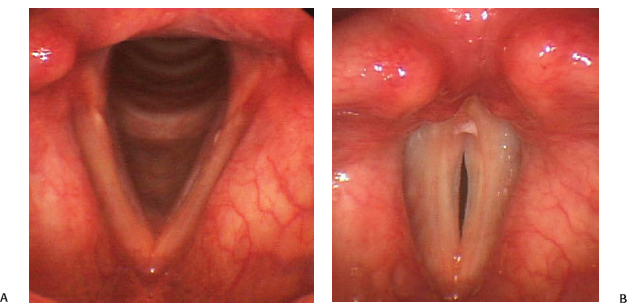
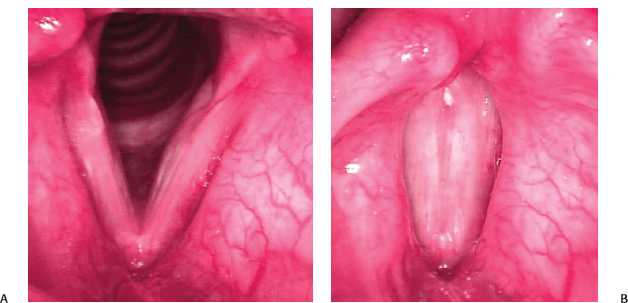
17 Glottic closure is the ability of the vocal folds to make contact along their medial edges. Videostroboscopy provides an effective tool for measurement of closure. In general, during the closed phase of the glottic cycle, the vocal folds should make complete contact along their length. In females, there is often a small gap posteriorly, which is considered normal (Fig. 17.1). With normal closure and normally vibrating vocal folds, air is released through the glottis in discrete puffs. This periodic pulsatile airflow is the glottic sound source.1,2 Incomplete vocal fold closure during voicing allows for leakage of air through the glottis in an uncontrolled manner. Often this escaping air creates noise that is perceived by the listener as breathiness or a hiss. Due to air escape, less air is available for voice production, which may cause the voice to be weaker than normal. Thus, in cases of glottic inefficiency, more air is required to create the same amount of sound. Also, more effort is usually employed by the speaker in an attempt to squeeze the vocal folds together and achieve complete closure. These last two factors may lead to vocal fatigue, a very common complaint in patients who suffer from incomplete glottic closure. Fig. 17.1 (A) Normal complete glottic closure in a male. (B) Small normal posterior gap in a female. In the normal larynx, the vocal folds are straight, taut, and fully mobile. These characteristics allow the vocal folds to come together fully during phonation. Pathology that interferes with any of these characteristics can affect the closure, including abnormalities of the vocal fold margin (medial tissues available for vibration) and abnormalities of the laryngeal musculature (medial compressive forces). In some cases of unilateral pathology, compensation by one vocal fold for abnormalities of the other can yield normal closure. The role of videostroboscopy in the assessment of closure cannot be overestimated. For years we had judged closure with the naked eye, viewing vocal folds vibrating over 100 cycles per second. At that speed, the edges of the vocal folds appear fuzzy and blurred to the eye, and whereas we can know if the vocal processes (where vibration does not occur) are in contact, we cannot know whether the membranous folds are truly making contact (Fig. 17.2). With stroboscopy, the apparent motion of the vocal folds is slowed down, and the rate of vibratory motion and the amount of time the vocal folds are in contact can be assessed. The technique of laryngeal stro-boscopy is covered elsewhere in this book. Be aware that the pitch at which the subject is phonating can affect glottic closure. Remember to test patients at different pitches. Fig. 17.2 (A) Right vocal fold cyst viewed with halogen light and without stroboscopy during phonation. Although we would expect closure to be incomplete, the image does not clearly demonstrate the status of the closure. (B) Right vocal fold cyst viewed with xenon light and with stroboscopy. Closure is noted to be complete during the closed phase of vibration. (C) Right vocal fold cyst viewed with stroboscopy. The cyst itself is much better defined during the open phase of vibration. The various configurations of a glottal gap (in incomplete closure) have been described by Bless et al.3 Note that some authors have described the pattern of closure rather than the shape of the gap, which may reverse the meaning of the descriptors.4 In this chapter, the descriptor relates to the shape or location of the gap rather than which part of the vocal folds are in contact. Closure can be affected by three basic problems: Fig. 17.3 (A) Left vocal fold paralysis. View of larynx with vocal folds abducted. (B) Left vocal fold paralysis with vocal folds adducted. Closure is incomplete along the entire length of the vocal fold, although the posterior glottis is difficult to see during phonation. (C) Bilateral vocal fold bowing viewed with vocal folds abducted. (D) Bilateral vocal fold bowing viewed with vocal folds adducted. Note that the vocal processes make contact, but the musculomembranous vocal folds cannot. Fig. 17.4 (A) Right vocal fold polyp prevents complete closure. The glottic gap is shaped as half an hourglass. (B) Vocal fold nodules cause incomplete closure in an hourglass configuration. Fig. 17.5 (A) Scarred vocal folds during abduction. (B) Scarred vocal folds during adduction with defect causing incomplete closure at site of defect. Edema of remainder of vocal folds contributes to inability to close at defect site. Fig. 17.6 (A) Left vocal fold cyst and bilateral vocal fold bowing viewed with vocal folds in abduction. (B) Left vocal fold cyst and bilateral vocal fold bowing viewed with vocal folds in adduction during the open phase of vibration. (C) Left vocal fold cyst and bilateral vocal fold bowing viewed with vocal folds in adduction during the closed phase of vibration. Closure is incomplete because of the bowing, not the cyst. Removal of the cyst would not improve closure. The information obtained with videostroboscopy helps us determine which type of lesion is present and which procedure or treatment is necessary to improve closure. With mass lesions, excision of the lesion will usually lead to improved closure. However, stroboscopy will sometimes reveal that closure would be incomplete even in the absence of the lesion (Fig. 17.6). In these cases, a significant improvement in voice may not result from excision, and the patient can be counseled accordingly, or the lesion may be left alone. Vocal fold immobility is due to either paralysis of the musculature that moves the vocal fold or fixation of the cricoarytenoid joint. An immobile vocal fold may rest in the midline or in a paramedian or even lateral position. If the vocal fold is not in the midline, incomplete closure is likely to result (Fig. 17.3A,B). In the case of a paralyzed vocal fold, as opposed to a fixed cricoarytenoid joint, the muscle is often flaccid and the vocal fold is bowed (Fig. 17.7). The bowed configuration of the paralyzed vocal fold further contributes to the open glottic configuration (Video Clip 27). Fig. 17.7 (A) Left vocal fold paralysis viewed with vocal folds in abduction. (B) Left vocal fold paralysis with flaccidity seen with vocal folds in adduction. In some cases of unilateral vocal fold immobility, the mobile contralateral vocal fold may be able to cross the midline to make contact with the immobile vocal fold and achieve complete closure. (However, the open phase may still predominate during the vibratory cycle in modal phonation [Video Clip 28]. In that case, the patient may complain of a soft, breathy voice, despite complete closure.) Similarly, complete closure may occur in cases of vocal fold paralysis where a certain degree of reinnervation has occurred. Unfortunately, this does not always result in a mobile vocal fold, as synkinesis often results. This means that both abductor and adductor muscles contract at the same time so that the vocal fold remains immobile but has tone. The synkinetic vocal fold is an immobile, straight vocal fold that may rest in the midline, making it easy for the mobile vocal fold to make full contact and achieving complete closure. When vocal fold closure is incomplete due to vocal fold paralysis, there is usually a gap from the anterior commissure to the vocal process of the arytenoid cartilage or even to the posterior aspect of the glottis (Fig. 17.8). With an isolated recurrent laryngeal nerve lesion (superior laryngeal nerve and cricothy-roid muscle functioning), a subject may be able to attain better closure at high pitch when the cricothyroid muscle is active. Hence, some patients with a paralyzed vocal fold will speak at an unusually high pitch to compensate for the weak voice at normal pitch (Video Clip 25). The effect on the mucosal wave of an immobile vocal fold depends on the glottal gap. If closure is normal and there is good vocal fold tone, the mucosal wave may be normal, and vibration may be symmetric with the normal fold. With a large gap, there may be no observable wave or the voice may be so aperiodic that stroboscopy is unable to reliably demonstrate the wave (Video Clips 29 and 30). With a small gap, the wave of the immobile fold is likely to lag behind that of the normal fold (Video Clip 28).5 In cases of immobility, the initial workup is aimed at determining the cause of the mobility problem. A computed tomography (CT) scan from the skull base to below the arch of the aorta will detect most neoplasms involving the vagus or recurrent laryngeal nerves. Laryngeal electromyography (EMG) with testing of the intrinsic laryngeal muscles (usually thyroarytenoid and cricothyroid muscles) can help locate the site of the lesion (recurrent laryngeal and/or superior laryngeal nerve or vagus nerve) and may provide information regarding the prognosis for recovery. If the EMG is normal, then the vocal fold is mechanically fixed. This can be confirmed with direct microlaryngoscopy and palpation of the arytenoid cartilage.6–8 Careful examination of the subglottis is critical to ruling out causes of fixation, such as the rare chondroid tumor of the cricoid cartilage (which would also been seen on the CT scan done earlier). Fig. 17.8 (A) Right vocal fold paralysis seen with vocal folds abducted. (B) Right vocal fold paralysis with straight vocal fold and better closure on adduction. There are also many other, less common neurologic disorders that will result in impaired vocal motion and glottic closure. These must be considered when the etiology is not due to some other obvious cause.9 If accommodation does not occur and the vocal fold does not recover normal motion, closure will remain incomplete, and the voice will remain abnormal. There are surgical options to improve the voice. Closure can be improved by bulking up the immobile vocal fold with injection laryngoplasty, medialization of the vocal fold with framework surgery, with or without arytenoid adduction or arytenoidopexy, or reinnervation of the paralyzed vocal fold (Fig. 17.9). Restoration of normal closure may yield normal vibration and mucosal wave propagation in the paralyzed vocal fold despite lack of reinnervation (Video Clip 31).10,11 As we age, muscles and ligaments may become less taut. In the vocal fold, this results in bowing. The vocal folds are still mobile but cannot come completely together. Because there is no paralysis, the arytenoid cartilages are still fully mobile, and the vocal processes will make contact but the musculomembra-nous folds do not, resulting in a lentiform-shaped persistent glottic opening (Fig. 17.3C, D; Video Clips 16, 17, and 24). Atrophy of the vocalis muscle as a result of a paresis will also result in lack of bulk and bowing of the vocal fold and incomplete closure. With the vocal fold mobile, the workup is usually not as aggressive, as a neoplastic etiology is less likely. EMG can confirm a paresis. Voice therapy may result in improved closure and voice. As with the immobile vocal fold, surgery can be done to improve closure in cases of bowing or paresis. With a bowed but otherwise mobile vocal fold, the musculomembranous vocal fold should be medialized, but movement of the arytenoid should not be impaired. The size of the glottic gap can be documented with videostroboscopy, and this information can be used to judge the amount of medialization necessary. Fig. 17.9 (A) Closure prior to medialization of paralyzed left vocal fold. (B) Closure after medialization of paralyzed left vocal fold. (C) A mucosal wave can be seen on the paralyzed left vocal fold after medialization. Most benign vocal fold masses occur on the musculomembranous vocal folds. With phonation, these masses often make initial contact and prevent the remainder of the vocal folds from making contact, preventing complete closure. The location, size, shape, and consistency of the various lesions will determine how closure is affected. Nodules, cysts, pseudocysts, and polyps are all masses that may develop on the musculomembranous vocal folds. They are sometimes difficult to differentiate.12,13 Classic vocal fold nodules are symmetric masses in the midportion of the musculomembranous vocal folds, and their premature contact results in a glottic opening in the shape of an hourglass (Fig. 17.4B; Video Clip 18). Often, other benign lesions such as cysts and pseudocysts will be associated with a contralateral reactive nodule that may be close to the same size as the original lesion. Again, an hourglass-shaped glottic opening will result (Fig. 17.10). If there is only a unilateral lesion, such as a polyp or cyst, glottic closure will be shaped as half an hourglass (Fig. 17.4A; Video Clip 26). Higher pitch will stretch the vocal folds and accentuate the effect of a lesion of the vocal fold. At lower pitch, a lesion may not even be visible and closure may be normal, whereas at high pitch the lesion becomes apparent and closure is incomplete. This point stresses the importance of testing all patients along their full dynamic range. Fig. 17.10 (A) Left vocal fold polyp orpseudocyst and reactive swelling of the right vocal fold. Vocal fold tissue makes early contact at this site prior to reaching maximal closure. (B) Left vocal fold polyp or pseudocyst and reactive swelling of the right vocal fold. Closure is incomplete during the closed phase of vibration in an hourglass configuration. Granulomas are benign inflammatory masses that almost always occur on the vocal process of the arytenoid cartilage. When they are small, they do not affect closure at all, and the contralateral vocal process fits into a notch in the granuloma (Fig. 17.11). Even large granulomas often do not affect closure (Fig. 17.12). A fortunately less common cause of incomplete closure is a defect of the musculomem-branous vocal fold. This is usually a result of surgical excision of a mass from the vocal fold. Videostroboscopy demonstrates the exact configuration of closure and the location of the defect (Fig. 17.5). It also shows whether the tissue at the site of the defect vibrates normally or not. This is very important, as surgery to improve closure at the defect may not achieve a normal voice if the tissue was not vibrating properly preoperatively. Surgical procedures, such as fat graft implantation into the defect, have been designed both to improve closure and hopefully restore vibration to the vocal fold edge. If the tissue at the site of the defect vibrates normally (mucosal wave is present) and closure is incomplete, surgery should be focused on improving closure without disrupting the architecture of the edge of the vocal fold, which might yield a nonvibrating segment. Fig. 17.11 (A) Left vocal fold granuloma seen during abduction of vocal folds. (B) During adduction, left vocal fold granuloma does not affect closure. Fig. 17.12 (A) Large, right-sided granuloma seen with vocal folds abducted. (B) The same large, right-sided granuloma does not affect closure, which is complete. (C) Large, left-sided granuloma in another patient seen during vocal fold abduction. (D) The left-sided granuloma in this patient seems to prevent closure posteriorly. Sulcus vocalis is a condition in which there is a longitudinal scar on the medial edge of the vocal fold with adherence of the mucosa to the underlying vocal ligament (Fig. 17.13).14 This is thought to be due to chronic voice abuse/overuse or perhaps to the rupture of an intracordal cyst. These patients present with rough, breathy voices and voice fatigue. The initial impression on physical examination is that the vocal folds are bowed, and closure is usually incomplete. Videostroboscopy reveals a groove on the medial edge of the vocal fold that is usually not detected without