Purpose
To describe a novel method for placement of a sulcus-fixated, sutured posterior chamber intraocular lens (sf-SPC-IOL) using endoscopic guidance during pars plana vitrectomy surgery.
Design
A retrospective case-series by a single surgeon in both pediatric and adult patients undergoing sf-SPC-IOL in the setting of posterior segment surgery.
Methods
Seventy-four eyes of 71 patients had pars plana vitrectomy and placement of an sf-SPC-IOL in an academic, outpatient setting. Preoperative diagnosis included trauma (42%), subluxated lenses with no capsular support (24%), uveitis (15%), congenital cataract (11%), Marfan syndrome or ectopia lentis (6%), and other (2%). Fifty-one adults and 20 children (<18 years of age) were reviewed from cases performed from 1999 through 2007. The sf-SPC-IOL sutures were placed using endoscopic visualization of ab interno scleral fixation.
Results
The mean follow-up time was nearly 3 years (3 months to 9 years) and most patients experienced an improvement in visual function. Many eyes had advanced posterior segment disorders. Only 2 broken sutures occurred, both attributable to repeat trauma. Advantages of this technique include: excellent visualization and haptic localization, optimal lens centration, buried knots, broad scleral imbrication, and minimal vitreous- and hemorrhage-related complications. Disadvantages include the learning curve, increased operative time, long-term suture stability issues, and limited availability of intraocular endoscopes.
Conclusions
Endoscopic-guided sf-SPC-IOL using this approach, in the setting of posterior segment disease, is a reasonable option for visual rehabilitation in both pediatric and adult patients.
Placement of an intraocular lens is a common and routine procedure during ophthalmic surgery. There is broad consensus that placement of a posterior chamber intraocular chamber lens (PC-IOL) in the capsular bag remains the preferred location. However, in the absence of adequate capsular support, alternative techniques have been employed. The most common approach is to simply place an open-loop designed intraocular lens into the anterior chamber angle (AC-IOL). This technique also has gained broad acceptance. There are no comparative, prospective randomized studies that suggest a strong preference for one type of lens over another in the setting of limited capsular support in younger adults or in children. In Turkey, Evereklioglu and associates compared outcomes and complication rates in a series of eyes with no capsular support that had either open-loop AC-IOL placement (73 eyes) or a scleral fixated sutured PC-IOL (sf-SPC-IOL) placement (51 eyes). The conclusions were that both methods are safe; however, the sf-SPC-IOL had a more favorable outcome and lower complication rate than the AC-IOL group. The authors noted that the sf-SPC-IOL was technically more difficult. According to a practice pattern survey (2003) of the American Society of Cataract and Refractive Surgery and the American Association for Pediatric Ophthalmology and Strabismus, 70% of the respondents had a preference for sf-SPC-IOL in the setting of no capsular support. An sf-SPC-IOL may be beneficial in patients where placement of an AC-IOL is suboptimal. For example, an AC-IOL may be contraindicated in the setting of trauma with iris or angle injury, uveitis, chronic cystoid macular edema (CME) from lens chafe, or open- or closed-angle glaucoma in young adults or children with a long-term risk of endothelial cell loss and corneal decompensation.
Identification of the sulcus for proper suture placement can be performed using several techniques. Duffey and associates identified the sulcus in 21 cadaver eyes and suggested that by measuring either 0.83 mm vertically or 0.46 mm horizontally from the limbus, the average ciliary sulcus location may be estimated in cases using an ab externo approach. Sharkey and Murray suggested that transillumination of the ciliary body is helpful to localize the suture pass for sf-SPC-IOL. Pavlin and associates used ultrasonography to localize the haptics. However, despite these techniques, many sf-SPC-IOL are not located in the sulcus. Sewelam and associates, using ultrasound biomicroscopy from an ab externo approach, only found 55% to be located in the sulcus while 27.5% were anterior to the sulcus and 17.5% were posterior to the sulcus.
The endoscope was introduced for ophthalmology in approximately 1990. In 1996, Jurgens and associates described the use of an endoscope to localize the sulcus in the setting of sf-SPC-IOL placement. This procedure made use of a straight needle on a 16-gauge sheath over the endoscope that allowed direct visualization of the sulcus as well as needle insertion. In 1993, Lewis described an sf-SPC-IOL technique that avoided the use of scleral flaps. This important step allowed for the knots to be buried and rotated in order to avoid exposure. The work by Johnston and associates also supports the concomitant placement of sf-SPC-IOL in combination with pars plana vitrectomy and emphasizes that a complete vitrectomy reduces long-term complications in a similar case mix as those reported herein.
