Chapter 53 Other optic neuropathies in childhood
Childhood optic neuritis
Pediatric neurologists must be involved in the management of childhood optic neuritis.
Optic neuritis
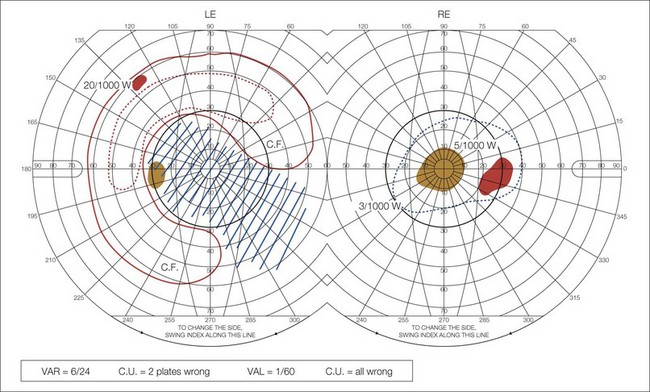
Although optic neuritis is diagnosed in children using the same clinical criteria as in adults (subacute visual loss, pain with eye movements, visual field defects, and a relative afferent pupil defect), diagnosis may be more difficult. Children find it difficult to articulate the typical history of optic neuritis and may not present until they are profoundly affected. They may complain that it is dark all the time or insist on keeping the house lights on even in daylight because of impaired brightness sense (Fig. 53.1). Perimetry or fields to confrontation often reveal a central scotoma (Fig. 53.2). The abnormal vision and difficulty navigating may be interpreted as poor gait. Input from a pediatric neurologist is important, because transverse myelitis may be the presenting feature of neuromyelitis optica (NMO) – see below. The conversion rate to multiple sclerosis in children is unclear due to a lack of adequately powered long-term studies. However, as with adults, T2 lesions on MRI scan are associated with an increased risk of developing MS.1–3
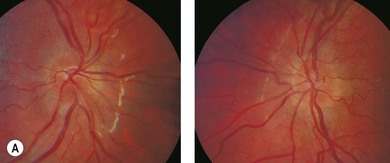
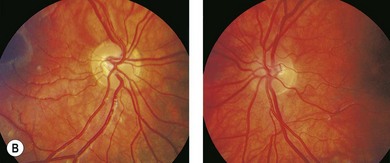
Factors that are associated with a reduced risk of developing MS include young age, bilateral optic neuritis, disk swelling (Fig. 53.3), and antecedent infection.
Neuromyelitis optica
Neuromyelitis optica (NMO) or Devic’s disease is a central nervous system inflammatory disorder that predominantly affects the optic nerves and spinal cord. It is a distinct entity, and in about 70% of cases it is associated with an NMO-IgG autoantibody which targets aquaporin-4 channels. AQP4 is expressed in the collecting duct cells in the kidneys and in astrocytes. It is upregulated by direct insult to the central nervous system. Aquaporins are involved in the conduction of water through cell membranes.4 The NMO-IgG antibody is not present in MS. Standard MS immunomodulatory treatment may not be effective. Plasmapheresis may be required if immunosuppression is ineffective. The primary goal of therapy is to prevent future attacks.
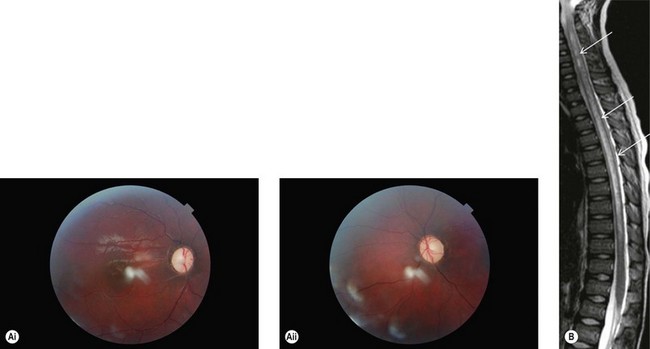
MRI does not usually show the periventricular white matter lesions seen in typical MS. It is important to specifically request imaging of the spinal cord to detect longitudinal myelitis involving ≥three segments (Fig. 53.4).
The diagnostic criteria for NMO are summarized in Box 53.1.
The disease is more prevalent in females than males (greater than 4 : 1 ratio). It is more prevalent among the Black, Asian, and Indian populations. In Europe NMO is very rare and the majority of cases are not associated with NMO-IgG autoantibodies.5
In the absence of AQP4 antibodies, the disease is more likely to be monophasic and long-term treatment with azothioprine, mycophenolate, or rituximab is usually not required.5
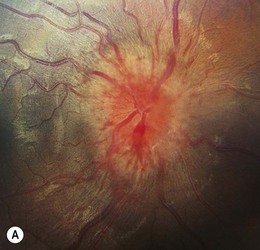
Neuroretinitis
Neuroretinitis is usually unilateral, occasionally bilateral. It is an inflammatory disorder characterized by optic disk edema and formation of a macular star (Fig. 53.5). The primary abnormality is inflammation and increased permeability of the optic disk vasculature, causing leakage of fluid into the peripapillary retina.6 The cause of this vasculitis is not clear: some cases have an infectious etiology, most commonly Bartonella henselae (cat scratch disease), also syphilis, tuberculosis, Lyme disease, leptospirosis, and toxoplasmosis.7