stroboscopy. Also, the mucosal wave is absent. The surgical approach to these patients is somewhat controversial. Improving closure with framework surgery or injection is often the first step. A stronger voice with less fatigue usually results, but it is still not a normal voice (Fig. 17.14). Addressing the sulcus itself is, in this author’s opinion, a technically much more challenging procedure than improving closure and carries higher risk. Fig. 17.13 (A) Bilateral sulcus vocalis and vocal fold bowing seen with the vocal folds abducted. (B) Bilateral sulcus vocalis and vocal fold bowing with incomplete closure during adduction. Fig. 17.14 (A) Bilateral sulcus vocalis and vocal fold bowing seen with the vocal folds abducted after bilateral medialization. (B) Bilateral sulcus vocalis and vocal fold bowing. There is improved closure and voice after medialization of both vocal folds. The differential diagnosis of a persistent glottic gap during phonation includes lesions that affect the medial tissues of the vocal fold margin and lesions that affect the compressive abilities of the vocal folds. Lesions of the medial tissues of the vocal fold include benign vocal fold lesions due to trauma and scarring of the vocal folds from any cause. These lesions prevent complete closure of the glottis during voicing by the change they impart to the shape of the vocal fold margin. Lesions that affect the compressive abilities of the vocal folds include vocal fold paralysis and paresis and prevent closure by their effect on the position of the vocal fold during phonation. 1. Hirano M. Clinical Examination of the Voice. New York, NY: Springer-Verlag; 1981 2. Colton RH. Physiology of phonation. In: Benninger MS, Jacobson B, Johnson A, eds. Vocal Arts Medicine: The Care and Prevention of Professional Voice Disorders. New York, NY: Thieme Medical Publishers; 1993:30–60 3. Bless DM, Hirano M, Feder RJ. Videostroboscopic evaluation of the larynx. Ear Nose Throat J 1987;66:289–296 4. Gelfer MP, Bultemeyer DK. Evaluation of vocal fold vibratory patterns in normal voices. J Voice 1990;4: 335–345 5. Sercarz JA, Berke GS, Ming Y, Gerratt BR, Natividad M. Videostroboscopy of human vocal fold paralysis. Ann Otol Rhinol Laryngol 1992;101:567–577 6. Altman JS, Benninger MS. The evaluation of unilateral vocal fold immobility: is chest X-ray enough? J Voice 1997;11:364–367 7. Benninger MS, Crumley RL, Ford CN, et al. Evaluation and treatment of the unilateral paralyzed vocal fold. Otolaryngol Head Neck Surg 1994;111:497–508 8. Terris DJ, Arnstein DP, Nguyen HH. Contemporary evaluation of unilateral vocal cord paralysis. Otolaryngol Head Neck Surg 1992;107:84–90 9. Benninger MS, Gardner GM, Schwimmer C. Laryngeal neurophysiology. In: Rubin J, Sataloff R, Korovin G, eds. Diagnosis and Treatment of Voice Disorders, 2nd edition. Clifton Park, NY: Thomson Delmar Learning; 2003:107–113 10. Gardner GM, Parnes S. Status of the mucosal wave post Teflon vocal cord injection vs. thyroplasty. J Voice 1991;5:64–73 11. Kokesh J, Flint PW, Robinson LR, Cummings CW. Correlation between stroboscopy and electromyogra- phy in laryngeal paralysis. Ann Otol Rhinol Laryngol 1993;102:852–857 12. Woo P, Colton R, Casper J, Brewer D. Diagnostic value of stroboscopic examination in hoarse patients. J Voice 1991;5:231–238 13. Sataloff RT, Spiegel JR, Hawkshaw MJ. Strobovideolaryngoscopy: results and clinical value. Ann Otol Rhinol Laryngol 1991;100(9 Pt 1):725–727 14. Ford CN, Inagi K, Khidr A, Bless DM, Gilchrist KW. Sulcus vocalis: a rational analytical approach to diagno sis and management. Ann Otol Rhinol Laryngol 1996;105:189–200
Persistent Glottic Opening
 Mobility Problems
Mobility Problems
Vocal Fold Paralysis
Vocal Fold Bowing and Vocal Fold Paresis

 Mass Lesions That Prevent Closure
Mass Lesions That Prevent Closure
 Defects in the Vocal Fold
Defects in the Vocal Fold
Sulcus Vocalis
 Conclusion
Conclusion
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