In this retrospective series, we describe a novel technique for sf-SPC-IOL placement that combines many previously described techniques in adult and pediatric eyes with posterior segment pathologies. Our technique uses a pars plana approach, endoscopic ab interno suture placement, buried knots, substantial scleral imbrication, and a large optic lens while specifically avoiding scleral flaps and exposed suture knots.
Methods
We retrospectively reviewed 74 eyes of 71 patients (46 male, 25 female) and divided our series into pediatric (age ≤18; 21 eyes; 20 subjects [16 male, 4 female]; age range 3-18; mean age = 10) and adult (age >18; 53 eyes; 51 subjects [30 male, 21 female]; age range 21-87; median age = 51) cases. A single surgeon (T.W.O.) performed the technique used for all cases. Minor modifications of the technique evolved over the initial 2 to 3 years.
Patients
A consecutive series of candidates for sf-SPC-IOL from August 1999 through September 2007 were reviewed. Patients were considered candidates if they lacked zonular support for a sulcus PC-IOL or if they had a history of severe uveitis, anterior segment or iris root trauma, open- or closed-angle glaucoma, or other relative contraindications to an AC-IOL. In the pediatric age group, 12 eyes had trauma involving the posterior segment and lacked capsular support for an IOL. Eyes had serious injuries that included retinal detachment, suprachoroidal hemorrhages, choroidal ruptures, posterior globe ruptures, traumatic macular holes, proliferative vitreoretinopathy, and other trauma-related injuries. Eyes were commonly left aphakic during the primary repair and the sf-SPC-IOL was placed at the time of silicone oil removal when the eyes appeared to have macular potential. Six eyes had congenital cataract surgery, were left aphakic, and were intolerant or noncompliant with contact lens wear. One such eye was microphthalmic, requiring a 38-diopter (D) IOL, and 2 IOLs were placed in a piggyback manner using this same technique (20-D + 18-D IOL). Two eyes of 1 child had severe uveitis. An initial procedure using vitrectomy and lensectomy with placement of the lens in the capsular bag resulted in a dense cyclitic membrane and hypotony maculopathy despite aggressive management of the uveitis. The lens, capsular bag, and cyclitic membrane were removed and an endoscopic sf-SPC-IOL was placed. The intraocular pressure normalized and the visual acuity improved to approximately 20/70 (limited as a result of hypotony maculopathy). The fellow eye was done using sf-SPC-IOL primarily and there were no postoperative complications other than management of recurrent episodes of uveitis. Final visual outcome was much better in the second eye (20/25) when an sf-SPC-IOL was performed as the primary surgery. A second uveitic pediatric case had juvenile idiopathic arthritis (JIA) and an sf-SPC-IOL was placed primarily.
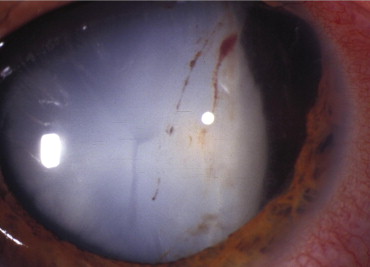
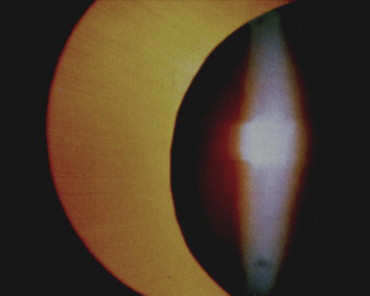
In the 51 adult patients, 18 eyes had both anterior and posterior segment trauma ( Figure 1 ) or lacked adequate capsular support for a sulcus-based IOL, or there were concerns about placement of an AC-IOL. Seventeen eyes either had dislocated PC-IOLs and lacked capsular support, or had dislocated crystalline lenses. The decision for an sf-SPC-IOL was made either based on their age (arbitrarily set at <50 years old) or because there was a contraindication for an AC-IOL (eg, glaucoma). Uveitis cases (9) included intermediate uveitis (2), JIA in cases over age 18 (2), sarcoidosis (1), UGH syndrome (uveitis, glaucoma, and hyphema) (2), and chronic CME from either an iris-fixated IOL (1) or a closed-loop AC-IOL (1). Other cases included Marfan syndrome (3) ( Figure 2 ), ectopia lentis (1), congenital cataract patients that were left aphakic (2), and an iris colobomatous defect with no zonular or iris support (1). Two patients had AC-IOLs removed in the presence of chronic CME.
The surgical technique is schematically characterized in Figure 3 . First, a standard 20-gauge 3-port pars plana vitrectomy was performed.
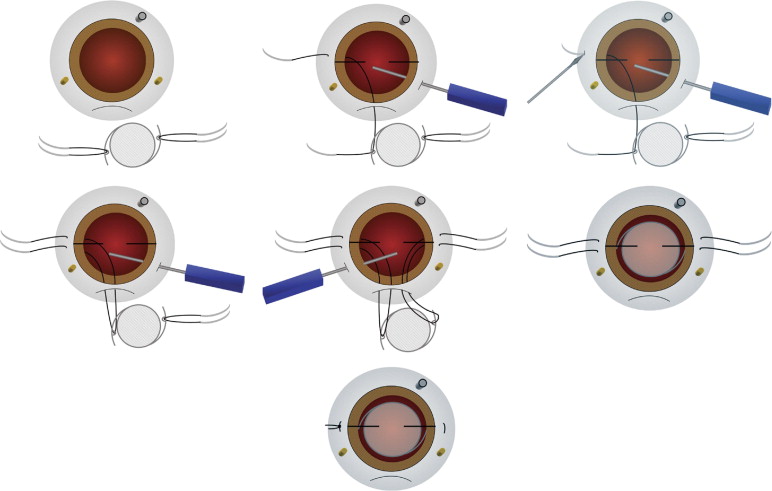
Sclerotomy Location and Marking
During the initial set-up, careful attention to placement of the sclerotomies is important ( Figure 3 , Top left). The infusion sclerotomy is placed more inferior than for a normal vitrectomy. Therefore, the lid speculum needs to be opened slightly wider than normal. This allows for better access to the superior incision and also allows for globe mobility with a more inferiorly displaced infusion line. The purpose of an inferiorly displaced infusion line is to minimize lens rotation that may result when the internal aspect of the infusion cannulae is sutured too close to the 3-o’clock and 9-o’clock position (site for haptic suture fixation). The arms of the haptic will be rotated out of the ciliary sulcus when the infusion is adjacent to the horizontal meridians. Also, the needle pass at the horizontal line may be obstructed if the infusion is too close. Therefore, the infusion is either placed near the 5-o’clock or 7-o’clock position for a left or right eye, respectively. Next, the superior sclerotomy placement is also important to properly localize. They must be at the 2-o’clock and 10-o’clock position. If they are placed too close to the 3-o’clock and 9-o’clock position, they interfere with the needle pass and place the 10-0 prolene at risk for interfering with the sclerotomy. If the placement is too superior, then the endoscope does not have a direct advantage for a straight view of the opposite sulcus, and the superior scleral tunnel incision may be compromised.
Conjunctival Opening
When opening conjunctivae with 20-gauge surgery, a broad circumferential incision very close to the limbus is encouraged. Care is taken to allow adequate incisional opening for the inferior sclerotomy as well as the superior wound. For a right eye, the conjunctiva will be opened from the 6:30-o’clock to 4-o’clock position in a clockwise manner, and from the 8-o’clock to 5:30-o’clock position in a left eye. Using small-gauge surgery, 3-o’clock and 9-o’clock areas need to be opened to accommodate the 10-0 prolene along with a superior opening for the IOL. Ink marks are then made on the sclera to define the sclerotomies and a 7-mm superior scleral tunnel incision.
Centration Marking
In order to optimize centration, a radial keratotomy (RK) marker is used with ink on 2 horizontal blades ( Figure 3 , Top center). The circular RK marker is centered on the pupillary axis so that ink marks are made on the cornea to delineate the 3-o’clock and 9-o’clock position. These marks will help localize suture placement and optimize lens centration.
Pars Plana Vitrectomy and Superior Wound Creation
After the sclerotomies are made, the posterior hyaloid is elevated and the vitreous is removed. Posterior segment injuries are repaired primarily. Next, the vitreous base is shaved and capsular remnants are removed. A frown-shaped, superior beveled lamellar incision is made with an angled blade. A goal for the entrance of the incision with a sharp keratome is to enter the anterior chamber approximately 2 mm into clear cornea in order to minimize iris prolapse during suture placement and lens insertion. Proper scleral tunnel wound construction improves the ease of the case, especially with placement of the ab interno needle pass.
Suture Placement
After confirming the correct lens power, a CZ70BD lens (Alcon Laboratories; Fort Worth, Texas, USA) is opened and placed on the drape, just superior to the eyelid. Two separate double-armed 10-0 prolene sutures on CIF-4 needles are used (Ethicon Inc, Somerville, New Jersey, USA). A single needle of each suture is passed through the eyelet of the IOL ( Figure 3 , Top left) so that the lens haptics are oriented properly (as one would position a lens for dialing clockwise). The proximal-most base of the needle is grasped with a needle driver in order to pass the needle through the superior beveled incision. The endoscope is placed in the contralateral sclerotomy. Important at this point, the infusion is clamped to avoid iris prolapse during needle entry into the anterior chamber. The backhanded needle is introduced using a sweeping technique (opposite to the direction of the needle tip) across the beveled incision. This technique avoids needle engagement into the scleral or iris tissues around the tunnel. Once the needle has entered the anterior chamber, it is then directed forward, in a slow and deliberately advancing motion toward the sulcus, just inferior to the horizontal corneal centration marking. The tip can then be localized into the sulcus with the endoscope ( Figure 3 , Top center) (GRIN solid rod endoscope, Insight Inc, Stuart, Florida, USA). Once the needle is engaged and the entry confirmed, the exit site through the sclera is less critical and can be directed horizontally through the sclera. Before the needle is pulled out of the sclera, a sharp pointed blade (such as a microvitreoretinal blade) engages the sclera at the external needle exit site in order to slightly enlarge the needle track and allow for the knot to be buried more easily ( Figure 3 , Top right). The second arm of the suture is then passed in a similar manner, just superior to the horizontal meridian ( Figure 3 , Middle left). The goal is to separate the 2 passes by at least 2 mm. Care is taken not to grasp or manipulate the prolene that is left remaining to hold the haptic with any instrument other than a smooth 10-0 tying forceps, thus avoiding a weakened suture. The infusion is turned on intermittently to maintain adequate intraocular pressure and turned off when passing a needle into the anterior chamber. The process is repeated on the opposite side ( Figure 3 , Middle center).
Lens Insertion, Avoiding Suture Entanglement
An important aspect of this technique is to maintain a tight and clear line for the sutures as the IOL is passed into the eye ( Figure 3 , Middle right). An angled smooth forceps is used to hold the optic, and a 10-0 smooth tying forceps is used in the opposite hand to maintain a “tight line” with each of the 4 exit sites of the prolene suture. The infusion is temporarily turned to the off position while the lens is inserted slowly and each of the 4 suture lines is kept tight (avoiding slack in the suture). Care is taken to prevent the 10-0 prolene from wrapping around or twisting around the haptic. Twisting, rotation, or unintended haptic capture will cause either lens rotation or inability to rotate and bury the knots after the ends are tied. Once the lens is in the eye, the prolene sutures are pulled to secure the lens into the sulcus. The infusion is then turned on.
Tying and Rotating the Knots
Only 10-0 smooth forceps are used to lift the prolene and both (2) forceps are used to lift on the suture in a seesaw manner (as though pulling on 2 opposite ends of a rope on a pulley) to be sure that the haptics are not twisted around the suture ( Figure 3 , Middle right). If the suture does not rotate easily, the haptics may be wrapped. A decision needs to be made at that point to remove the lens and reinsert or to leave the haptics tangled. If the lens centers well, it is reasonable to tie it in place. Both ends of the prolene are cut and a slip-then-lock-knot (1-1-1) configuration is used to ensure a secure knot that is not too large to bury. The suture is then gently buried by rotating the knot ( Figure 3 , Bottom). If it cannot be rotated and buried, the ends are left long (>2 mm) and the ends of the suture are secured posteriorly using a partial-depth 10-0 nylon suture that keeps the ends from extending out of the conjunctival opening ( Figure 3 , Bottom). Should the knot fail to rotate, avoid cutting the ends short, as they will protrude through conjunctiva postoperatively. Such protrusion will create a potential pathway for microbes to gain access to the vitreous that could lead to endophthalmitis. A scleral patch graft should be placed to cover any residual sharp, protruding proline sutures, should the methods described fail.
Closure
Once the lens is centered, haptics secured, and knots buried or ends left long and tied posteriorly, the superior wound, sclerotomies, and conjunctiva are meticulously closed in order to cover the prolene sutures. If properly buried, even with minimal or scarred conjunctiva, the sutures are so smooth that they will epithelialize.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


