8 Orbital Complications of Maxillary Sinusitis In this chapter, we will describe the relevant anatomy, physiology, and pathogenesis of orbital complications of maxillary sinusitis. The classification of orbital complications and the diagnostic and therapeutic strategies when dealing with these complications will also be discussed. Bacterial infection of the paranasal sinuses is one of the most common diseases affecting almost 32 million Americans every year.1 It almost always is a consequence of a preceding viral infection affecting the upper respiratory tract. The maxillary and ethmoid sinuses are the most common sinuses affected followed by the frontal and sphenoid sinuses. Sinusitis responds to medical treatment in the majority of cases, yet occasionally orbital complications may occur due to spread of infection. The infection may involve the eyelid and the surrounding skin or extend deeper into the orbit and its adnexa. Periorbital cellulitis (POC) refers to an infection involving the eyelid and the surrounding skin, whereas infection affecting the orbit and its contents is called orbital cellulitis (OC). Often POC, a commonly occurring infectious process, may be difficult to distinguish from OC, which is traditionally associated with a high morbidity and potential mortality. Sinusitis is a frequent cause of periorbital and orbital cellulitis accounting for up to 80% of cases. The ethmoid sinus is the most common source of orbital infection.2–4 Direct extension of infection from the maxillary sinus to the orbit, though rare, may occur in the presence of a preexisting defect in the orbital floor due to previous trauma or via the various venous channels connecting this structures.5,6 More commonly, orbital complications from maxillary sinusitis result when there is extension to or there is concomitant ethmoid involvement. Odontogenic infections are an infrequent but important cause of orbital infections.7–9 The apices of the maxillary molars and premolars that lie in close proximity to the floor of the maxillary sinus may be the source of ascending infection that progresses from the antrum into the ethmoid labyrinth, then through the lamina into the orbit. Infection from the maxillary sinus may also extend into the orbit through the inferior and the superior orbital fissure resulting in orbital abscesses that are laterally or posteriorly located. It must be appreciated the POC and OC are two distinct disorders with different etiologies. POC is a more common infectious process limited to the eyelids in the preseptal region. In contrast, OC represents a more severe, but less common, infection of the orbit posterior to the septum. If not diagnosed and treated promptly, OC can have devastating consequences. Permanent visual impairment has been reported resulting from orbital complications due to sinusitis.10–12 In a recent report of 218 cases of orbital infection, permanent orbital complications were reported in 19 patients including blindness (nine patients), strabismus (six patients), and ptosis (four patients).4 In another report describing 159 cases of orbital complications due to sinusitis, four patients suffered from permanent blindness.13 Increased intraorbital pressure due to infection in conjunction with the septic process might lead to blindness from thrombosis of the retinal artery, direct pressure effect on the optic nerve or vasculitis of its vasa vasorum. Visual loss may be gradual or sudden and may occur without any funduscopic abnormality. Life-threatening intracranial complications may arise from direct extension of the infection from the orbit via retrograde thrombophlebitis of the ophthalmic veins into the cavernous sinus.14 Infection may also extend intracranially through other anatomic routes, such as the optic foramen, superior orbital fissure, and ethmoid canals, where the periorbita continues as the dura. Although orbital complication may occur in both adults and children, the latter group is affected more frequently.4,10,15 Schramm and colleagues collected 303 cases of orbital cellulitis over a 10-year period.3 Age range was 2 weeks to 66 years. Another study by Shahin showed that 75% of the patients were below age 16 and 33% below 4 years.16 The severity of the disease may be lesser in children as compared with adults.17 Proptosis is a significant finding in orbital cellulitis. In general, the degree of proptosis correlates well with the severity of orbital cellulitis or abscess. The orbit may also be affected in chronic maxillary sinus disease. Chronic osteomyelitis may cause orbital cellulitis. Displacement of the globe and diplopia may also result from an expanding maxillary mucocele. Rarely, enophthalmos may be a sequel of chronic maxillary sinusitis causing its walls to collapse, a condition also described as silent sinus syndrome.18,19 The orbit is a quadrangular pyramidal cavity composed of seven separate bones. Sixty to 80% of the orbit has its contributions from the sinuses, i.e., the roof of the maxillary sinus, the lateral wall of the ethmoids, and the floor of the frontal sinus. The paranasal sinuses are in intimate contact with the orbit, which is separated only by a thin plate of bone from the frontal sinus superiorly, the ethmoid labyrinth medially, and the maxillary sinus inferiorly. The roof of the maxillary sinus forms the inferior orbital wall and is relatively thick. In contrast, the medial wall of the orbit, which is formed by the lateral wall of the ethmoid, is extremely thin, and therefore is called the lamina papyracea. The lamina papyracea may show bony dehiscence that offers little resistance to inflammation and displacing forces. The lamina papyracea also has preformed vascular channels communicating the ethmoid cavity with the orbit. Consequently, acute and chronic inflammatory disease within the sinuses has ready access to the orbit and its adnexa. The orbit is predominantly an osseous socket and any extension of inflammation or the compression of the orbital contents will lead to exophthalmos or proptosis. The surrounding paranasal sinuses are divided into two groups. The anterior group of paranasal sinuses, the maxillary sinus, the frontal sinus, and the anterior ethmoid cells, are a common source of orbital complications. Direct orbital spread of maxillary sinus disease is uncommon, and usually results when there is concomitant ethmoid involvement or there is extension of the inflammation to the ethmoid labyrinth. The posterior group of paranasal sinuses includes the posterior ethmoid cells and the sphenoid sinus. These are closely related to the orbital apex, optic nerve, and the cavernous sinus. Inflammatory disease in this region may cause serious complications including impairment of vision, blindness, cranial nerve palsies, and thrombophlebitis of the cavernous sinus. Venous drainage is the key to the spread of infection from the sinuses to the orbit. The venous drainage forms a vascular network that interconnects with the nasal cavity, orbit, and paranasal sinuses. These veins are valveless allowing retrograde extension of the infection. The superior and inferior ophthalmic veins course throughout the orbit, draining portions of the paranasal sinuses, and eventually empty into the cavernous sinus. The superior ophthalmic vein is continuous with the nasofrontal vein and the inferior ophthalmic vein receives tributaries from the eyelids, lacrimal sac, and orbital muscles. These interconnecting systems of veins permit ready access to the orbit and eyelids from infections in the nose and paranasal sinuses. The cavernous sinus contains several cranial nerves (CNs) including the oculomotor (CN III), trochlear (CN IV), first branch of the trigeminal, and the abducent (CN VI), as well as the internal carotid artery. The communication between the cavernous sinuses on either side, present a pathway for the spread of infection to the opposite side. Orbital extension of infection from the maxillary sinus may occur through a variety of avenues: • Direct invasion through compromised bony barriers: the most common spread of infection is by extension to the ethmoid labyrinth. Within the ethmoids, the lamina papyracea offers little resistance to infection. Often, the lamina papyracea may show various degrees of bone dehiscence that may be congenital or occur secondary to trauma or surgery. The lamina papyracea has two main natural openings along the fronto-ethmoid suture line through which the anterior and posterior ethmoid neurovascular bundles pass. Direct spread of infection can take place through dehiscent areas or through the vascular channels mentioned above. Infection from the maxillary sinus may also reach the orbit via the inferior orbital fissure. A rare route is via the pterygopalatine or the infratemporal fossa and the superior orbital fissure. • Retrograde septic thrombophlebitis: access to the orbit is gained by the ophthalmic vein via the pterygoid venous plexus. The pathogens can also reach the orbit via the facial vein and the angular vein. These veins communicate in the region of the medial canthus via its venous anastomosis with the supratrochlear veins and the supraorbital veins. A report of postmortem dissections have shown septic thrombi to occur in venous channels communicating the paranasal sinuses the orbit and cranial cavity.20 • Erosive osteomyelitis: osteomyelitic bone erosion of the maxillary sinus may extend to the orbit. Chandler’s classification, based on the anatomic location of inflammation, is the most widely accepted classification for orbital infections.21 According to the classification, orbital inflammation is divided into five groups (Fig. 8.1): Group I is preseptal cellulitis (PSC), Group II is orbital cellulitis (OC), Group III is subperiosteal abscess (SPA), Group IV is orbital abscess (OA), and Group V is cavernous sinus thrombosis (CST). The anatomic distinction among the various types of orbital infections is important as it significantly influences the selection of therapy and clinical outcome. In this group, the infection is limited to the skin and the subcutaneous tissue of the eyelid, which is anterior to the orbital septum (Fig. 8.2). The orbital septum is the reflection of the periorbita from the orbital margin to the globe and serves as an important barrier to the spread of infection. The orbital adnexa, including the muscles and optic nerve, lies behind the orbital septum and is unaffected by the infectious process. PSC accounts for ~70% of orbital infections.2,3 Reviewing 119 patients with inflammatory disease about the eye, Goodwin et al found that in 97 cases (81.5%), the infection was preseptal.22 Clinical findings in PSC include edema and erythema of the eyelid, with or without, conjunctival injection. As the infection is anterior to the orbital septum, there is no limitation of extraocular movement and no impairment of visual acuity. Often the segment of the eyelid involved may suggest the sinus of origin. Ethmoid sinusitis may cause edema of the eyelids medially early in the course of infection and later proceed to involve the entire eyelid. Maxillary sinusitis may produce swelling of the lower eyelid. Frontal or supraorbital ethmoid disease may involve only the upper eyelid. The inflammatory edema may totally close the eye and therefore it is extremely important to force the eyelids apart to evaluate the eye. A computed tomography (CT) scan obtained in this group will demonstrate edema of the eyelid anterior to the orbital septum. The characteristic finding is that the tissues posterior to the orbital septum are radiographically normal. PSC generally resolves with appropriate antibiotic therapy. Persistent swelling may represent the formation of an eyelid abscess, which will require independent drainage. Fig. 8.1 Drawings of the types of orbital infections as per Chandler.21 (A) Preseptal cellulitis (PSC). (B) Orbital cellulitis (OC). (C) Subperiosteal abscess(SPA). (D) Orbital abscess(OA). (E) Cavernous sinus thrombosis(CST). Subperiosteal abscess (SPA) is defined as a collection of pus between the bony orbital wall and the periorbita. The periorbita, which is loosely attached to the underlying bone, readily separates from it. The circumscribed swelling, resulting from the SPA tends to displace the globe and may cause impairment of ocular motility. SPA is commonly located in the superomedial or inferomedial aspect of the orbit (Fig. 8.3), but may occur in the superior, inferior, and even lateral aspects (Fig. 8.4).4 In the early stage, the patient presents with minimal conjunctival congestion and normal visual acuity. With progression of the disease, chemosis, proptosis, and limited mobility of extraocular muscles along with some visual loss develops. The abscess may remain localized or may penetrate the periorbita to produce an orbital cellulitis or abscess. On CT scan or magnetic resonance imaging (MRI), SPA is seen as a contrast-enhancing mass in the extraconal space with a ring-enhanced lesion or an air fluid level being pathognomic of an abscess. This is considered by most to be a surgical emergency requiring prompt drainage. Fig. 8.2 A patient with preseptal abscess (PSA). (A) Facial profile of the patient showing a fluctuant swelling of the upper eyelid. The patient’s vision was normal. Pus was aspirated confirming the abscess, which required surgical drainage. (B) Axial computed tomography scan of the patient showing the PSA. (C) The patient 5 weeks after the drainage of the PSA showing complete resolution. Fig. 8.3 A patient with inferior subperiosteal abscess resulting from maxillary sinusitis. This patient was referred by an ophthalmologist after the computed tomography scan showed a subperiosteal abscess secondary to maxillary sinusitis. Note the air bubble in the abscess and the concha bullosa. This patient had very minimal disease in the ethmoids. The abscess was drained endoscopically. Surgery involved trimming of the lateral lamella of the concha bullosa, uncinectomy, a wide middle meatal antrostomy, ethmoidectomy, exposure of the lamina papyracea, and removal on the lamina papyracea anteriorly to drain the abscess into the nasal cavity. Fig. 8.4 A 16-year-old boy with inferior and lateral abscess secondary to maxillary sinusitis. (A) Coronal computed tomography scan of the patient, who presented with proptosis and impairment of vision and eye movements. Note the inferior SPA and lateral extension of the abscess. (B) Open drainage of the abscess done by the ophthalmologist. Orbital cellulitis (OC) is postseptal cellulitis in which the infectious process spreads to the soft tissue posterior to the orbital septum and penetrates the orbital periosteum to involve the orbital contents (Fig. 8.5). There is diffuse edema of the orbital contents with infiltration of the adipose tissue with inflammatory cells and bacteria. In most cases, the patient presents clinically with severe eyelid edema, which may close the eyes. Proptosis and chemosis that result from obstruction of the ophthalmic veins may be so intense that prolapse of the bulbar conjunctiva develops. In most cases, there is impaired ocular mobility that may range from partial to total ophthalmoplegia. Continuous elevation of intraocular pressure leads to progressive visual loss and eventually permanent blindness. Ophthalmologic evaluation in orbital cellulitis might show a decrease in visual acuity and/or limitation of global movements, proptosis, significant chemosis, and eyelid edema. Constitutional symptoms may be prominent, with fever, malaise, and leukocytosis present. Treatment is with intravenous antibiotics and close monitoring of the patient for any progression of the disease. Absence of clinical improvement in the ocular findings, after adequate medical therapy, is an indication for surgical exploration or drainage. Fig. 8.5 A 52-year-old Chinese man with orbital cellulitis. (A) He presented with mild proptosis and gross chemosis of the left eye. The vision was slightly impaired and eye movements restricted. (B) Axial computed tomography scan of the patient. Note the inflammatory edema of the orbital fat in the affected eye emits different signals as compared with the normal eye. No obvious orbital abscess was noted. As his vision deteriorated despite antimicrobial therapy, an open surgical drainage was performed by the ophthalmologist. Minimal pus was drained, but the patient’s vision improved following the drainage. Fig. 8.6 (A) A 26-year-old man referred by the ophthalmologist with an orbital abscess documented on computed tomography scan. This patient presented with proptosis, ophthalmoplegia, restricted eye movements, and progressive deterioration of vision. (B) The patient underwent combined endoscopic and open surgical drainage of the orbital abscess. Following a complete ethmoidectomy and middle meatal antrostomy, the lamina papyracea was removed as far back as the orbital apex. Three incisions were made in the periorbita extending from posterior to anterior. The abscess was drained externally through an external ethmoidectomy incision. Orbital abscess (OA) is a collection of pus within the orbital tissues (Fig. 8.6A). This may arise from an acute sinus infection penetrating the periosteum or from an orbital cellulitis progressing to suppuration. Clinically, the patient presents with marked proptosis, chemosis, and ophthalmoplegia, and intense congestion of the eyelids and conjunctiva. Pus collection in close proximity to the optic nerve results in severe visual loss and even blindness due to compression. Septic or vascular visual loss may result from continued presence of pus within the orbit. Orbital abscess may sometimes be difficult to distinguish from orbital cellulitis. There is diffuse infiltration of the orbital fat with massive proptosis, extraocular enlargement, and occasionally gas formation seen within the orbital tissue on CT or MRI. If an obvious abscess is documented on the CT scan, emergent surgical drainage of the abscess is indicated (Fig. 8.6B). Cavernous sinus thrombosis (CST) may be caused by retrograde spread of infection through the superior and/or inferior ophthalmic veins into the cavernous sinus causing life-threatening septic thrombophlebitis (Fig. 8.7). Because the left and right cavernous sinuses are interconnected, the signs and symptoms of orbital infection may be bilateral in many cases. When the contralateral eye is beginning to be affected by orbital infection, it is most likely that the infection has extended to the cavernous sinus and should prompt the diagnosis of cavernous sinus thrombosis. Patients with CST are extremely ill on presentation, with signs of meningitis and multiple cranial nerve palsies bilaterally. Neglected or inadequately treated orbital infections may progress to cavernous sinus thrombosis. Occasionally, the disease may run a fulminant course, especially in the compromised host. This generally involves tissue invasion by opportunistic mycotic organisms. Fig. 8.7 A patient with cavernous sinus thrombosis. This immunocompromised diabetic 76-year-old man with fungal sinusitis presented with marked proptosis, chemosis, ophthalmoplegia, and complete visual loss. Despite aggressive medical therapy and surgical intervention, this patient died of the infection and cavernous sinus thrombosis. The organisms that cause these infections are similar to the bacteria that cause acute sinusitis, with the most common being Streptococcus pneumoniae, Haemophilus influenza, and Branhamella catarrhalis. In adults, Staphylococcus aureus and mixed cultures including anaerobic organisms such as Bacteroides species (sp) gram-negative anaerobic bacilli (Prevotella, Porphyromonas, and Fusobacterium), Peptostreptococcus and microaerophilic sp may be implicated.23,24 Anaerobes could be associated with cellulitis and orbital abscess that develops following chronic sinusitis or following sinusitis associated with odontogenic infection. The orbital infections associated with maxillary sinusitis of odontogenic origin is often polymicrobial and organisms most often isolated are anaerobic gram-negative bacilli, Peptostreptococcus sp, Fusobacterium sp, and Streptococcus sp.23,25 The organisms isolated in cavernous sinus thrombosis are S. aureus (50 to 70% instances), Streptococcus sp (20%), and gram-negative anaerobic bacilli. Similar organisms can be recovered from subperiosteal and orbital abscesses and their corresponding maxillary sinusitis. History and physical examination is the cornerstone of the diagnosis with emphasis on ophthalmologic examination to document any decrease in visual acuity, limitation of extraocular movement and cranial nerve deficits. A neurologic examination should also be performed to exclude concomitant intracranial complications. Elevated white blood count and CRP are nonspecific markers of inflammation and support the assumption of infectious process. Blood cultures have low yield yet can be taken when bacteremia is suspected due to chills and temperature elevation.10 Lumbar puncture is unreliable and should be used judiciously when central nervous system (CNS) involvement is suspected.24 Cultures from the nasal cavity and eye secretions have limited correlation to the sinus content and thus are not reliable. Plain radiographs are nonspecific yet can show the presence or absence of air fluid level, opacification or bony destruction of the sinuses. This imaging modality is seldom used today. CT is readily available and is the imaging modality of choice. It clearly demonstrates the orbital contents and the anatomy of the adjoining structures. For a more complete evaluation, CT scans are acquired in axial views; triplanar reconstruction permits evaluation in coronal, axial, and sagittal planes and provides detailed information of bone and soft tissue. Based on clinical symptoms, it is impossible to differentiate PSC or OC from an OA. CT scanning with contrast enhancement is capable of localizing an abscess and defining its walls. A CT scan may demonstrate SPA as either homogeneous or ring enhancement, with displacement of the rectus muscle and increased radiodensity of extraconal fat. Gas may be present within an abscess owing to gas-forming organisms or communication with an adjacent sinus. Bone window can outline bone defects that may predispose or result from the inflammatory process. Based on the CT scanning, Zimmerman and Bilaniuk have anatomically divided infections within the orbit proper into (1) intraconal—centrally within the muscle cone; (2) extraconal—peripherally between the periosteum and recti; and (3) subperiosteal—between the orbital wall and its periosteum.26 A CT scan has up to 90% accuracy in identifying SPA.27–29 Skedros et al found CT scans to be accurate predictors of SPA in 80% of their 20 cases, whereas Younis et al reported a diagnostic accuracy of 91% in a series of 43 patients with orbital complications.28,29 Though CT scans have a high degree of accuracy in identifying SPA, the importance of clinical examination and vigilance in periorbital involvement cannot be overemphasized.15,30 There have been reports where orbital abscess was not identified on the CT, but found on surgical exploration. Delay in surgery in such cases resulted in visual loss for some patients. Patt and Manning report of four patients, in their series of 159 patients, who developed permanent blindness.13 The presence of an orbital abscess, which was ultimately found at surgical exploration, was not diagnosed by CT in any of these four patients. MRI provides superior soft tissue resolution and tissue characterization when compared with CT and is indicated when orbital or intracranial extension of infection is suspected. OC is demonstrated as an increased signal signifying edema and inflammatory infiltrates in the orbital fat on T2-weighted images and with diffuse enhancement postcontrast (gadolinium) administration. On T1-weighted images, the signal of the fat is low due to the high water content within inflammatory process. Both SPA and OA are seen on T2 as ring enhancement with low signal intensity centrally and high signal, peripherally. An air fluid level within the collection is diagnostic of abscess. The role of MRI is useful for soft tissue details, delineating SPA, and early detection of intracranial involvement. Orbital ultrasound has been used in the diagnosis and in following the progression of intraorbital infection. This is an inexpensive study, does not expose the patient to ionizing radiation, and in most cases can be performed at the bedside if needed.31 Although its theoretical ability to differentiate severe tissue edema from abscess formation surpasses CT, the limitations of ultrasound are its inability to identify deep orbital as well as intracranial disease extent. Therefore, it is not recommended as a routine diagnostic test.15,22 Medical treatment should be aggressive from the early stages to prevent progression of the infection. In our institution, the majority of these patients present to the ophthalmologist and are referred to the Otolaryngology service. POC is best managed by a multidisciplinary team including an ophthalmologist, microbiologist, otolaryngologist, radiologist, and a pediatrician, as most patients are in the pediatric age group. The role of the otolaryngologist is extremely important as sinus disease accounts for more than 80% of POC. The management should be as an inpatient and is initiated with blood tests, cultures, and imaging studies of the sinus and orbit. Therapeutic measures should be instituted immediately. Evaluation of the patient should include a comprehensive clinical examination and imaging studies with an attempt to make a distinction between PSC and postseptal infection. Clinical examination should test for changes in visual acuity, papillary reactivity, and evaluation of extraocular mobility. Imaging studies such as the CT scans of the sinuses and orbit facilitate the diagnosis and aid in the distinction of PSC from a postseptal inflammation. Though CT scans are a fairly accurate predictor of SPA, these can sometimes be misleading and should not be the absolute criteria for surgical intervention.13,30 An MRI scan may be indicated in assessing complex presentations of POC or when intracranial complications are suspected. Patients with mild inflammatory eyelid edema and PSC can be treated with oral antibiotics such as amoxicillinclavulanate or a second-generation cephalosporin. Close monitoring of the patient is mandatory, however. Parenteral antimicrobial therapy should be initiated when postseptal involvement is suspected or develops. Drugs that have good blood–brain barrier are preferred. The parenteral agents include ceftriaxone or cefotaxime, and metronidazole or clindamycin should be added for anaerobe cover. Anaerobic bacteria should be suspected when orbital cellulitis is associated with odontogenic infection and chronic sinusitis. Vancomycin should be administered in cases where methicillin-resistant S. aureus is present or suspected. When CST is suspected, high doses of parenteral wide-spectrum antimicrobial agents should be used. The role of anticoagulants and corticosteroids is controversial. Medical therapy of orbital complications of sinusitis must also include supportive therapy with topical and systemic decongestants, humidification, analgesics, and hydration with intravenous fluids. The patient’s visual acuity and extraocular muscle mobility should be closely monitored. Sequential CT scans may be needed for follow-up. If there is no improvement with 24 to 36 hours of medical therapy, or there is progression of symptoms within 24 hours, surgical intervention is indicated. The majority of preseptal infections generally resolve with medical treatment except for an occasional case that forms an eyelid abscess and may require an incision and drainage. Intraorbital infections, however, are more serious and the majority of them require surgical drainage. A conservative approach for intraorbital abscesses such as SPA and OA is generally not recommended, though few reports in the literature support this.22,32,33 Goodwin and colleagues reported three patients of a series of 13 with orbital abscess who responded to antibiotic therapy alone.22 However, the selection criteria for conservative management should include normal visual acuity and some globe motion. Patients on conservative therapy must be vigilantly monitored and repeatedly reexamined during therapy and surgical intervention initiated if the vision is compromised. Souliere et al reported 5 of the 10 patients documented as SPA on CT scan were managed with intravenous antibiotics and nasal decongestion alone.32 All had complete clinical and radiographic resolution without complications. Handler et al caution that because it may not be possible to differentiate pus-containing abscesses from inflammatory masses seen on CT, a more conservative approach with aggressive medical therapy in such cases is justified.33 Others also warn of what appears as an orbital abscess on CT scan may not be confirmed at surgery. They advocate careful clinical evaluation and response to antibiotic therapy as important determinants in the decision for surgical intervention.34 Some authors have also reported a better outcome with conservative treatment in young children, particularly infants, as compared with adults who tend to have a worse prognosis.17 The general opinion, however, is that in view of the severe and potentially devastating complications, including visual loss, cavernous sinus thrombosis, and the potential for intracranial progression, surgical drainage should be performed sooner in the disease course. There have been several reports where CT scan had failed to detect intraorbital abscess. These reports express caution in interpreting the CT scan and advocate aggressive surgical therapy in appropriate clinical situations.13,30,35 Krohel et al report four cases with visual loss to less than 20/200, despite treatment with intravenous antibiotics and surgical drainage. A CT scan had failed to detect orbital abscess in two cases.35 It must be emphasized that inappropriate or inadequate treatment may result in significant morbidity. Furthermore, partially treated cases may not manifest the expected clinical findings of orbital infection and may present in an insidious fashion with symptoms evolving over weeks to months. In most cases, surgical intervention is indicated by the presence of an abscess on CT, deterioration of visual acuity, signs of deterioration and progression in the orbital involvement despite adequate medical therapy, relapse of symptoms, or their progression to the contralateral eye. Indicators for deterioration may be radiologic, clinical, or both. Proptosis may be used as an indicator for surgery. Surgery involves drainage of the abscess and the involved sinuses. Surgical management includes open external drainage, transnasal endoscopic drainage, or combined endoscopic and external drainage. In the past, open external drainage was the modality of choice for a majority of the patients.2 The diagnostic and treatment trends in orbital infections have changed since the rise in popularity of endoscopic sinus surgery in the mid-1980s.36 There have been several reports since early 1990 on the use of endoscopic sinus surgery for orbital infections.25,37–39 Medially located SPA are particularly suitable for endoscopic drainage.40,41 The main advantage of endoscopic surgery is the simultaneous treatment of causative sinus infection and orbital disease and the ability to explore the orbit with improved illumination and visualization using angled endoscopes when necessary. The added advantage is that of cosmesis given that it avoids the external scar of an open drainage. Though medial SPA is ideal for endoscopic treatment, there have been reports of draining superior and inferiorly located SPA using the endo-scopes.42 Drainage of orbital abscess, particularly intraconal abscess, is best achieved through a combined approach and should not be attempted without the active participation of ophthalmology colleagues. The surgery (see Video 8.1) is performed with the patient under general anesthesia and with orotracheal intubation. Nasal decongestion is achieved with neuropatties soaked in 4% cocaine if available, or oxymetazoline. With patient supine on the operating table, the head is elevated by ~20 degrees. During draping of the patient the eyes are left uncovered. The nasal mucosa is allowed to decongest for at least 10 to 15 minutes, after which the neuropatties are removed and the operating field is infiltrated with 1:80000 epinephrine. To avoid bleeding due to mucosal trauma, a 27-gauge needle is used and multiple sites for infiltration are avoided. The two main sites of infiltration are the uncinate process and the basal lamella. Often, the nasal mucosa is severely inflamed and may not respond to decongestion resulting in excessive bleeding during the surgery. Continuous suction provided by the microdebrider assists in clearing the bloody field and maintains optimal visualization intraoperatively. The majority of the surgery is performed using the zero-degree endoscope; and 30-, 45-, and 70-degree endoscopes are used as and when necessary particularly when working in the maxillary and the frontal sinus. The angled endoscopes are used to visualize laterally and around the corners into the orbit especially in the case of an intraorbital abscess. Maxillary sinusitis by itself is rarely the cause of OA, often it involves other paranasal sinuses. Most patients with orbital complication from maxillary sinusitis have involvement of the ethmoid labyrinth and require an anterior or complete ethmoidectomy with middle meatal antrostomy for drainage of the maxillary sinus. Manipulation of the frontal recess is usually not necessary, and is performed only when the epicenter of the infection is in the frontal recess. In most cases, a complete ethmoidectomy is performed by removing the uncinate process, the ethmoid bulla, only the middle part of the basal lamella to ensure the stability of the middle turbinate, and the posterior ethmoid cells. Depending upon the involvement, a sphenoidotomy is performed. A middle meatal antrostomy is performed to drain the pus within the maxillary sinus. The lamina papyracea is skeletonized from the orbital apex posteriorly to the nasolacrimal system anteriorly. The superior limit of exposure is the skull base and inferiorly is the roof of the maxillary sinus. The lamina papyracea is gently palpated with a Freer elevator and fractured at its thinnest location. A plane of dissection is established between the lamina papyracea and the periorbita, and the lamina papyracea is dissected off the periorbita using the Freer elevator. The extent of removal of the lamina papyracea and exposure of the periorbita depends on the extent and location of the abscess. In the situation when there is a circumscribed SPA, lamina papyracea overlying the SPA is removed to drain the abscess. Incision of the periorbita in draining a SPA may not be necessary. However, if there is an OA present, the periorbita is incised to drain the abscess. In case the orbital pressure is persistently elevated, it is prudent to decompress the entire medial orbital wall. This is done by one or several incisions of the periorbita. A sharp sickle knife or a #11 blade on a Bard Parker handle is used to make these incisions. The tip of the knife should remain superficial and the incision made from posterior to anterior. Most extraconal orbital abscesses can be drained by this maneuver. Drainage of an intraconal abscess, however, may require orbital exploration and must be done with an ophthalmologist. A combined approach is necessary in most cases. It is important to obtain pus for cultures. This should be done in the beginning of the procedure when purulent material is obtained from the middle meatus and the maxillary sinus. Subsequently, purulent material from the SPA or OA should also be obtained and sent for cultures. The patient’s general condition, vital signs, vision, and eye movements are monitored postoperatively. Postoperative care is performed as in routine sinus surgery. Patients are instructed to perform nasal irrigations twice a day. Endoscopic debridement is performed on a weekly basis until mucosal healing takes place. In pediatric patients, office debridement may not be tolerated by the patient and a second-look procedure may be necessary. This is individualized depending on the extent of surgery and the mucosal trauma during the operation. Systemic culture directed antimicrobial therapy is continued postoperatively. Once there is improvement and signs of infection have abated, the patient is sent home. Although infrequent, complications of sinusitis are clinical emergencies and can result in devastating permanent vision and neurologic deficits if not diagnosed and treated promptly. Orbital involvement in sinusitis occurs most commonly by spread of infection from the ethmoid sinuses; yet maxillary sinusitis can spread to the orbit directly through the superior wall of the maxilla or indirectly through extension to the ethmoids and then to the orbit. The main pathophysiologic mechanisms for infection spread to the orbit are direct extension through compromised bony barriers, septic thrombophlebitis, and erosive osteomyelitis. S. pneumoniae, H. influenza, and B. catarrhalis are the most common pathogens in acute sinusitis, yet S. aureus and anaerobes in a dental infection can also be the cause. Chandler et al have described five stages of orbital involvement: less severe infection might cause cellulitis of orbital tissue yet in more serious cases orbital abscess or cavernous sinus thrombosis might form, which carry a high incidence of permanent visual deficiency. When orbital complication of sinusitis is suspected, a CT scan is recommended to define the orbital involvement and detect abscess formation. In case of cellulitis without pus collection, broad-spectrum intravenous antibiotics can be started under close otolaryngologic and ophthalmologic follow-up. In contrast, abscess formation merits immediate surgical intervention and drainage of the involved sinuses as well as the intraorbital pus collection. In case of cavernous sinus thrombosis, anticoagulant therapy is added to surgical drainage and antibiotic therapy. A multidisciplinary team composed of an ophthalmologist, otolaryngologist, microbiologist, neurosurgeon, and a pediatrician, if the patient is a child, should manage patients together. Though open drainage of orbital abscess is widely practiced by ophthalmologists, endoscopic drainage of SPA and OA has been increasingly reported in the past 15 years. A combined endoscopic and open drainage may be necessary for some intraconal and/or laterally located OA. • Patients with periorbital cellulitis should be carefully evaluated and a distinction made between periorbital and orbital cellulitis. • A CT scan, generally the recommended imaging modality to differentiate between cellulitis and abscess formation, may not always be reliable. Clinical correlation is essential. • An MRI should be considered if intracranial complication is suspected. • Close ophthalmologic follow-up is essential to detect visual impairment, which dictates immediate surgical drainage. • Blood cultures and lumbar puncture have low yield and therefore are of limited value. • Dental infection is an important cause of sinusitis and if suspected, anaerobic coverage is recommended. • Open surgical drainage is widely practiced by the ophthalmologist when surgical drainage is indicated. • As the majority of orbital infections are caused by paranasal sinus infections, endoscopic surgical drainage of the sinuses should be performed. Endoscopic sinus surgery has the advantage of improved illumination and visualization. Angled endoscopes can be useful to look around the corners while draining the OA. • Depending upon the extent of the disease a middle meatal antrostomy and anterior ethmoidectomy is performed and if needed, posterior ethmoidectomy and sphenoidotomy can also be done. • In draining a medial SPA, the lamina papyracea is resected to drain the abscess. • Incision of the periorbita following removal of the lamina may be done if the abscess is extraconal or the intraorbital pressure is high. It may be combined with an open drainage. • Intraconal abscess is best drained by open drainage.
 Relevant Anatomy
Relevant Anatomy
 Pathophysiology of the Spread of Infection
Pathophysiology of the Spread of Infection
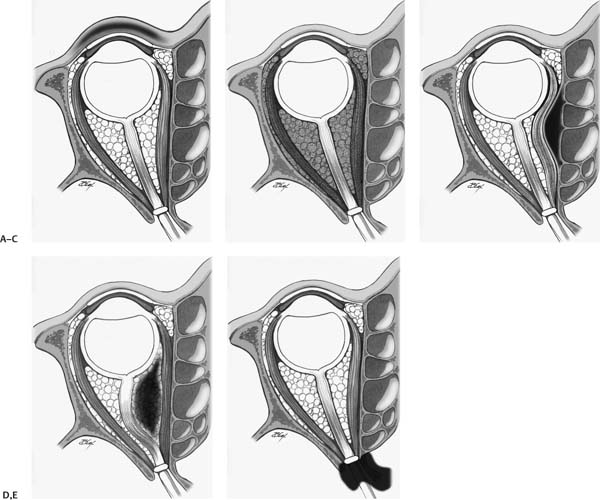
 Classification of Orbital Complications of Sinusitis
Classification of Orbital Complications of Sinusitis
Preseptal Cellulitis
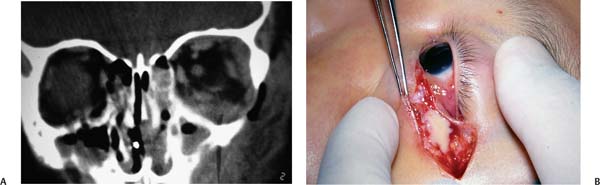
Subperiosteal Abscess
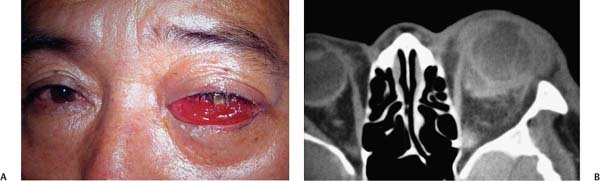
Orbital Cellulitis
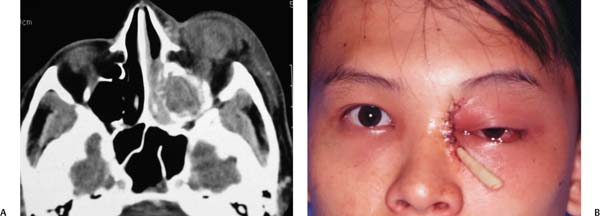
Orbital Abscess
Cavernous Sinus Thrombosis
 Microbiology
Microbiology
 Diagnosis
Diagnosis
Laboratory Tests
Imaging
 Management
Management
Medical Treatment
Surgical Management
Surgical Technique
Postoperative Care
 Conclusion
Conclusion
Orbital Complications of Maxillary Sinusitis
Pearls
< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree