Chapter 3 Management of the Patient with Rhinitis
Types of Rhinitis
Rhinitis has traditionally been classified into two broad categories: allergic rhinitis, which implies a rhinitis primarily related to immune-mediated inflammation; and nonallergic rhinitis, which implies a nonimmune mechanism that triggers the patient’s symptoms. While much is understood and has been written about the pathophysiology, diagnosis and treatment of allergic rhinitis, a relative paucity of information is present for nonallergic rhinitis. In addition, many patients experience symptoms that are triggered by both immune and nonimmune mechanisms, and these patients are often classified as having mixed rhinitis, with characteristics of both allergic and nonallergic disease. Recognizing both allergic and nonallergic patterns in rhinitis is essential for the clinician in recommending appropriate treatment plans for patients experiencing nasal symptoms (Box 3.1).
It is clear that patients with nasal symptoms can have other sources for their symptoms than purely inflammation. Lund et al have recently suggested a classification of rhinitis into four types: structural; infectious; allergic; and “other.”1 This system recognizes that anatomic and infectious factors may also play a role in the expression of symptoms among patients. Structural rhinitis, for example, involves the presence of anatomic abnormalities such as deviation of the nasal septum and hypertrophy of the inferior turbinates that can interfere with air flow through the nose. Infectious rhinitis includes both acute and chronic rhinosinusitis, which have significant impact on nasal inflammation and nasal symptoms. In fact, current classification schemes do not differentiate infectious rhinitis from infectious rhinosinusitis, recognizing the key role that nasal disease plays in the sinus pathology among these patients. The remaining two categories in the system devised by Lund et al, allergic rhinitis and “other” rhinitis, correspond to the categories of allergic and nonallergic rhinitis discussed above. While nasal obstruction due to anatomic deformity or variability can be important, surgical management of these conditions is beyond the scope of the present textbook. The management of patients with acute and chronic rhinosinusitis is presented in Chapter 4.
▪ Allergic Rhinitis
The term allergic rhinitis (AR) refers to a condition manifested by nasal inflammation, and triggered by an immunologic response of the nasal and sinus mucosa. This immunologic response is primarily mediated by immunoglobulin E (IgE), and expressed through the influence of a number of humoral and cellular mediators. AR has traditionally been divided into two categories based upon the temporal course of the development and presentations of the symptoms: seasonal allergic rhinitis (SAR), which refers to immune-mediated nasal symptoms triggered by seasonal increases in environmental antigens, such as tree, grass and weed pollens and outdoor molds; and perennial allergic rhinitis (PAR), which refers to nasal symptoms occurring throughout the year, and generally attributed to indoor antigens such as animal dander, dust mites, cockroach, and indoor molds.2
Seasonal Allergic Rhinitis (SAR)
In most parts of the developed world, there are three distinct times of the year in which patients with SAR may become symptomatic. These three times of symptom expression correspond to the periods at which various plant families pollinate, and can broadly be correlated with the spring, summer, and fall seasons. As a general rule, in more temperate climates these pollen seasons are relatively distinct, with tree pollen commonly present in the spring, grass pollen in the summer, and weed pollen in the fall. In addition, mold spores are often present in warmer weather, and can be present for much of the year in warmer and more humid climates.
ARIA Classification of Allergic Rhinitis
While most of the literature on the diagnosis and treatment of allergic rhinitis has utilized this dichotomous classification based on seasonality of symptoms, expert opinion has recently suggested a new system for the classification of AR. This approach, which is based upon the chronicity and severity of symptoms of AR, was presented through a report entitled the ARIA Guidelines (Allergic Rhinitis and Its Impact on Asthma).3 The ARIA report suggests that a similar system should be used for the classification of allergic rhinitis to that used in classifying asthma.
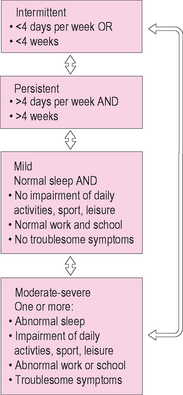
The ARIA approach has four diagnostic categories that are used to classify the severity and chronicity of symptoms: (1) mild intermittent AR; (2) moderate-severe intermittent AR; (3) mild persistent AR; and (4) moderate-severe persistent AR (Figure 3.1). In this system, chronicity is divided into two categories: intermittent and persistent. Intermittent AR is defined as a symptomatic period lasting less than 4 days a week or less than 4 weeks a year. Persistent AR is defined as symptomatic periods lasting more than 4 days a week and occurring more than 4 weeks a year. In classifying the severity of rhinitis, the ARIA system defines two levels based upon the clinician’s assessment of the impact of rhinitis symptoms on daily function, sleep, or quality of life. Mild disease is characterized by symptoms that are bothersome to the patient, but do not cause significant impact on sleep, daily function, or quality of life. Moderate-severe disease differs from mild disease, in that it is characterized by symptoms that interfere with daytime function, adversely impact sleep quality or duration, or cause a decrease in global or disease-specific quality of life. Based upon an evaluation of severity and chronicity, the ARIA guidelines suggest a pattern of pharmacologic and nonpharmacologic interventions.
▪ Nonallergic Rhinitis
Nonallergic rhinitis, in contrast to allergic rhinitis, refers to nonimmune-mediated nasal inflammation or irritation that promotes nasal symptoms such as congestion and rhinorrhea. Nonallergic rhinitis is a syndrome that cannot be explained by any uniform or consistent pathophysiologic mechanism. This condition involves many differing physiologic processes, and is often considered a “diagnosis of exclusion” among patients with nasal symptoms. Various triggers for the expression of nonallergic symptoms in the nose include infection, hormonal variability, pharmacologic agents, and autonomic dysregulation.4
Bachert recently divided nonallergic rhinitis into five categories based on their underlying etiology. He described these five categories as: (1) irritative-toxic (occupational) rhinitis; (2) hormonal rhinitis; (3) drug-induced rhinitis; (4) idiopathic (vasomotor) rhinitis; and (5) other forms (e.g., nonallergic rhinitis with eosinophilia (NARES)).5 Bachert provided specific information regarding the mechanisms and triggers for these various types of nonallergic rhinitis.
Drug-induced Rhinitis
Bachert notes that many medications can affect nasal physiology. Many classes of medications, including angiotensin-converting enzyme (ACE) inhibitors, beta-blockers and other antihypertensive agents, oral contraceptives, psychotropic medications, topical nasal decongestants, nonsteroidal anti-inflammatory medications, and phospodiasterase type-5 inhibitors (PDE-5) have been shown to have effects on the nose (Box 3.2).
Nonallergic Rhinitis with Eosinophilia (NARES)
Patients with NARES present with paroxysmal sneezing episodes, profuse watery rhinorrhea, nasal pruritis, nasal congestion, and hyposmia/anosmia. In contrast to allergic rhinitis patients, however, these patients fail to demonstrate any evidence for allergy on testing, yet have numerous eosinophils on nasal smears.6 Although its etiology is unknown, NARES shares clinical characteristics with Samter’s triad (aspirin sensitivity, asthma, and nasal polyposis), and may reflect a variant of that disease.
Epidemiology and Burden of Rhinitis
Overview
As noted above, rhinitis can be defined as an inflammatory or irritative disorder of the nasal membranes. Rhinitis presents with a pattern of symptoms that usually includes sneezing, nasal itching, rhinorrhea, and nasal congestion.7 In addition, patients with rhinitis will often complain of changes in the sense of smell, facial pressure or fullness, headache, and aural blockage. During periods of increased symptoms, patient with rhinitis experience a significant impact on both function and quality of life.
While nasal symptoms of rhinitis can be bothersome to patients and significantly interfere with normal function, the comorbidities of rhinitis can be quite serious and even life-threatening. Rhinitis represents inflammation in one part of the respiratory system, and can be associated with other common and serious respiratory illnesses such as rhinosinusitis and asthma.8 In fact, among patients with asthma, the prevalence of rhinitis in that population approaches 90%.9 In addition, rhinitis appears to play a role in the severity of symptoms among individuals with obstructive sleep apnea.10 Furthermore, the treatment of patients with chronic rhinosinusitis is often less successful among patients with allergic rhinitis than it is among their nonallergic counterparts. Because of its functional impairment and its serious comorbidities, rhinitis is therefore not a trivial disease, but one that can have serious medical and functional consequences.
Burden of rhinitis
The economic impact of rhinitis is significant. Direct costs annually attributable to the treatment of allergic rhinitis alone were estimated in 2003 to range between US$2 and 5 billion.11 In addition, the indirect costs of AR significantly contribute to the economic burden of the disease, with an estimated US$5–10 billion annually attributable to the morbidity of this common disease.11 In another recent estimate, over US$6 billion was outlayed specifically for prescription medications used for treating the symptoms of allergic rhinitis.12 Worldwide treatment of rhinitis would certainly account for a significant increment in these US figures.
In addition to the direct and indirect financial costs of allergic and nonallergic rhinitis, quality of life, daytime function, and sleep are frequently compromised among patients, not only by the disease states but also by treatments whose adverse effects further adversely impact function. Patients with allergic and nonallergic rhinitis experience a wide range of cognitive and social issues that can be disruptive in their daily activities and interpersonal relationships. Fatigue, confusion, distractibility and other cognitive symptoms are common among patients with rhinitis, and can be worsened by treatment with pharmacologic agents such as sedating antihistamines. Among children with allergic rhinitis similar effects can be seen, resulting in decrements in learning and attention in the classroom.13 In addition, patients with AR experience disruption in normal patterns of sleep, which can contribute to daytime symptoms.14
Prevalence of Rhinitis
Allergic and nonallergic rhinitis are common illnesses. Prevalence studies worldwide suggest that the rates of AR within the population vary between 10% and 20%.15,16 It has been reported that 58 million Americans annually experience symptoms of allergic rhinitis, while 19 million Americans experience symptoms of nonallergic rhinitis.15 As was noted earlier, many patients have both nonallergic and allergic triggers for their symptoms. This mixed rhinitis can occur in up to 44% of patients with AR.15
In addition to these absolute values, there is evidence that the prevalence of AR is increasing. Several studies have shown that the rates of AR have increased at least twofold over the past two decades.17,18 While several hypotheses have been suggested to explain this increasing prevalence, the reasons for this steady increase remain speculative.
Managing the Patient with Allergic Rhinitis
▪ Pathophysiology
Allergic rhinitis is an immune-mediated inflammatory condition that affects the mucosa of the nose, paranasal sinuses, and related mucosal structures. The primary mechanism underlying AR involves a type-I hypersensitivity reaction that is directed by various cellular and humoral agents. It is mediated through processes under the control of T-helper 2 cells, and involves a complex interaction of various inflammatory mechanisms. A full review of the immunology of the allergic response is presented in Chapter 1.
The allergic response in the nose is initiated when individuals come into contact with antigens to which they have been previously sensitized. IgE molecules that had been synthesized during the sensitization process to these antigens are present on the surface of mast cells, and have specific determinants available to bind to these antigens. When antigen particles bind to adjacent IgE molecules, a sequence of biochemical events occurs, resulting in degranulation of mast cells and release of preformed mediators such as histamine into the nasal tissues. This process of degranulation and histamine release is the primary process responsible for initiation of the immediate allergic response.19
Histamine binds to specific histamine-1 (H1) receptors on the surface of target cells in the nose, leading to local effects in the nasal mucosa, including transudation of plasma, engorgement and edema of the mucosa, stimulation of mucous glands to produce increased mucus secretions, and other direct inflammatory events.20 In addition, histamine, as well as other mediators and neuropeptides released during the allergic response, cause stimulation of fine sensory nerves in the nasal mucosa, resulting in irritative effects such as sneezing and itching (Figure 3.2).2 These events occur rapidly after exposure to a sensitized antigen, often leading to the development of symptoms within 5–10 minutes of contact. Symptoms of allergic rhinitis, such as sneezing, itching, rhinorrhea, and nasal congestion, occur as a result of these inflammatory processes that occur after exposure, and characterize the “early-phase” response to allergic stimulation.
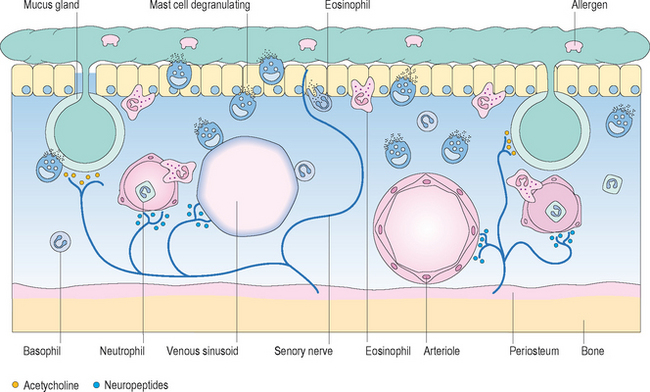
Figure 3.2 Acute-phase mucosal response to antigen.
(Reproduced with permission from Holgate ST. Allergy, 2nd edn, figure 4.9, p. 59, published by Mosby, 2001.)
In addition to these immediate effects that occur rapidly after exposure, a second, delayed process of inflammation occurs in many patients with AR. This delayed expression of nasal symptoms is referred to as the “late-phase” response, and results in expression of symptoms at 2–4 hours after exposure or more. While the early phase response occurs primarily as a response to histamine, the late phase response is directed by other mediators such as cysteinyl leukotrienes and inflammatory cells such as eosinophils and basophils.2 An appreciation of this biphasic response in AR is important in understanding the method of presentation among patients with AR and various treatment options specific for these inflammatory processes.
▪ Presentation
While allergic rhinitis can develop at any age, the majority of patients with allergic rhinitis first present with symptoms in middle childhood. Recent prevalence data suggest that up to 40% of children may express symptoms of AR in early childhood.21 Other studies suggest that the mean age for diagnosis of allergic rhinitis is between the ages of 9 and 11 years.16 Symptoms tend to be experienced most significantly among patients between 10 and 40 years of age, and decline somewhat thereafter. It is uncommon for patients under age 2 to experience symptoms related to allergic rhinitis. In addition, while patients may first express symptoms of allergic rhinitis in their older years, the onset of rhinitis symptoms among patients older than 55 years of age would strongly favor a diagnosis of nonallergic rhinitis.
In addition, due to the significant mucosal inflammation of the nasal and sinus membranes, and due to their concurrent nasal obstruction and congestion, many patients with both AR will report a decreased sense of smell or taste, facial pressure or pain, and temporal or frontal headache.22 These symptoms of pressure and anosmia are also common among patients with chronic sinonasal polyposis and acute and chronic rhinosinusitis.
In patients with SAR, the waxing and waning of symptoms follows the pollen counts during those seasons in which the patient has allergic sensitization to the pollens present in the environment. These symptoms will usually lag for a few days following the seasonal pollen fluctuations, and can be blunted by the use of various medications. This seasonal change in patient symptoms offers an important element of the clinical history that can be used by the clinician in confirming a diagnosis of allergic rhinitis. Seasonal changes in chronically stable symptoms among patients with PAR also suggest a seasonal component to the patient’s PAR.
In those patients with PAR, symptoms are generally present throughout all seasons of the year. The diagnosis of PAR based on history alone can often be more difficult than that of SAR due to the absence of a clear seasonality to the patient’s symptoms. In addition, patients with PAR often experience a somewhat different cluster of symptoms than those noted by the patient with SAR. Among patients with PAR, nasal obstruction and postnasal drainage appear more commonly than the sneezing and itching often seen more frequently among patients with SAR.22 In addition, since both chronic rhinosinusitis and nonallergic rhinitis can have similar symptom patterns to PAR, it can be difficult to diagnose PAR without confirmatory testing.
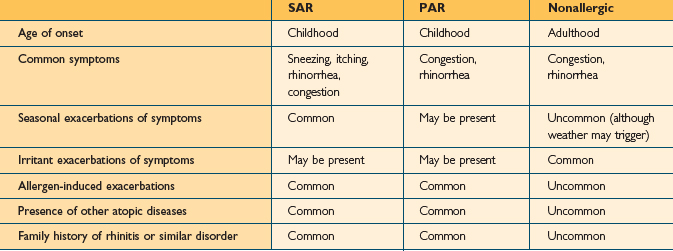
While AR and nonallergic rhinitis both present with symptoms related to nasal inflammation and irritation, the pattern of symptoms is usually different in the two conditions. The type of symptoms noted in patients with nonallergic rhinitis depends on the pathophysiological processes involved and the mechanisms of nasal irritation or inflammation. For example, patients with vasomotor rhinitis present predominantly with clear rhinorrhea, while those with rhinitis of pregnancy present with congestion. The presentation of patients with nonallergic rhinitis will be discussed later. Table 3.1 displays some common differences between the presentations of patients with AR and nonallergic rhinitis.
▪ Diagnosis
History
The evaluation of the patient with symptoms of rhinitis in large part depends on a thorough and careful history. Patients with both allergic and nonallergic rhinitis will present with characteristic symptoms that can be elicited through the history. In addition, the patient’s history can often distinguish AR from nonallergic rhinitis (Table 3.1).
While not all patients with AR complain of seasonal triggers or fluctuations related to time of the year, seasonal variability of the patient’s nasal symptoms is also important to assess. The symptoms of SAR demonstrate a clear relationship with the increase of pollen in the environment during discrete seasons of the year. This variability of symptoms is an important component of the history among patients with rhinitis, and suggests a diagnosis of SAR. Patients with PAR may also have a seasonal worsening of symptoms, but will have significant symptoms between traditional pollen seasons. Many patients with AR will present with complaints characteristic of both SAR and PAR.
Physical Examination
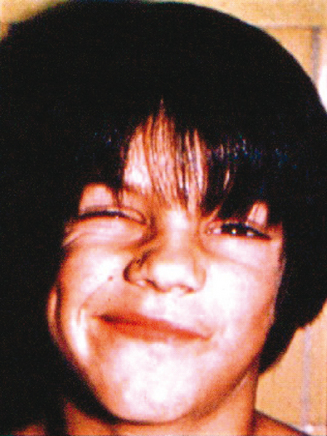
The physical examination of the patient with symptoms of rhinitis involves not only a careful evaluation of the nose itself, but also a comprehensive evaluation of the head, neck, and chest as well. The physical examination begins with an inspection of the face. The clinician will examine the face for external signs suggesting nasal inflammation. These signs include facial puffiness, edema, facial asymmetry, or infraorbital discoloration (Figure 3.3). The eyes are examined for evidence of conjunctival injection, irritation or erythema. Infraorbital darkening of the skin implies venous stasis due to nasal congestion. Allergic patients often demonstrate fine creases in the eyelids, noted as Dennie’s lines. These fine creases occur due to spasms of Mueller’s muscles, and are often seen in children with AR.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree