Chapter 70 Ocular Histoplasmosis
Historical perspective
In 1942 Reid provided the first description of histoplasmosis-associated ophthalmic abnormalities from a patient with acute disseminated histoplasmosis.1 Following Reid’s description, additional reports surfaced of atrophic chorioretinal lesions associated with positive histoplasmin skin testing.2–4 In 1959 Woods and Wahlen4 published a series of 62 patients with granulomatous uveitis. Nineteen of these patients “showed a peculiar and consistent pattern of ocular lesions” that included both discrete atrophic, sparsely pigmented or unpigmented, peripheral lesions (frequently referred to as “histo spots”) and later cystic lesions in the macula. Skin testing for histoplasmin was positive in all of these 19 patients. Woods and Wahlen concluded that previous benign systemic histoplasmosis was responsible for the ocular findings in these 19 patients.4 A few years later Schlaegel and Kenney5 demonstrated that atrophic lesions around the optic nerve were also part of the clinical spectrum of ocular histoplasmosis syndrome (OHS), often called ocular histoplasmosis or presumed ocular histoplasmosis syndrome (POHS).
Clinical features of ocular histoplasmosis
A clinical diagnosis of ocular histoplasmosis is based on the presence of at least two of the following fundus lesions in one or both eyes in the absence of ocular inflammation:6,7
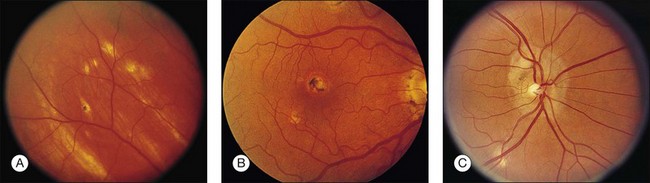
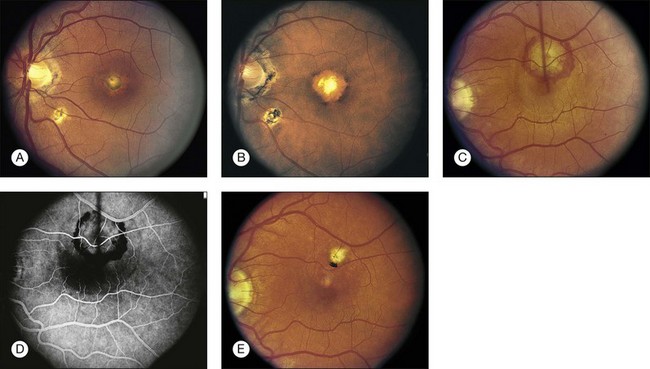
• Discrete, focal, atrophic (i.e., punched-out) choroidal scars in the macula or the periphery, smaller in size than the optic disc (histo spots) (Fig. 70.1).
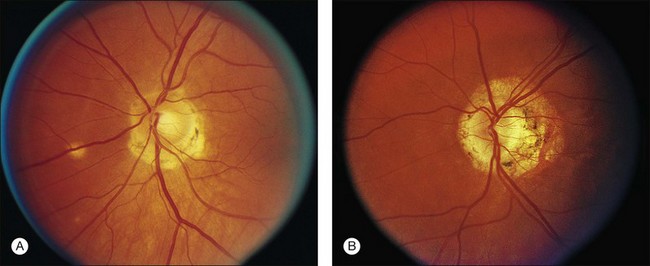
• Peripapillary chorioretinal scarring (i.e., peripapillary atrophy) (Fig. 70.2).
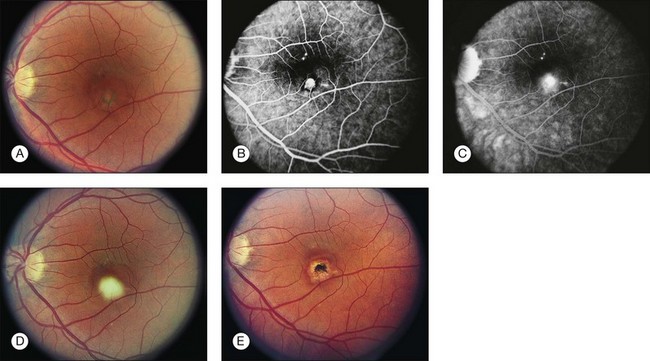
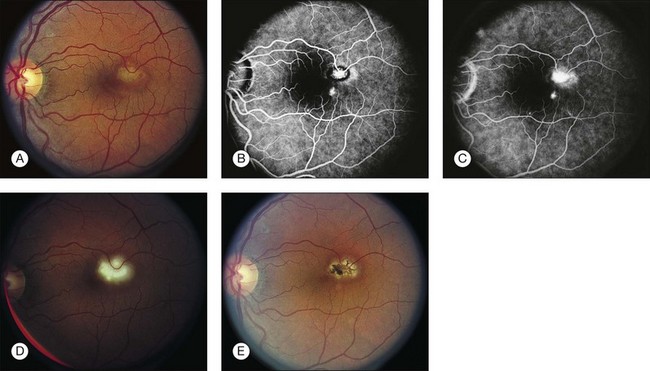
• CNV or associated sequelae (hemorrhagic retinal detachment, fibrovascular disciform scar) (Figs 70.3–70.5).
Most often both eyes have typical lesions, although the appearance may not be symmetric at initial presentation. The early granulomatous stage of ocular histoplasmosis, as described by Woods and Whalen, is rarely seen clinically.4,6 The initial focal scars are probably too small to be seen with the ophthalmoscope. Gass6 has postulated that lymphocytic infiltration of the surrounding tissue produces enlargement of the lesion over a period of years and thus allows it to become clinically detectable.
Differential diagnosis
The differential diagnosis of ocular histoplasmosis includes a wide spectrum of disorders:
• Multifocal choroiditis with panuveitis. Characterized by multiple chorioretinal scars with similar findings to ocular histoplasmosis. Significant anterior and/or posterior inflammation present in the active phase, and there may have associated CNV. One study examined distinguishing features of multifocal choroiditis compared to ocular histoplasmosis.8 Findings that were more characteristic of multifocal choroiditis included progressive growth of lesions, bridging scars, progressive proliferation of pigment, myopic disc changes, clustering of lesions (e.g., macula, equator), disc swelling, subretinal fibrosis, and narrowed/sheathed vessels.8 These features may be particularly important in distinguishing quiescent multifocal choroiditis from ocular histoplasmosis (see Chapter 76, White spot syndromes and related diseases).
• Myopic degeneration. Peripapillary atrophy and CNV may be seen in patients with myopic degeneration. Small white focal areas of chorioretinal atrophy along with linear atrophic areas (e.g., lacquer cracks) may also be present in the posterior pole (see Chapter 68, Myopic macular degeneration).
• Multiple evanescent white-dot syndrome (MEWDS). White lesions of the retinal pigment epithelium (RPE)/outer retina may be present with associated granularity of the fovea. Often the vision is transiently decreased with an associated enlarged blind spot. Mild inflammation may be present. Scarring and permanent chorioretinal lesions are not usually observed (see Chapter 76, White spot syndromes and related diseases).
• Idiopathic CNV. A diagnosis of exclusion. Particularly in younger individuals, idiopathic CNV is seen in the absence of other signs of ocular histoplasmosis, age-related macular degeneration (AMD), angioid streaks, and other CNV-related conditions.
• Choroidal rupture with CNV. A history of trauma is usually present. A partially circumferential concentric chorioretinal macular scar is typically present and is associated with the CNV. Peripapillary atrophy and associated peripheral chorioretinal atrophy is not present (see Chapter 91, Traumatic chorioretinopathies).
• Punctate inner choroidopathy. Minimal to mild inflammation may be present. Atrophic scars may be associated with CNV. Spots are usually smaller than those seen with ocular histoplasmosis. Predominantly seen in women. Peripapillary atrophy is usually not present. Acute symptoms (e.g., photopsias) are usually associated with the initial diagnosis of the white lesions and may correlate with location of lesions (see Chapter 76, White spot syndromes and related diseases).
• Neovascular AMD. Typically in older patients (i.e., >50 years). Drusen present. Areas of focal atrophy may be present in the macula but the atrophy is not usually seen in the periphery. Peripapillary atrophy is often not present (see Chapter 66, Neovascular (exudative or “wet”) age-related macular degeneration).
• Sarcoidosis. Scattered active inflammatory choroidal lesions may be present. Usually accompanied by anterior/posterior inflammation. CNV and peripapillary atrophy not typically present. Elevated angiotensin-converting enzyme may be seen. Often associated with hilar adenopathy on chest X-ray or CT scan of the chest (see Chapter 78, Sarcoidosis).
Relationship of ocular disease to systemic infection
Systemic infection with Histoplasma capsulatum via the respiratory tract is thought to be the initial event prior to the development of ocular histoplasmosis. Although a definitive causal relationship between H. capsulatum and the ocular disorder has not been demonstrated to satisfy Koch’s postulates completely,9,10 continuing experimental work with primates,11,12 may eventually satisfy this requirement.
• Almost all patients diagnosed as having ocular histoplasmosis in the USA have lived some or all of their lives in an endemic area.13,14
• Positive histoplasmin skin testing occurs more frequently in patients with ocular histoplasmosis compared with controls.14–16
• Activation of lesions of ocular histoplasmosis has been reported following histoplasmin skin testing.2–4,16–18
• DNA from H. capsulatum has been isolated from an enucleated eye previously diagnosed with ocular histoplasmosis.19
Other observations can be used to question the causal relationship between H. capsulatum and the ocular syndrome. In the UK and Europe, a clinical syndrome nearly identical to ocular histoplasmosis may occur.20–24 These patients have never lived in or visited an endemic area, however, and only a small proportion of Europeans are positive reactors to histoplasmin skin testing.20–25 Additionally, H. capsulatum has not been identified in the UK.25 Certainly, the possibility exists that an alternate organism may result in a similar ocular syndrome in these areas.22 Systemic antifungal treatment with amphotericin B has not been shown to be effective for the treatment of the ocular disorder.26.
Clinical features of systemic infection
Goodwin27 classified systemic infection based on the immune status of the host and exposure type. The usual histoplasmosis infection is a relatively mild illness with flu-like respiratory symptoms. Most patients do not seek medical care. Studies in Tennessee have demonstrated that almost 90% of children of 13 years of age had positive reactions to histoplasmin skin tests.28 A great deal of variation has been observed in the distribution of positive reactors by neighborhood of residence.29,30 Rarely, more severe, even fatal cases of disseminated infection may occur, but these are usually associated with immune system deficiencies, such as acquired immunodeficency syndrome (AIDS). Occasionally, epidemics of systemic disease outbreak may occur which are often associated with high levels of environmental exposure (e.g., excavations, construction projects in old buildings, work in chicken or other fowl habitats, or exposure in bat-inhabited caves).31–46
Epidemiology of ocular histoplasmosis
Geographic distribution of H. capsulatum in the USA
The Ohio and Mississippi river valleys make up the largest part of the “histo belt,” where 60% or more of lifelong residents have positive histoplasmin skin testing.47 Comstock described the major endemic histoplasmosis area as a triangle with its apices in Eastern Nebraska, Central Ohio, and Southwestern Mississippi.29
Prevalence and incidence
The prevalence of asymptomatic ocular histoplasmosis in endemic areas (e.g., Ohio, Maryland) within the USA ranges from 1.6 to 5.3%.14,15,48 The disciform lesion prevalence rates in the same areas were 0.0 to 0.1% of the endemic populations.14,15,48 In those eyes that had atrophic spots, the prevalence of disciform lesions was 4.5%.48
The incidence rate of neovascular disciform lesions and atrophic lesions is largely unknown. The development of initial neovascular disciform lesions has been reported at around 2 per 100 000 population per year.49 Studies examining the incidence rate of neovascular lesions in fellow eyes have shown a rate of 0.0 to 12% per year.50–54
Age
The median age of patients with vision-threatening disciform lesions has typically been reported to be in the fourth and fifth decade, with an age range of 10 to 81 years old.13,17,49,55–58 The median age of persons who have atrophic scars has been reported to be in the fourth, fifth, and sixth decades of life by various investigators.15,59 These reports are of the age at detection, however, and not necessarily the age of development of the atrophic lesion. It is likely that these lesions develop earlier in life and are only coincidentally discovered during ophthalmic examinations for causes of visual symptoms that may or may not be related to ocular histoplasmosis.
Gender and race
There is no gender predilection for ocular histoplasmosis. The vast majority of disciform lesions occur in Caucasians with only around a dozen cases reported among African Americans.60 Interestingly, histo spots and positive skin tests have been reported in some studies to have similar prevalence among Caucasians and African Americans.15,61 Other studies have found a much higher prevalence in Caucasians (i.e., nearly 100% of all cases) as compared to Hispanics or African Americans.14,16,48,55
Histocompatibility antigens and genetic predisposition
In disciform lesions, both human leukocyte antigen (HLA)-B7 and HLA-DRw2 have been reported to be two to four times more common among cases than controls.62–64 For histo spots, HLA-DRw2 was twice as common among cases as among controls, but less difference was seen between the groups in regards to HLA-B7.64,65 These findings suggest an underlying genetic susceptibility or predisposition for development of ocular histoplasmosis. It is unclear whether this genetic predisposition specifically reflects the susceptibility to ocular histoplasmosis or to infection by H. capsulatum. Although these associations exist, routine testing for HLA typing in connection with ocular histoplasmosis is not typically performed owing to the lack of significant positive and negative predictive values.
Pathogenesis
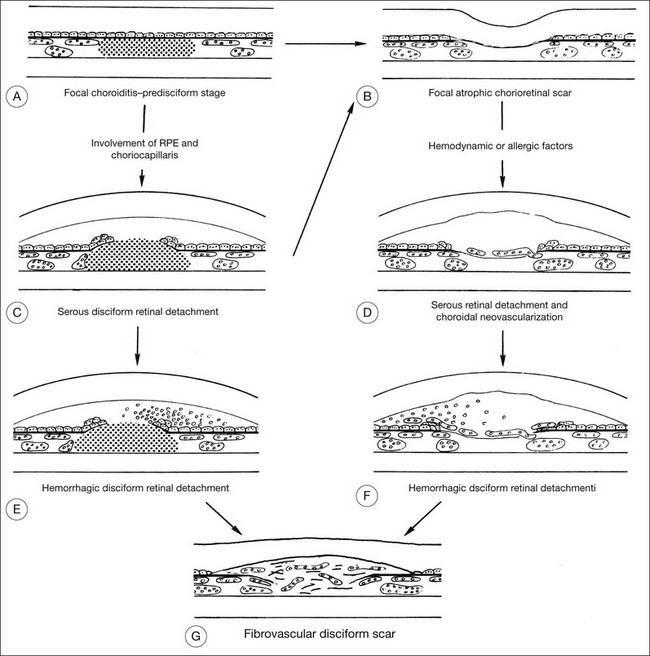
Numerous theories regarding the pathogenesis of ocular histoplasmosis have been proposed. The most widely accepted theory involves focal infection of the choroid at the time of systemic infection. The focal inflammatory/infectious process results in an atrophic scar that disrupts Bruch’s membrane. Alternatively, the infection may involve the retinal pigment epithelium and choriocapillaris and may progress rapidly to subretinal hemorrhage, exudation, and a fibrovascular disciform scar (Fig. 70.6).
CNV formation may be promoted by multiple factors at the site of the atrophic scar. Disruption of Bruch’s membrane provides access to the subretinal space for neovascularization.66 The fragile vessels are prone to hemorrhage and exudation, often ultimately resulting in disorganization of the RPE and neurosensory retina and, ultimately, a fibrovascular scar.
The initiator for CNV development is unknown. The results from HLA typing suggest a possible genetic predisposition for progression from atrophic scars to disciform lesions in ocular histoplasmosis.62–65 Other hypotheses have attributed these phenomena to a larger initial inoculum of the fungus,11,67 reinfection,4,68 hypersensitivity,4,14 and the presence of other factors that compromise the vascular system14,69,70 or the immune system.71 CNV development has also been associated with proangiogenic factors such as vascular endothelial growth factor.72
Studying ocular histoplasmosis with animal models has been difficult. Histoplasmosis is known to occur in many species of animals.73–77 However, efforts to develop an animal model for ocular histoplasmosis have been hampered by two major factors: (1) nonprimates do not have a macula with its special anatomic, physiologic, and neurologic characteristics; and (2) decades are believed to elapse between initial infection with H. capsulatum and the development of characteristic macular lesions. The most promising animal models are primates, in which systemic infection and ocular lesions have been produced.11,12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree