 Orbital Osseous, Fibro-osseous, and Cartilaginous Tumors
Orbital Osseous, Fibro-osseous, and Cartilaginous TumorsOrbital Osteoma
General Considerations
The main tumors of bone are the benign osteoma and the malignant osteosarcoma (1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23). Osteoma is the most common tumor of the nose and paranasal sinuses and the most common neoplasm of the frontal sinus. Osteoma that arises from the bones of the frontal sinus, ethmoid sinus, and other periorbital bones can extend into orbit. Osteoma in an ocular oncology practice are relatively uncommon (2,3,4,5,6). In the authors’ series of 1,264 orbital lesions, the 4 osteomas accounted for 19% of osseous and fibro-osseous tumors and for ,1% of all orbital tumors. The true incidence is actually greater, because most lesions originate in the sinuses, have minimal orbital involvement, and are more likely to be managed by otorhinolaryngologists.
Orbital osteoma can sometimes occur with Gardner syndrome, an autosomal-dominant condition characterized by adenomatous polyposis of the bowel, secondary bowel cancer, typical congenital hyperplastic lesions of the retinal pigment epithelium (RPE), desmoid tumors, and other lesions (8,18). The RPE lesions are discussed in the Textbook and Atlas of Intraocular Tumors. A patient with a suspected orbital osteoma should undergo ophthalmoscopy and possible referral to a gastroenterologist.
Clinical Features
Orbital osteoma can occur at any age and there is no predilection for gender. Depending on the size and location of the osteoma, it can be asymptomatic or can produce orbital symptoms and signs such as proptosis and displacement of the globe. Osteoma can cause pain, described by the patient as a headache. A hard mass may be visible and palpable at the superior or nasal orbital rim. The bony mass may obstruct the ostea of the sinus and lead to chronic sinusitis or secondary mucocele.
Diagnostic Approaches
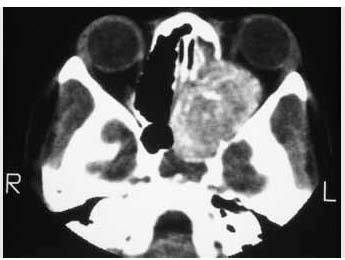
Computed tomography of orbital osteoma shows a sessile or pedunculated mass with bone density arising from otherwise normal bone, usually the frontal or ethmoid bones. The ivory type may be identical to bone; the fibrous type is less dense and may resemble fibrous dysplasia.
Pathology
Histopathologically, osteoma has been divided into three types: compact (ivory), cancellous, and fibrous (1,2,3,4). It is believed that the compact type is most mature and the fibrous the least mature and that the fibrous type may be part of a continuum incorporating ossifying fibroma and fibrous dysplasia (1,3).
Management
Asymptomatic orbital osteoma can sometimes be followed conservatively. The only exception is an osteoma of the sphenoid bone that shows encroachment on the optic canal, in which case earlier surgical excision may be justified. A larger or symptomatic osteoma can be managed by surgical excision. A superonasal lynch incision can be used for the more common superonasal lesion. For a more posterior osteoma that involves the orbital roof or cribriform plate, a combined orbitocranial approach can be employed. Bone instruments are required for this surgery. Incomplete removal does not usually lead to recurrence (4).
Selected References
1. Fu YS, Perzin KH. Non-epithelial tumors of the nasal cavity, paranasal sinuses, and nasopharynx: a clinicopathologic study. II. Osseous and fibro-osseous lesions, including osteoma, fibrous dysplasia, ossifying fibroma, osteoblastoma, giant cell tumor, and osteosarcoma. Cancer 1974;33: 1289-1305.
2. Shields JA. Osseous, fibro-osseous, and cartilaginous tumors. In: Shields JA, ed. Diagnosis and Management of Orbital Tumors. Philadelphia: WB Saunders; 1989:205-211.
3. Rootman J. Neoplasia. Osteoma. In: Rootman J, ed. Diseases of the Orbit. 2nd ed. Philadelphia: Lippincott, Williams & Wilkins; 2003:280-282.
4. Henderson JW. Tumors of orbital bone. In: Henderson JW, ed. Orbital Tumors. 3rd ed. New York: Raven; 1994:161-164.
5. Shields JA, Bakewell B, Augsburger JJ, et al. Classification and incidence of space-occupying lesions of the orbit. A survey of 645 biopsies. Arch Ophthalmol 1984;102:1606-1611.
6. Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: the 2002 Montgomery Lecture, part 1. Ophthalmology 2004;111:997-1008.
7. Ataman M, Ayas K, Gursel B. Giant osteoma of the frontal sinus. Rhinology 1993;31:185-187.
8. Whitson WE, Orcutt JC, Walkinshaw MD. Orbital osteoma in Gardner’s syndrome. Am J Ophthalmol 1986;101:236-241.
9. Van Gehuchten D, Lemagne JM, Weber S, et al. A case of exophthalmos-an early symptom of Gardner’s syndrome. Orbit 1982;1:61-69.
10. Appalanarsayya K, Murthy ASR, Viswanath CK, et al. Osteoma involving the orbit. Case report and review of the literature. Int Surg 1970;54:449-453.
11. Borello ED, Argentina R, Sedano HO. Giant osteoid osteoma of the maxilla. Oral Surg 1967;23:563-566.
12. Blodi FC. Pathology of orbital bones. The XXXII Edward Jackson Memorial Lecture. Am J Ophthalmol 1976;81:1-26.
13. Selva D, White VA, O’Connell JX, et al. Primary bone tumors of the orbit. Surv Ophthalmol 2004;49:328-342.
14. Selva D, Chen C, Wormald PJ. Frontoethmoidal osteoma: a stereotactic-assisted sino-orbital approach. Ophthal Plast Reconstr Surg 2003;19: 237-238.
15. Kim AW, Foster JA, Papay FA, et al. Orbital extension of a frontal sinus osteoma in a thirteen-year-old girl. JAAPOS 2000;4:122-124.
16. Ma’luf RN, Ghazi NG, Zein WM, et al. Orbital osteoma arising adjacent to a foreign body. Ophthal Plast Reconstr Surg 2000;19:327-330.
17. Grove AS. Osteomas of the orbit. Ophthalmic Surg 1978;9:23-39.
18. McNab AA. Orbital osteoma in Gardner’s syndrome. Aust N Z J Ophthalmol 1998;26:169-170.
19. Miller NR, Gray J, Snip R. Giant mushroom-shaped osteoma of the orbit originating from the maxillary sinus. Am J Ophthalmol 1977;83:587-591.
20. Newell FW. Osteoma involving the orbit. Am J Ophthalmol 1948;31: 1281-1289.
21. Sternberg I, Levine MR. Ethmoidal sinus osteoma: a primary cause of nasolacrimal obstruction and dacryocystorhinostomy failure. Ophthalmic Surg 1984;15:295-297.
22. Tarkkanen JV, Mets LP. A case of orbital osteoma. Acta Ophthalmologica 1964;42:1074-1078.
23. Thakur V, Nema HV. Osteoma of the lesser wing of the sphenoid. Eye Ear Nose Throat Mon 1969;48:619-621.
Orbital Osteoma
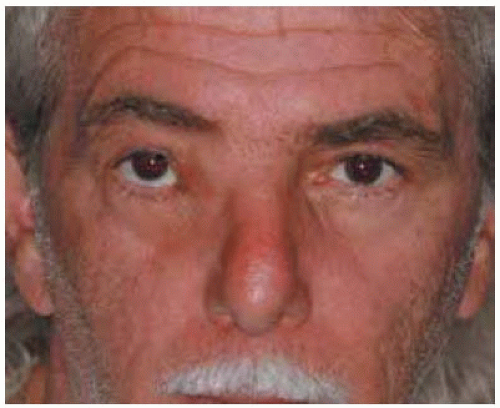 Figure 33.1. Photograph of a 60-year-old man with slowly progressive hard mass in region of right medial canthus. |
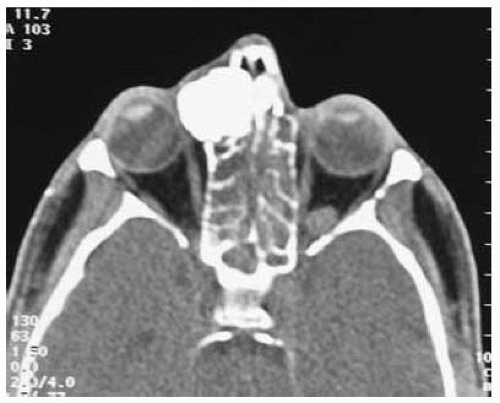 Figure 33.3. Axial computed tomography shows bone density mass in medial aspect of anterior orbit, nasal cavity, and ethmoid sinus. |
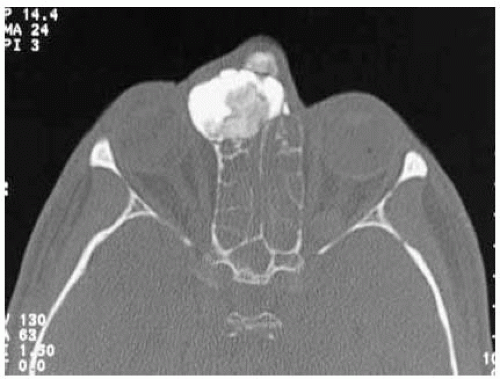 Figure 33.4. Axial computed tomography in bonew indow setting, showing heterogeneous mass with bone density. |
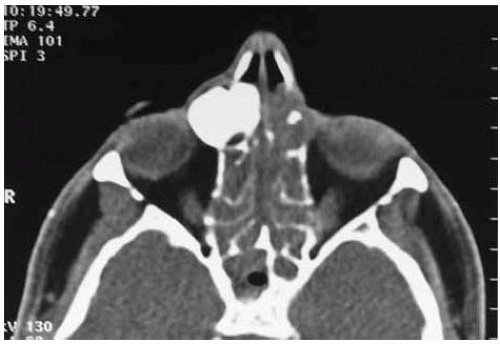 Figure 33.5. Axial computed tomography at a slightly higher level. Note opacity in the contralateral ethmoid sinus. It is uncertain whether the sinusitis is primary or secondary to the osteoma. |
Orbital Osteoma: Clinicopathologic and Imaging Correlation and Occurrence in Gardner Syndrome
Whitson W E, Orcutt JC, Walkinshaw M D. Orbital osteom a in Gardner’s syndrome. Am J Ophthalmol 1986;101:236-241.
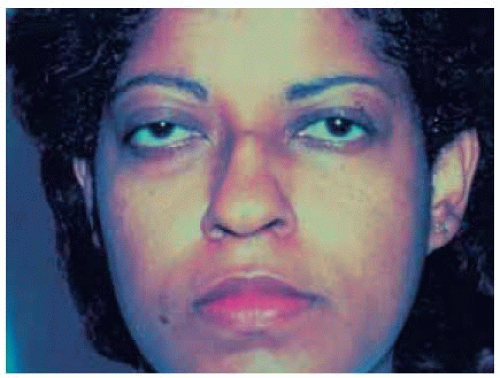 Figure 33.7. Orbital osteoma. Proptosis of the right eye in a 26-year-old wom an. (Courtesy of Pearl Rosenbaum , M D, and Thom as Slam ovitz, MD.) |
 Figure 33.8. Patient shown in Figure 33.7 demonstrating limitation of supraduction of right eye. (Courtesy of Pearl Rosenbaum , M D, and Thomas Slamovitz, MD.) |
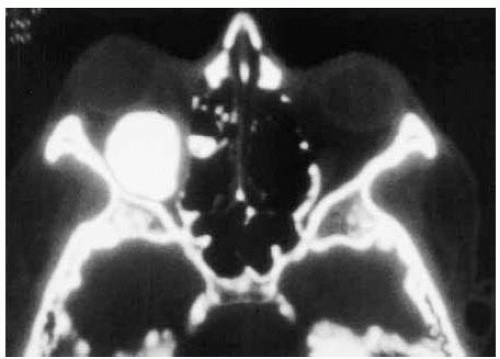 Figure 33.9. Axial computed tomography of patient shown in Figure 33.7 demonstrating a dense mass involving the orbital roof and part of the ethmoid sinus. (Courtesy of Pearl Rosenbaum , M D, and Thomas Slamovitz, MD.) |
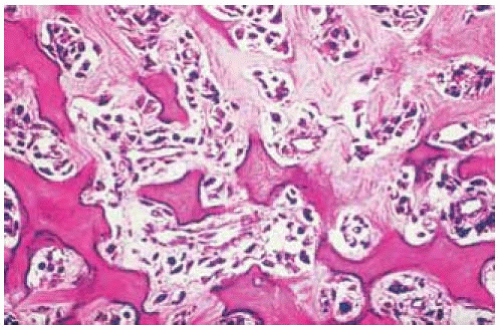
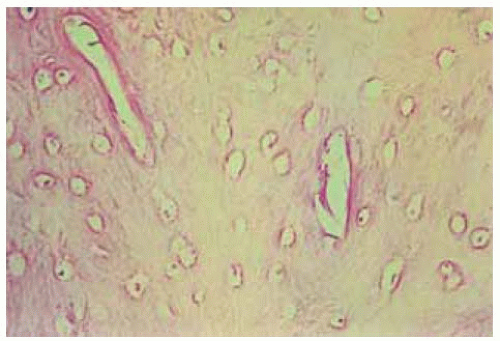 Figure 33.10. Histopathology of lesion shown in Figure 33.9 demonstrating compact bone and minimal fibrous stroma. (Hematoxylin-eosin 50.) (Courtesy of Pearl Rosenbaum, MD, and Thomas Slamovitz, MD.) |
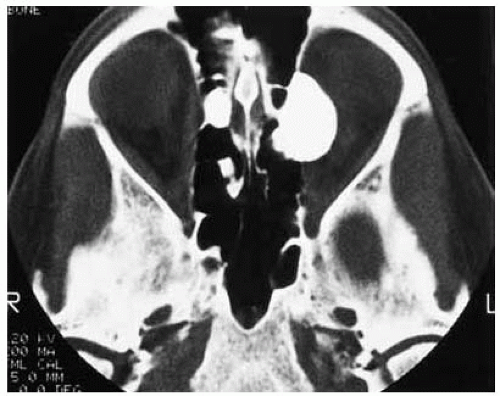 Figure 33.11. Orbital osteoma in Gardner syndrome. Axial computed tomography showing large bone density mass originating from the medial orbital wall. (Courtesy of James Orcutt, MD.) |
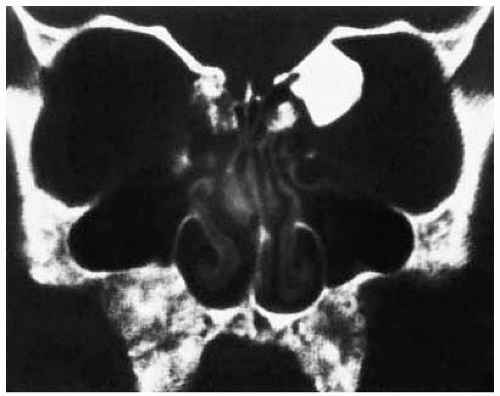 Figure 33.12. Coronal computed tomography of lesion shown in Figure 33.11. (Courtesy of James Orcutt, MD.) |
Orbital Osteosarcoma
General Considerations
Osteosarcoma (osteogenic sarcoma) is the most common primary malignant neoplasm of bone. It occurs twice as frequently as chondrosarcoma and three times more often than Ewing sarcoma (1). It is a neoplasm of children or young adults that usually originates in long bones and rarely from flat skull bones.
Osteosarcoma can affect the orbital bones as a primary lesion or as a secondary tumor after irradiation for familial retinoblastoma (1,2,3,4,5,6,7,8,9,10,11,12). It has an increased incidence in patients with Paget disease and fibrous dysplasia (4,5,6,7). There is a close genetic relationship between osteosarcoma and retinoblastoma, with both being linked to a deletion in the long arm of chromosome 13 (3). In the authors’ series of 1,264 orbital lesions, the 5 osteosarcomas accounted for 24% of osseous and fibro-osseous tumors and 1% of all orbital tumors (8). All 5 osteosarcomas in our series occurred in patients who had undergone ipsilateral orbital irradiation for hereditary retinoblastoma (11). We had no case of primary orbital osteosarcoma (8).
Clinical Features
Primary orbital osteosarcoma characteristically causes a rapid onset and progression of unilateral proptosis, pain, globe displacement, periorbital numbness, eyelid edema, and conjunctival chemosis (7). When the tumor arises from the ethmoid or frontal bones, there is downward or lateral displacement secondary to a firm, palpable, mass, whereas one arising from the sphenoid wing causes proptosis without a palpable mass.
Diagnostic Approaches
Orbital CT and magnetic resonance imaging (MRI) generally show an irregular, invasive, destructive bone mass with foci of calcification and invasion of adjacent soft tissue. If the osteoid content is low and the fibrovascular content high, then the lesion appears less dense than bone. In some cases, linear shadows radiate from the main mass because tumor cells grow in fingerlike projections from the main mass. CT shows the bony extent of the lesion; MRI can better delineate the soft tissue component.
Pathology and Pathogenesis
Orbital osteosarcoma is composed of malignant spindle cells with hyperchromatic nuclei and numerous mitotic figures. Osteoid and neoplastic bone formation are readily evident. If there are no bone elements, the lesion is more likely to be diagnosed as a fibrosarcoma (7). In many cases, the matrix of the tumor contains chondroid and fibromatoid elements and numerous blood vessels. Thin-walled sinusoidal spaces may contain neoplastic cells, perhaps accounting for the blood-borne metastasis.
Management
Osteosarcoma involving the orbital bones poses a difficult therapeutic challenge. Some authorities advocate preoperative chemotherapy, followed by wide surgical excision, and subsequent chemotherapy or irradiation depending on the clinical and histopathologic findings. The prognosis for patients with osteosarcoma of the orbital bones is generally poor and, historically, most patients have died despite treatment (7).
Selected References
1. Fu YS, Perzin KH. Non-epithelial tumors of the nasal cavity, paranasal sinuses, and nasopharynx: a clinicopathologic study. II. Osseous and fibro-osseous lesions, including osteoma, fibrous dysplasia, ossifying fibroma, osteoblastoma, giant cell tumor, and osteosarcoma. Cancer 1974;33: 1289-1305.
2. Mandel MR, Stewart WB. Periorbital osteosarcoma: an unusual case report and review of the clinical and histopathological features. Ophthal Plast Reconstr Surg 1985;1:129-136.
3. Benedict WF, Fung YK, Murphree AL. The gene responsible for the development of retinoblastoma and osteosarcoma. Cancer 1988;62:1691-1694.
4. Blodi FC. Pathology of orbital bones. The XXXII Edward Jackson Memorial Lecture. Am J Ophthalmol 1976;81:1-26.
5. Shields JA. Osseous, fibro-osseous, and cartilaginous tumors. In: Shields JA, ed. Diagnosis and Management of Orbital Tumors. Philadelphia: WB Saunders; 1989:205-211.
6. Epley KD, Lasky JB, Karesh JW. Osteosarcoma of the orbit associated with Paget disease. Ophthal Plast Reconstr Surg 1998;14:62-66.
7. Henderson JW. Tumors of orbital bone. In: Henderson JW, ed. Orbital Tumors. 3rd ed. New York: Raven; 1994:161-164.
8. Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: the 2002 Montgomery Lecture, part 1. Ophthalmology 2004;111:997-1008.
9. Goldberg S, Slamovits TL, Dorfman HD, et al. Sarcomatous transformation of the orbit in a patient with Paget’s disease. Ophthalmology 2000;107: 1464-1467.
10. Dhir SP, Munjal VP, Jain IS, et al. Osteosarcoma of the orbit. J Pediatr Ophthalmol Strabismus 1980;17:312-314.
11. Abramson DH, Ronner HJ, Ellsworth RM. Second tumors in irradiated bilateral retinoblastoma. Am J Ophthalmol 1979;87:624-628.
12. Parmar DN, Luthert PJ, Cree IA, et al. Two unusual osteogenic orbital tumors: presumed parosteal osteosarcomas of the orbit. Ophthalmology 2001;108:1452-1456.
Orbit Osteosarcoma
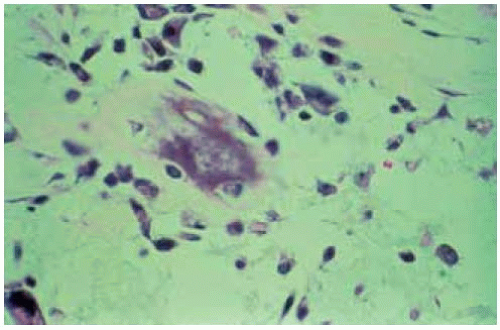 Figure 33.14. Histopathology of lesion shown in Figure 33.13 showing neoplastic cells in a myxom atousmatrix. (Hem atoxylin-eosin 200.) (Courtesy of Elise Torczynski, MD.) |
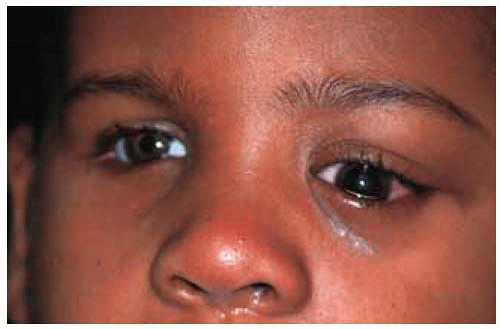 Figure 33.15. Facial appearance of a 5-year-old child who at age 1 year underwent enucleation of the right eye and irradiation of the left eye for retinoblastoma. |
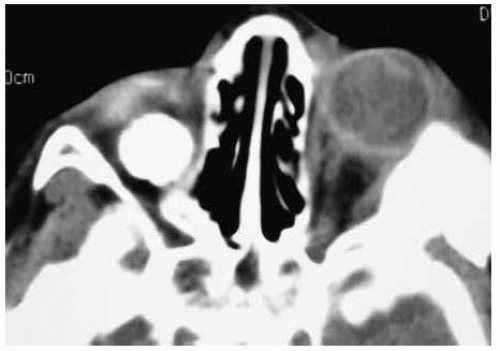 Figure 33.16. Axial computed tomography of child shown in Figure 33.15. Note the orbital implant in the right orbit and the extensive bony mass superotemporally in the left orbit. |
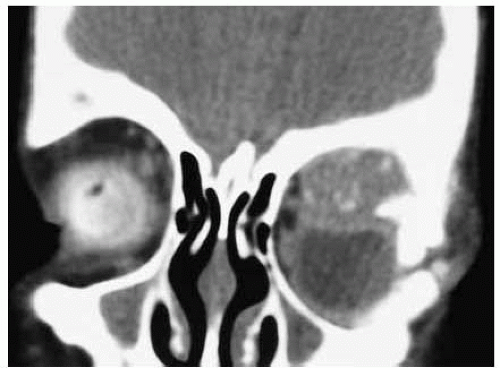 Figure 33.17. Coronal computed tomography of child shown in Figure 33.15. Note the soft tissue component in the superior portion of the left orbit. |
Orbital Fibrous Dysplasia
General Considerations
Several fibro-osseous lesions can occur in the orbital bones, including fibrous dysplasia, ossifying fibroma, aneurysmal bone cyst, giant cell tumor (osteoclastoma), giant cell reparative granuloma, and brown tumor of hyperparathyroidism. Most of these are discussed in more detail elsewhere (1,2,3,4) and are not covered in detail here.
Fibrous dysplasia, a fibro-osseous malformation that presumably results from an idiopathic arrest in the maturation of bone at the woven bone stage, can sometimes involve the orbital bones (1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22). It may be monostotic or polyostotic. The monostotic form accounts for 80% of cases, of which 20% affect the craniofacial bones. The frontal bone is most often involved, followed by the sphenoid and ethmoid bones. Orbital fibrous dysplasia is generally of the monostotic form, although it usually involves contiguous bones (3). The polyostotic form occasionally is found as a part of Albright syndrome, characterized by precocious puberty in girls and mottled skin pigmentation ipsilateral to the osseous involvement. Orbital cases are rarely associated with Albright syndrome (21,22).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree