Chapter 12 Management of the Patient with Occupational Allergy
Introduction
Occupational allergy causes considerable morbidity and mortality, posing a great burden to society in terms of disability, health care costs, and time off work. In the USA there are an estimated 14.6 million work absence days due to asthma alone annually.1 Some of the common conditions caused by occupational allergies include occupational asthma, hypersensitivity pneumonitis, latex rubber allergy, and allergic contact dermatitis. The greatest challenge is to be able to distinguish occupational allergy from non-work-related allergic conditions. This chapter will focus on the characteristics of occupational allergies that will help to differentiate occupational from non-work-related causes. One of the effective ways to reduce the burden of occupational allergy is to prevent the exposure and sensitization to occupational allergens in susceptible workers, but it is equally important to prevent long-term complications by recognizing and treating these conditions early once they have occurred. Failure to recognize occupational asthma can lead to chronic symptoms, disability, absenteeism from work, and increased health care costs. Similarly delayed detection of hypersensitivity pneumonitis can lead to irreversible pulmonary fibrosis and long-term disability. In this chapter discussion will be limited to occupational asthma, hypersensitivity pneumonitis, latex allergy, and allergic contact dermatitis, which are some of the commonest occupational allergic conditions.
Prevalence
According to the Asthma and Allergy Foundation of America the annual cost of asthma is estimated to be US$18 billion, it is the fourth leading cause of work absenteeism with nearly 15 million missed or lost workdays each year and a total cost of nearly 3 billion in lost productivity.2 Work-related asthma is the most commonly reported occupational lung disease in the USA. In the USA 10–25% of adult asthma is either initiated or aggravated by work, with incidence rates of 29–710 cases per million workers per year.3 In the UK it is estimated occupational asthma accounts for 2–6% of adult asthma,4 and other population-based studies in Europe have estimated it to be between 5% and 10%. The occupations at highest risk for occupational asthma are farmers, painters, plastic workers, cleaners, spray painters, and agriculture workers.5 Latex-induced asthma is an important cause of asthma in health care workers.
The prevalence of hypersensitivity pneumonitis is unknown, due in part to the lack of standard diagnostic criteria and partly because it has so many causes. According to NIOSH Occupational Respiratory Disease Surveillance the number of deaths from hypersensitivity pneumonitis has been increasing from less than 20 per year in 1979 to 57 in 1999.6 Many agents can cause hypersensitivity pneumonitis and its development depends on the size and nature of the antigen, the concentration of the antigen, the duration of exposure, and the frequency of repeated exposures. It is interesting to note that research shows hypersensitivity pneumonitis occurs more frequently in nonsmokers than smokers.7
The prevalence of latex sensitization in the general population ranges between 5% and 10%. Clinical associations have also been found between latex and certain fruits and vegetables such as kiwi, banana, chestnut, avocado, lettuce, tomato, and potato. Because of this, latex allergy may follow fruit or vegetable allergy or vice versa.8 Occupations at highest risk to latex allergy include health care workers (nurses, doctors, dentists, operating room staff, laboratory technicians) and workers in the latex industry. One study reported a prevalence of 11% for positive skin tests to latex in a surgical glove manufacturing plant.9 In another study the prevalence of latex sensitization among health care workers at two hospital sites was found to be 12.1%.8 The amount of latex needed to produce sensitization is unknown, and no safe occupational exposure limit has been established for latex protein.
In the USA skin diseases and disorders accounted for 13% (57 900 cases) of all nonfatal occupational illness cases in private industry reported in 1997. Of these there were 6600 cases of dermatitis that involved time away from work. Workers with dermatitis had a median of 3 days off from work. Service and manufacturing industries each were the cause of 29% of the cases of dermatitis with days away from work. Laborers, fabricators, precision production workers, repair personnel and craft workers are the workers most commonly affected by dermatitis with time away from work.10 In the work setting hands are the most often affected part of the body, either alone or with other parts of the body. The hands are involved in 80–90% of cases of occupational dermatitis.11
Epidemiology
▪ Work-related Asthma
Work-related asthma is classified as either occupational or work-aggravated asthma. Workplace exposures can cause new onset asthma or exacerbate pre-existing asthma. Occupational asthma is defined as new onset asthma, which is caused by workplace exposures. There are two subtypes of occupational asthma, sensitizer-induced asthma that has a latency period and is due to immunologic mechanisms and irritant-induced asthma that has no latency period and occurs after high-intensity exposures to irritating agents. The latency period can vary from weeks to years. Reactive airways dysfunction is a discrete subset of irritant-induced asthma. Pre-existing asthma that is worsened by workplace exposures is called work-aggravated asthma. In this chapter the focus will be on sensitizer-induced asthma, which is characterized by variable airflow limitation or bronchial hyperresponsiveness, or both induced by agents in the workplace.
▪ Hypersensitivity Pneumonitis
Hypersensitivity pneumonitis is an immunologically mediated parenchymal lung disease which involves the alveolar walls and terminal bronchioles. It is caused by inhalation of organic dusts. The clinical picture and pathology of hypersensitivity pneumonitis is the same regardless of the cause. Many different dusts are know to cause hypersensitivity pneumonitis but the mechanism of disease is not clearly understood. Specific IgG antibodies against the dust involved seem to be necessary. However, this is not sufficient on its own to explain the symptoms, as not all inviduals with antibodies develop disease. Repeated exposure to the antigen causes sensitization followed by immunologically mediated damage to the lungs. Many agents can cause hypersensitivity pneumonitis. The major categories of antigen include animal/insect proteins, microbial agents (bacteria, fungi), and low molecular weight agents. The clinical presentation can be acute, subacute, or chronic. Some of the causes of hypersensitivity pneumonitis are listed in Table 12.1.
TABLE 12.1 Some of the causes of hypersensitivity pneumonitis
| Disease | Source of antigen | Antigen |
|---|---|---|
| Bird fancier’s lung | Pigeon, parakeet, dove, duck | Avian proteins |
| Furrier’s lung | Animal pelts/cat hair | Dust from fur/cat hair |
| Farmer’s lung | Moldy hay, silage, grain | Thermophilic actinomycetes |
| Woodworker’s disease | Cedar, oak, mahogany, pine, spruce | Alternaria spp. |
| Tobacco grower’s lung | Tobacco leaves | Tobacco dust |
| Coffee worker’s lung | Coffee bean dust | Coffee dust |
| Bagassosis | Moldy sugar cane | Thermoactinomyces sacchari |
| Malt worker’s lung | Moldy malt | Aspergillus clavatus |
| Cheese worker’s lung | Moldy cheese | Penicillum casei |
| Oyster shell lung | Shell dust | Oyster shell protein |
| Tea grower’s lung | Tea leaves | Tea dust |
| Mushroom worker’s lung | Moldy mushroom | Thermoactinomyces sacchari |
| Pauli’s reagent alveolitis | Laboratory reagent | Pauli’s reagent |
| Pyrethrum lung | Insecticide | Pyrethum |
| Epoxy resin worker’s lung | Adesive, foam, resin | Phthalic anhydride |
| Drug-induced alveolitis | Medications | E.g. sulfasalazine, nitrofurantoin |
| Plastic worker’s lung | Plastic | Trimellitic anhydride |
| Humidifier lung | Contamined forced air system | Saccharopolyspora rectivirgula, Thermoactinomyces vulgaris |
| Chemical worker’s lung | Urethane paint catalyst | Diphenylmethane diisocyanate |
▪ Contact Dermatitis
Contact dermatitis can be divided into allergic or irritant types. Up to 80% of cases of contact dermatitis are due to irritants. Irritants cause dermatitis by nonimmunologic reactions whereas allergens cause dermatitis by delayed hypersensitivity immunologic reactions. It is difficult to differentiate the irritant from allergic contact dermatitis clinically. Chemicals are the most important cause of occupational skin disease followed by mechanical, physical, and biological agents. Individuals may develop contact dermatitis to most chemicals if they are exposed to the chemical in sufficient quantities for an adequate period of time. Chemicals cause approximately 53% of work-related dermatitis.10 In humans more than 3000 chemicals have been implicated in contact dermatitis. Poison ivy and oak are the commonest cause of allergic contact dermatitis followed by chrysanthemums and compositae species (Figure 12.1). Horticulturists, farmers, loggers, foresters, florists, and nursery workers are at risk of developing phytodermatitis from contact with allergens from plants.
Anatomy and Physiology
The average adult has approximately 18 square feet of skin, which consists of the outer epidermis and the deeper dermis. The outermost layer of the superficial epidermis is the keratin layer (stratum corneum), which is made up of nonviable anucleate cells. Deep to this layer there are the stratum spinosum and the basal (germinative) layers. The germinative layer produces epidermal cells that move up and transform into the flat, compact, and dehydrated keratinized cells of the stratum corneum. The stratum corneum is a protective barrier of the skin preventing internal tissues from exposure to chemicals, toxins, ultraviolet radiation, bacteria, and extreme temperatures. It is thickest on the palms of the hands and the soles of the feet, so that hand dermatitis mainly affects the dorsal aspect rather than the palms. The keratin layer allows lipophilic chemicals to be absorbed more so than hydrophilic substances. Permeability of the skin is increased if waterproof materials such as gloves cover the skin, and if the skin has abrasions or is inflamed. The deeper layers of the epidermis contain the Langerhans cells, which are dendritic antigen-presenting cells, that are necessary for allergic contact dermatitis to take place. Melanocytes in the epidermis produce the pigment melanin, which protects against ultraviolet radiation. The dermis is mainly made of collagen in a ground substance and this makes the skin strong and flexible. The dermis contains blood vessels, lymphatic drainage, nerves, and epidermal appendages.12
Pathophysiology
▪ Occupational Asthma
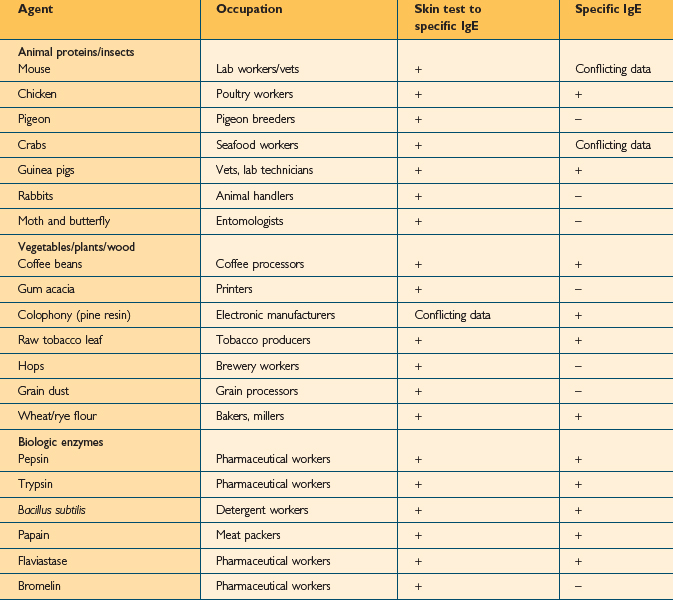
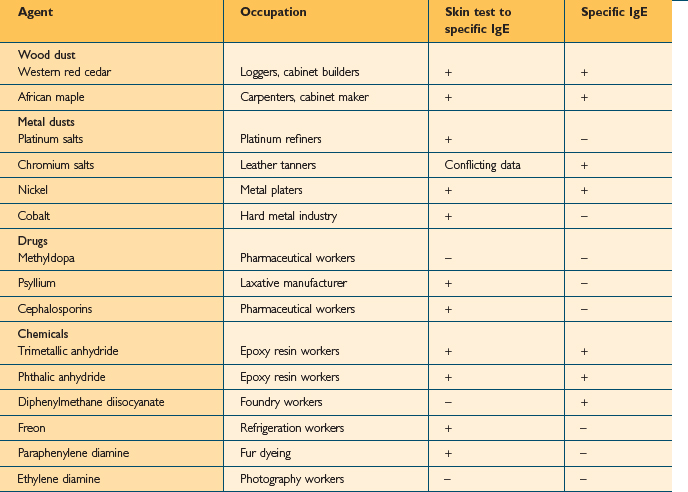
Over 350 agents are known to trigger occupational asthma.3 Sensitizing agents that cause occupational asthma can be divided into high-molecular weight compounds (>5000 Daltons) and low-molecular weight compounds (<5000 Daltons). High molecular weight compounds such as plant proteins act as complete antigens and cause the production of specific IgE antibodies (Table 12.2). The mechanism for low molecular weight compounds is unknown but certain low molecular weight compounds such as acid anhydrides probably act as haptens and bind with proteins to form functional antigens. Many low molecular weight agents, including isocyanate, do not consistently induce specific IgE antibodies (Table 12.3).
The first step in sensitizer-induced occupational asthma is the binding of the antigen with specific IgE receptors on the surface of mast cells, basophils, and possibly macrophages and eosinophils. These cells, after capturing the antigen migrate to the local lymph nodes and interact with naïve T cells (Th0) which differentiates into Th2 cells in the presence of interleukin (IL) 4 and other proinflammatory mediators. This leads to a cascade of events causing an influx of inflammatory cells into the airway and the subsequent release of inflammatory mediators. In addition to this, it stimulates isotype switching of B cells to antibody production of IgG and IgM to IgE. The IgE antibody produced by B cells circulates in the blood attaching to high affinity receptors on mast cells and low affinity receptors on basophils. Once the antigen binds with the IgE there is a release of granule stored mediators such as histamine and eosinophil/neutrophil chemotactic factors. Leukotrienes and prostaglandins are also released from membrane phospholipids. These mediators cause the symptoms of asthma such as edema and bronchoconstriction by affecting vascular permeability, smooth muscle tone, cell migration, and mucus production. Following sensitization, subsequent re-exposure to even minute quantities of allergen causes immediate symptom production which may be severe. The latency period for the development of sensitization can vary from weeks to years. However in order to produce sensitization the antigen concentration and duration of exposure has to be significant.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree