Chapter 7 Otitis Media: Background and Science
Introduction to the Problem
Otitis media (OM) is a common clinical problem that affects millions of people around the world. OM represents a spectrum of disease processes that include acute otitis media (AOM), recurrent acute otitis media (RAOM), otitis media with effusion (OME), and chronic otitis media with effusion. In the early portions of the 20th century, persistence of otitis media was termed secretory otitis media.1,2 Now considered to be equivalent to otitis media with effusion (middle ear effusion without signs of acute ear infection), this secretory otitis was noted to be resistant to typical therapeutic interventions while many of the patients were noted to have a history of atopic disease.1–6 Since that time numerous studies have attempted to establish a causal relationship between atopy and OME. Many of the early studies lacked proper controls and were fraught with misclassification bias due to poorly defined disease criteria. Over the last 10–15 years, no study has yet to definitively identify allergy as an etiologic agent in the pathogenesis of OME.6–8 However, numerous studies continue to demonstrate an association between atopy and OME.9–22 Whether research identifies absolute or implicit causality between allergy and OME, it is important that the clinician recognizes the potential role of atopy in the development of and persistence of OME to adequately approach therapeutic options and/or interventions for their patients.
Over the last decade, a change in the approach to the allergic patient has developed, in which an intimate relationship is thought to exist between the upper and lower airways in allergic disease.9,23,24 The concept of an “united airway” in the disease process holds that the middle ear, Eustachian tube, and the nasopharynx are thought to participate in the allergic Th2 immune-mediated hypersensitivity response in a similar manner as the remainder of the upper and lower airway.8,23,24 Therefore, allergic inflammation is not confined to a specific site or target organ but is considered to range throughout the common airway.8,9,23,24 This chapter reviews the epidemiology, anatomy, pathophysiology, and diagnosis of suspected allergic middle ear disease, as well as provides an evidence-based, united airway approach for the management of the patient with otitis.
Epidemiology
Otitis media (OM) and otitis media with effusion (OME) represent significant health problems with greater than 2.2 million episodes diagnosed per year in the USA.5,7 This translates into one of the most frequent health-related problems for which children receive medical care in the USA.5,7 OME is most prevalent in early childhood where screening surveys have reported point prevalence of middle-ear effusions (MEE) from infancy to 5 years of age to range between 15% and 40% with the peak incidence during the winter months.7,10,25–27 During the first year of life about half of all children will have one episode of OME, more than 60% by age two, and nearly 90% (80% of ears) will have at least one episode of OME at some time prior to school age.7,28,29
Most episodes of OME resolve within 3 months. However, about a third (30–40%) of children have recurrent OME with approximately 5–10% of episodes lasting a year or longer.3,5,7,25,28,29 The sequelae of repeated episodes or persistence of OME in children can be significant and may produce impairments in receptive language skills, balance, coordination, maintaining attention, and school readiness.7,12,30,31 The health-care-related expenditures associated with OME have been estimated to be anywhere between US$3 and 5 billion dollars annually.5,32,33 However, this may drastically underestimate the indirect impact on society. The burden of disease may also affect caregivers of those with OME. Quality of life surveys have found that more than 50% of the caregivers displayed physical problems: poor sleep, poor eating, or irritability due to recurrent AOM and chronic OME in children.34,35
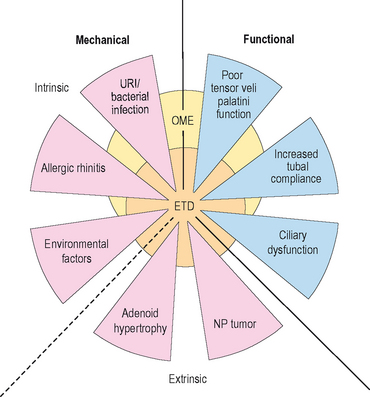
It is generally accepted that the development of OME is multifactioral. Eustachian tube dysfunction (ETD), bacterial and/or viral infection of the middle ear, and inflammation within the nose resulting from allergic rhinitis or upper respiratory infection are some of the contributors that play an important, interrelated role in the development of OME (Figure 7.1).5,6,9 Although no casual evidence directly links allergy as an etiologic agent in OME, population studies have shown a distinct relationship between allergy and OME.16,17 In Sweden, atopic infants were five times more likely to develop OME than nonatopics.16 In Japan, more than 87% of those with OME were found to have allergic symptoms and/or be atopic.17 Jero et al noted that those with allergy were 4.4 times less likely to clear acute episodes of OM.36 Other studies report that as many as 50% of all patients with otitis media have allergic rhinitis and 21% of patients with nasal allergy have otitis media.7,14 Nguyen et al showed that the allergic inflammation seen in atopics with OME occurred both in the middle ear and the nasopharynx.9
Numerous risk factors for the development of OM have identified. Risk factors for otitis media (acute or chronic) include: recurrent upper respiratory infection, allergic rhinitis, eustachian tube dysfunction, exposure to cigarette smoke, bottle-feeding/short duration of breast feeding, male gender, immunologic deficiency, ciliary dysfunction, cleft palate disease, first degree relative with allergy, attendance to day care, and seasonal changes.14,15,30,37
In adults, the exact prevalence or incidence of OME is not known. However, studies have noted the link between poorly controlled allergic rhinitis and the development of OME.17,38,39 Allergic rhinitis is a very common disease process that is thought to affect up to a cumulative frequency of 42% of the US population by age 40 and a point prevalence of 40 million.38,39 Mion et al recently confirmed a community-based study by Tomonga where about 50% of patients with chronic OME presented with allergic nasal disease.17,37
Relevant Anatomy and Physiology
The middle ear cleft is defined by the middle ear (ME), the Eustachian tube (ET), and the mastoid air cells. From an anatomic standpoint, the ME is limited laterally by the tympanic membrane, medially by the promontory (bone overlying the basal turn of the cochlea), and anteriorly by the carotid canal and the ET. The ME directly communicates with the mastoid air cells via the aditus ad antrum posteriorly while the floor is bound by the jugular bulb which is also covered by air cells. The ET extends from the anteroinferior portion of the ME to the nasopharynx. In adults, the nasopharyngeal orifice of the ET measures approximately 8 × 4 mm and is 15 mm below the tympanic ostium at an angle of 45 degrees from the horizontal plane.40,41 In children, the ET is positioned 10 degrees from the horizontal plane and is considerably shorter.40
Although the anatomy of the ME cleft provides a structural framework to approach ME disease, from an immunologic standpoint, it is more important to think of the physiologic components of the ME in terms of a complex interrelated system composed of the middle ear space, ET, nasopharynx (adenoids), nasal mucosa, and the mastoid air cells.42 The ET has a key role in middle ear function in that it allows for communication between the nasopharynx and middle ear. Swallowing causes the tensor veli palatini to actively open the ET and thus ventilates the middle ear with atmospheric pressure.14,40 (Approximately 1–2 μL of gas is exchanged with each swallow.) Other functions of the ET with respect to the middle ear include: providing a pathway for drainage of secretions into the nasopharynx and protection from nasopharyngeal secretions and sound pressure.18,40,43,44 Obstruction of the ET, whether functional or mechanical, alters the partial pressure of middle ear gases, resulting in negative middle ear pressure, improper ventilation, and a supportive milieu for bacteria reproduction (Figure 7.1).5,12 Children are further disadvantaged because the pediatric ET is shorter and situated in a more horizontal orientation compared to adults, which inherently impairs its protective function.40
Notably important to understanding the part allergic inflammation plays in the development and persistence of OME is the concept of gas exchange in the ME.42 Nitrogen, oxygen, and carbon dioxide are the main gases involved in exchange in the ME. Oxygen and carbon dioxide equilibrate rapidly within the ME space with each swallow. However, since the partial pressure of nitrogen is lower in the surrounding ME tissues, it slowly diffuses out of the ME space.5,40,42 The ventilation of the ME space by the ET preserves atmospheric pressure and prevents the retraction of the tympanic membrane due to the evacuation of nitrogen.42 Disruption or breakdown of these protective functions of the ET results in increased risk for the development of OME.12
Pathophysiology
To appreciate the immunologic reactions within the ME system, a brief discussion of the factors involved in these reactions is warranted. Atopic disease is characterized by allergen exposure that causes rapid degranulation of mast cells, which results in the release of histamine, cysteinyl leukotrienes (CysLTs), prostaglandins (PGD), and cytokines.45 Some of these substances lead to the infiltration of inflammatory cells such as: eosinophils, basophils, neutrophils, mast cells, and mononuclear cells.46,47 These cells subsequently stimulate further release of histamine and CysLTs, thus perpetuating the inflammatory response by signaling recruitment of more inflammatory cells, which, in turn, increase mucosal blood flow, permeability of the vasculature, as well as stimulating mucus production.45,48 Within the ME system, chronic allergic inflammation is associated with a tenfold increase in the numbers of mast cells present in mucosa, which is coupled with higher numbers of IgE receptors and surface-bound IgE.49,50 In addition, mast cells are also thought to process and present allergens to antigen-presenting cells (B lymphocytes, monocytes, and dendritic cells). Allergen presentation in this environment is a potentially important source of cytokines, including interleukin 1 (IL-1), IL-6, and tumor necrosis factor (TNF).45 Mast cells, naïve T cells, and basophils also are thought to release IL-4. At a critical threshold, IL-4 induces an isotypic switching of the activated naïve T-cells to Th2 cells. The Th2 cell then produces copious amounts of IL-4, which mediates an isotype switch of B cells to IgE production, and causes upregulation of various adhesion molecules. These Th2 lymphocytes also release IL-5, IL-9, and IL-13, which further stimulate recruitment, production, and activation of basophils, eosinophils, and mast cells.45 The imbalance in the immune response between Th1 cells and Th2 cells has been proposed as the immunologic basis for allergic rhinitis as well as asthma. Numerous clinical studies have shown Th2 dominance with excess production of both IL-4 and IL-5 in patients with allergic rhinitis and asthma.38
▪ Middle Ear Space
Over the last 20 years, many authors have attempted to isolate the ME mucosa as a target organ, a site capable of significant immunologic activity to induce OME.18–22,51,52 Hurst et al and Wright et al have demonstrated eosinophils, myeloperoxidase, eosinophil cationic protein, and mast cells to be present in ME effusions of those with chronic OME, suggesting that the ME mucosa in atopics responds differently from nonatopics.20–2251 Ebmeyer et al showed that mast cells were a major contributor to the early inflammatory response of the ME to bacteria.53 Sobol et al found T lymphocytes, eosinophils, and other Th2 cytokines in the effusions of atopic children.22 Animal models have also attempted to demonstrate the reactivity of the ME mucosa. Hardy et al, Pollock et al, and Ebert et al have demonstrated ET dysfunction via transtympanic challenge of both allergens and histamine.54–56
Despite these data there is still not definitive evidence that the ME mucosa acts as the major target organ in the genesis of OME. Because reactivity to allergens requires repeated exposure, Bernstein and others have suggested that various mechanical factors of the Eustachian tube result in low levels of antigen contact and limited exposure times.42,48,57,58 Since the ET is the primary path for antigen delivery into the ME space and opens on a limited basis, i.e. swallowing or yawning, aerosolized antigens likely have restricted access to the ME.42 In addition, allergic inflammation of the nasal mucosa likely would result in edema of the torus tubaris, further isolating and actually protecting the ME space from direct contact with inhaled antigens. However, Bernstein suggests, in a small number of patients (<10%), the ME mucosa acts as a target organ.42
▪ Eustachian Tube
Allergic inflammation within or around the nasopharyngeal portion of the ET may lead to the loss of its protective functions resulting in increased risk for the development of OM and OME.12 Several mechanisms have been proposed to explain Eustachian tube obstruction due to inflammatory processes. First, poor ET function may result from a retrograde spread of edema secondary to congestion of the nasal mucosa. Second, poor mucociliary function may lead to impaired clearance of secretions and obstruction of the lumen of the ET.12,18 Third, direct allergic inflammation within the ET may cause obstruction due to intrinsic venous engorgement and hypersecretion of mucus, isolating the middle ear space, ultimately affecting gas exchange, and resulting in the diffusion of nitrogen out of the ME space and into the mucosa.48 The development of a net negative pressure in the ME develops perturbing cellular tight junctions and allows for a transudation of fluids into the middle ear space.42,48 The persistent obstruction of the Eustachian tube with mucus results in chronic ME inflammation, mucosal metaplasia, increased glandular activities of goblet cells, and an inability to clear ME fluid.42,48
▪ Nasopharynx and Nasal Mucosa
Numerous studies have supported the concept that allergic inflammation in the nose results in significant ET obstruction.17,38,42,59 In a study of 100 patients with recurrent OME, nearly one third of the cases were attributed directly to allergy. The authors concluded that the nasal allergic response in patients predisposed them to ET obstruction through the action of inflammatory mediators including cytokines released by mucosal mast cells, inflammatory cells, and epithelial cells in the nose and nasopharynx.12,42 In other studies, approximately 50% of patients with chronic OME presented with allergic rhinitis.17,37
In summary, there are four principle components of the ME system that are potential targets for allergic inflammation causing the development of OM and OME: ME space, ET, nasopharynx/adenoids, and the nasal mucosa. Of these sites, it is less understood how the ME space, with its limited physical exposure to inhaled antigens, could contribute to allergy-induced OME. By contrast, the ET, nasopharynx/adenoids, and the nasal mucosa all receive extensive airborne antigen exposure and the resulting edema, inflammation, and obstruction of the ET are all involved in the pathogenesis of OME.42
Additionally, the inflammatory response in one portion of the airway may also lead to inflammatory changes in other portions. For example, viral upper respiratory infections and/or a nasal allergic response result in a significant amount of increased nasal secretions and inflammation, which is maintained by subsequent inflammatory mediators and cytokines.14 It is thought that viral upper respiratory infections may encourage secondary bacterial infections by affecting bacterial adherence, modulating host immune and inflammatory responses throughout the airway, and possibly producing ETD, increased frequency of asthma or rhinosinusitis.14,45 In a study of atopic subjects, inhaled allergen challenge isolated to the nose produced inflammatory changes including increased adhesion molecules, increased bronchial hyperactivity, and eosinophil infiltration in both the upper and lower airways.45,60 This supports the concept that an intimate relationship exists between the upper and lower airways, whereby allergic inflammation is not isolated to a specific site or target organ but affects the common airway.8,9,14,23,24,45
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree