, Natalia D. Gladkova2, Valentin M. Gelikonov3, Jerome L. Belinson4, Natalia M. Shakhova3 and Felix I. Feldchtein5, 3
(1)
Nizhny Novgorod Regional Hospital, Radionovast., 190, Nizhny Novgorod, Russia
(2)
Medical Academy, Nizhny Novgorod, Russia
(3)
Institute of Applied Physics Russian Academy of Sciences, Nizhny Novgorod, Russia
(4)
Cleveland Clinic Foundation, Cleveland, OH, USA
(5)
Imalux Corporation, Cleveland, OH, USA
Keywords
Gynecologic OCTOCT colposcopyendometrial OCT imagingCervical leukoplakiaCervical metaplasiaOCT laparoscopy77.1 Introduction: Motivation for OCT Application in Gynecology
Timely and efficient diagnosis of diseases of the female reproductive system is very important from the social viewpoint [1, 2]. Diagnostic efficacy of the existing techniques still needs improvement since malignant neoplasms of the female reproductive system organs are stable leaders among causes of death (over 35.9 %) [3]. Each year, 851.9 thousand genital cancer cases are recorded worldwide [1, 2].
Cervical cancer is among the most common malignant neoplasm in women and the most common cause of death from cancer in young women worldwide. It commonly occurs at the height of women’s productive lives often when they still have young children at home. Yearly, 510,000 new cervical cancer cases are registered worldwide, and of these cases, 288,000 women die, and over 5–6 billion dollars is spent on patient treatment [2].
A decrease in the cervical cancer incidence has occurred in the senior age group, while a significant increase is observed for women in the early reproductive age group (by 2 % yearly, on the average) [4–6]. In the USA, according to the data of the American Oncological Society as of 2002, 47 % of the cervical cancer patients are women up to 35 years old [7]. Cervical cancer in young women has a less favorable prognosis, because it progresses faster, late stage is observed more frequently than in the senior age group, and consequently 5-year survival is lower [7].
Initial risk stratification for cervical neoplasia is performed using screening techniques including Pap smear and HPV (human papilloma virus) testing. The next step for diagnosis is a visual examination of the cervix. The potentially neoplastic lesions can be better visualized using application of acetic acid. The unmagnified examination of the cervix is known as VIA (visual examination with acetic acid), and the magnified examination using low-magnification, long working distance microscope, is known as colposcopy. Both VIA and colposcopy are frequently combined with biopsies. Histopathology evaluation of the biopsies serves as a “gold standard” for diagnosis.
However, the diagnostic efficacy of the visual examination with biopsy is limited. Similar visual abnormalities can be observed for a variety of cervical conditions, benign and malignant, which reduces specificity and positive predictive value. Correct interpretation of colposcopic features requires high skills and long-term clinical experience, which makes colposcopy very subjective and limits interobserver agreement [8–10].
In addition, histological processing of biopsy requires several days or even weeks, which creates several problems. In most cases, treatment decisions cannot be made until histology results are received and reviewed, which requires more visits and increases healthcare cost and patient anxiety. In underdeveloped countries (which account for 80 % of the world’s cervical cancer cases), additional visits can be difficult or impractical. Therefore, in many cases a real-time decision should be made without biopsy results, representing a difficult tradeoff between potentially unnecessary treatment because of oversensitive but not specific diagnostics and, alternatively, potentially leaving early and curable cervical cancer untreated which could then grow into a life-threatening condition.
OCT is known to visualize in vivo and noninvasively tissue microstructure with spatial resolution approaching the histologic level and therefore can be expected to guide biopsies and to provide real-time tissue structure information when biopsies are contraindicated or impractical. Although thorough clinical studies are required to determine if OCT can be suitable for this purpose in gynecology in general and for cervical cancer in particular, the early results look encouraging.
The first in vivo OCT images of the uterine cervix were obtained by a Nizhny Novgorod team in 1997 [11]. Later, the clinical feasibility of OCT in gynecology was discussed in a number of papers [12–22]. The papers published by the MIT group in 1999 [23, 24] described the OCT features typical for a normal exocervix (a sharp, high-contrast interface between stratified squamous epithelium and connective tissue stroma), endocervix (visualization of cervical glands), and endometrium (contrast of glands). It was shown that the possibility to detect neoplastic changes in stratified squamous epithelium by the OCT is associated with the disappearance of the interface between the epithelium and connective tissue. These findings were later confirmed in the studies performed by the ССF group [25, 26] and the University of Texas at Austin [27].
The OCT potential for pelvic organ visualization during laparoscopy was explored in several papers [12, 15, 23, 28, 29]. The Nizhny Novgorod group [15] and the MIT group [29] explored the use of OCT to assess the functional condition of the fallopian tubes in reproductive gynecology. A University of Arizona group, considering four categories of the ovarian conditions (norm, endometriosis, high neoplasia risk, and neoplasia), formulates the OCT features to differentiate between benign and malignant processes [28].
In this chapter, we present a wide spectrum of the OCT studies of different parts of the female reproductive system and demonstrate the potential of the clinical use of a new visualization method in gynecological practice.
77.2 OCT-Colposcopy
77.2.1 Methodology and Patient Selection
During the OCT study of the female reproductive system, 235 patients were enrolled at the Nizhny Novgorod Regional Hospital and Regional Oncology Clinic.
All patients signed the voluntary informed consent. The study was approved by the Ethical Committee for scientific studies with human subjects.
The majority of work was performed on the uterine cervix. Two hundred five patients were enrolled in the cervical OCT study, average age 36.5 years.
The cervical OCT was performed for the patients with:
(i)
History of abnormal colposcopic findings
(ii)
Abnormal results of Pap smear (ASCUS, LSIL, HSIL)
(iii)
Positive HPV test for oncogenic viral type
Exclusion criterion was age under 18.
The breakdown of exocervical conditions is shown in Table 77.1 for the studied group of patients.
Table 77.1
In vivo OCT study of the female reproductive system
Total studied, n = 205 | ||||
|---|---|---|---|---|
Normal, n = 30 (14.6 %) | Benign pathological conditions, n = 113 (55.1 %) | Malignant pathological conditions, n = 52 (25.4 %) | Pregnant n = 10 (4.9 %) | |
Ectopy, n = 47 | CIN III, n = 28 | Uterine cervix cancer, n = 24 | ||
Exocervicitis, n = 28 | ||||
Endometriosis, n = 7 | ||||
Cervical erosion, n = 10 | ||||
Leukoplakia, n = 12 | ||||
CIN I–II, n = 19 | ||||
77.2.1.1 Uterine Cervix OCT Protocol
The cervical study OCT involved several stages:
Review of patient history including cytology results
Visual examination/colposcopy and identification of regions of interest (ROI)
OCT of identified ROI
Biopsy of ROI, when clinically appropriate
Histopathology evaluation of biopsy and comparison with OCT and colposcopic findings
OCT does not require additional preparation of the patient and anesthesia.
During the OCT studies, we used a compact portable OCT system developed and constructed at the Institute of Applied Physics of the Russian Academy of Sciences (Nizhniy Novgorod, Russia). The device received Russian regulatory authority certification for clinical use in August 2005.
The unit has the following technical characteristics:
Central wavelength 1,300 nm
Radiation power: not exceeding 6.0 mW
Spatial resolution: 10–20 μm
In-depth scanning range – up to 2 mm
Lateral scanning range 1–2 mm
Acquisition time for two-dimensional 200 × 200 pixel image: 1.5–2 s
The device is compact and has the following dimensions: 250 × 400 × 450 mm. The weight is 10 kg. All optical and electronic parts of the OCT unit are located inside a console.
The cervical OCT was performed using a detachable, reusable forward-looking OCT probe with an outer diameter 2.7 mm (Fig. 77.1a, b). The probe can be cold disinfected or sterilized. Alternatively, a disposable sterile sheath with an optically transparent membrane (Fig. 77.1b) was used to hold the probe and prevent contamination; in this case the probe was not in direct contact with the patient tissues.


Fig. 77.1
OCT probe distal tip (a) and a disposable sheath (Imalux Corporation) (b)
To perform OCT, the probe was applied to the cervical area of interest under the colposcope control. To reduce artifacts related to unintentional movements of the probe and the study object, the distal end of the probe or the sheath membrane was in contact with the tissue.
The obtained images were interpreted directly at the time of the patient examination.
Later, we conducted a comparative analysis of the OCT and histological data. The material obtained by the biopsy, loop electro excision procedure (LEEP), and hysterectomy was subject to histological assessment. The guided biopsy was performed under the colposcopic control immediately after the OCT imaging only when clinically indicated. Cervical histopathology was obtained for 138 out of 205 (67.3 %) patients. The specimen volume and depth were sufficient for identifying the structures in the OCT image with size usually equal to 1.7 × 1.5 mm.
77.2.2 OCT Images of Normal Cervix: Impact of Age and Hormonal Status on the OCT Image
Thirty patients with an unchanged uterine cervix were enrolled in the study. Some of these patients had colposcopy as a stage of preparation for radical hysterectomy. The cervical OCT was performed in vivo during colposcopy 1 day before the surgery. The cervical area to image was chosen at 12 o’clock of a conventional dial, 1 cm from the cervical channel, and the ex vivo imaging was performed of the same area of the fresh surgical specimen, followed by histopathological evaluation.
Figure 77.2 shows typical OCT image (а) and the parallel histology (b) of the unchanged normal cervix. The upper homogeneous layer with moderate signal level corresponds to a stratified squamous epithelium in the histological specimen. The lower, brighter layer in the OCT images corresponds to the connective tissue stroma of the cervical mucosa.
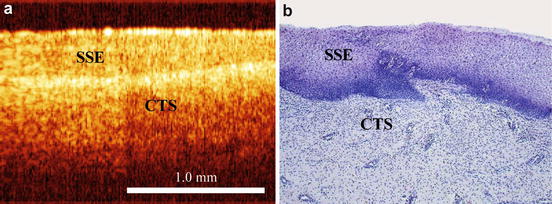
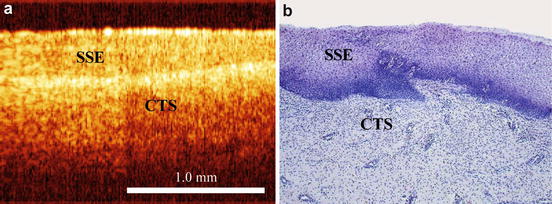
Fig. 77.2
OCT image (a) and parallel histology (b) of the cervical mucosa. SSE is the stratified squamous epithelium and CTS is the connective tissue stroma. OCT vertical scale is normalized to 1.4 refraction index
The interlayer interface corresponds to the basal membrane location; however, the basal membrane itself is extremely thin (several nanometers) and cannot be directly visualized using light.
After the application of 5 % acetic acid, optical backscattering increases, which is consistent with visual appearance (especially for the acetowhite epithelium) (Fig. 77.3).
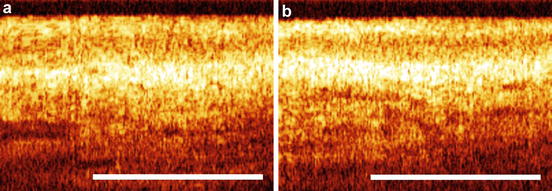
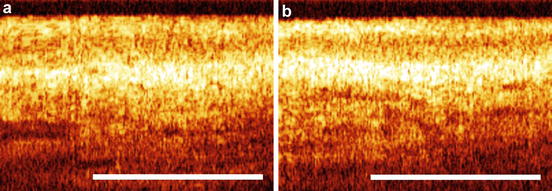
Fig. 77.3
ОCТ images of the normal cervical mucosa. (a) Before application of 5 % acetic acid, (b) after application of 5 % acetic acid
We consistently observed a two-layered image with an even, sharp, and continuous interface between the layers as the main sign of the normal exocervical OCT appearance for any age group.
77.2.2.1 OCT Study of the Epithelial Thickness of the Cervical Mucosa
Since the stratified squamous epithelium is well delineated in the normal cervical OCT images, the thickness can be easily measured. This thickness changes significantly depending on the menstrual cycle phase since it is known to be hormonal status dependent. The colpocytological study was performed for ten patients in the group with normal uterine cervix. We used karyopyknotic index (KI) and maturation index (MI) as commonly accepted means to assess hormonal status [30]. Figure 77.4 shows OCT cervical images for two patients in the same age group but with different estrogenic saturation level. For the first patient, 24 years old, the KI on the 24th day of the menstrual cycle was 28 and the MI was 0/44/56, the epithelial thickness was measured 250 μm (Fig. 77.4a) in the OCT image. The second patient, 30 years old, on the 17th day of the menstrual cycle, had KI equal to 0 and MI 0/89/11. Accordingly, the epithelial thickness was 160 μm.
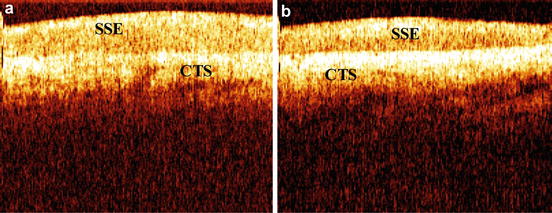
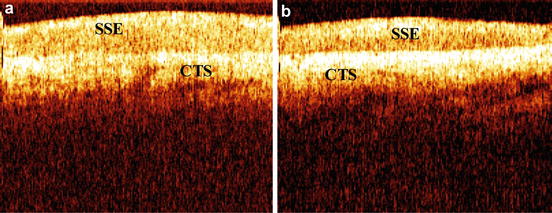
Fig. 77.4
ОCТ images of the cervical mucosa for two patients in the same age group: (a) a 24-year-old patient on the 24th day of the menstrual cycle, KI is 28, MI is 0/44/56, the SSE thickness is 250 μm; (b) a 30-year-old patient on the 17th day of the menstrual cycle, KI is 0, MI is 0/89/11, the SSE thickness is 160 μm. SSE is a stratified squamous epithelium and CTS is the connective tissue stroma
More pronounced differences can be observed between different age groups (Fig. 77.5). Pronounced proliferation with KI = 32 and MI = 0/26/51 was detected for a 29-year-old patient on the 12th day of the menstrual cycle. In the OCT image (Fig. 77.5a), the epithelial thickness was 275 μm. Epithelial atrophy with KI = 0 and MI = 12/88/0 was visualized for a 65-year-old patient (Fig. 77.5b) with the epithelial thickness reduced to 100 μm.
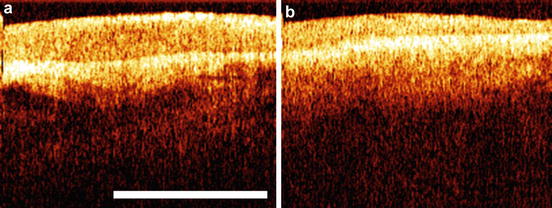
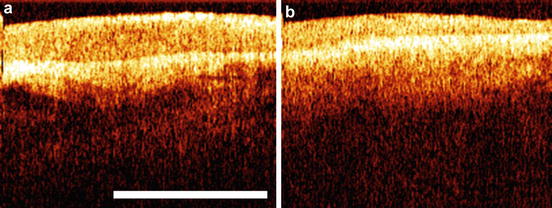
Fig. 77.5
ОCТ images of the cervical mucosa for two patients in different age groups: (a) 29-year-old patient on the 12th day of the menstrual cycle with KI = 32 and MI = 0/26/51, the SSE thickness is 275 μm, (b) 65-year-old, 20 years postmenopausal, KI = 0 and MI = 12/88/0, the SSE thickness is 100 μm
Therefore, OCT visualizes and allows objective in vivo measurement of the epithelial thickness variation in the cervical mucosa, including changes related to the hormonal status.
77.2.3 OCT Images of Benign Processes
77.2.3.1 Ectopy and Metaplasia
The normal cervical OCT appearance serves as a good baseline, and changes of this pattern can be associated with different benign and malignant pathological conditions.
Cervical ectopy (or ectropion) is a very common benign cervical condition. According to the histological data, the stromal base of ectopy is loose, infiltrated by inflammatory cells, and has a papillary shape with formation of crypts. The stromal papillae are covered by a single-row cuboidal epithelium. In the majority of cases, ectropion is visualized in the form of a non-layered structural image (Fig. 77.6a) in which chaotically located various shaped and brightness regions are observed. Comparing OCT images and histology slides, we found that bright (strongly scattering) parts correspond to the CTS, while dark (weakly scattering) parts correspond to the mucus-filled space between the stromal papillas.
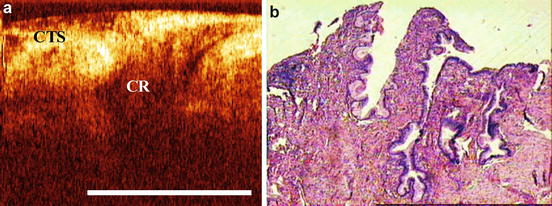
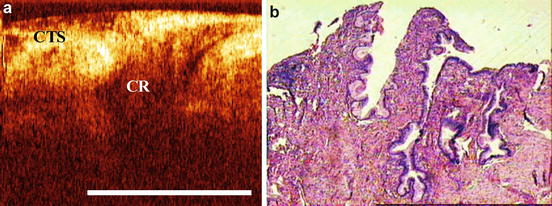
Fig. 77.6
OCT images (a) and parallel histology (b) of the cervical ectropion. CTS is the connective tissue stroma and CR is the mucus-filled crypts
The squamous regeneration process is accompanied by formation of structural elements (open ducts and cervical glands). The OCT is capable of visualizing these structures in vivo (Fig. 77.7).
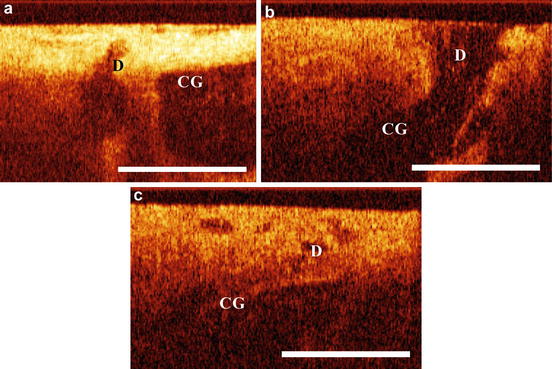
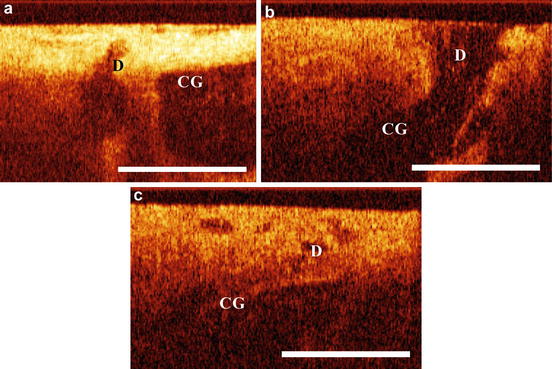
Fig. 77.7
(a–c) OCT images of structural regeneration elements. CG are cervical glands and D are the ducts of the cervical glands
Once the formation of a mature metaplastic epithelium is completed, the cervical mucosa is visualized as a sharp double-layered image with an even interlayer interface, resembling original squamous epithelium. However, closed cervical glands are seen under that new squamous epithelium (Fig. 77.8), which makes it different from the normal (original) squamous cervical mucosa.
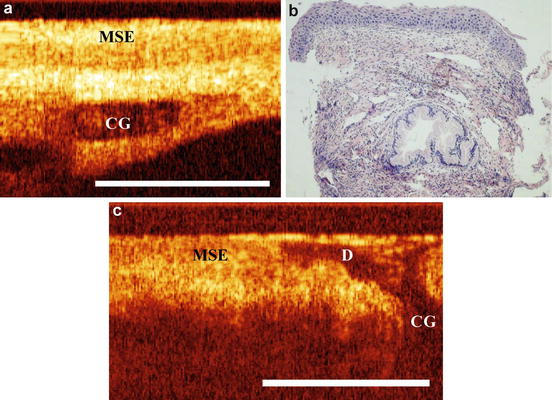
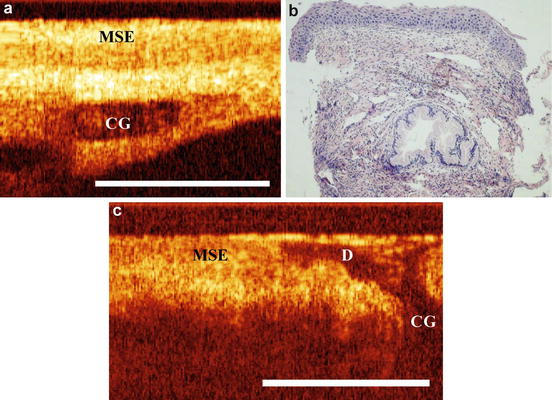
Fig. 77.8
OCT image of mature metaplastic epithelium (a, c) and parallel histology (b). CG are the closed cervical glands. MSE is the mature squamous epithelium. (c) D are the ducts of the cervical glands
77.2.3.2 Cervicitis
OCT images of inflammatory cervical changes may look different. OCT images still may have a sharp double-layered appearance. However, the contrast between SSE and stroma can be substantially reduced or completely lost. We associate it with the cellular infiltration changing stromal optical properties. In some OCT images, multiple sharp round and/or linear cavities with a low signal level (Fig. 77.9) can be observed. These cavities can be associated with edema and/or cervical glands.
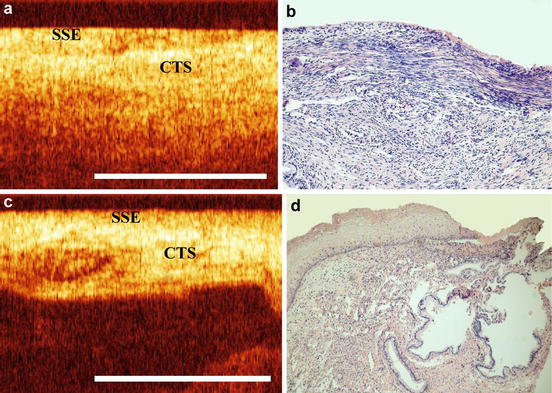
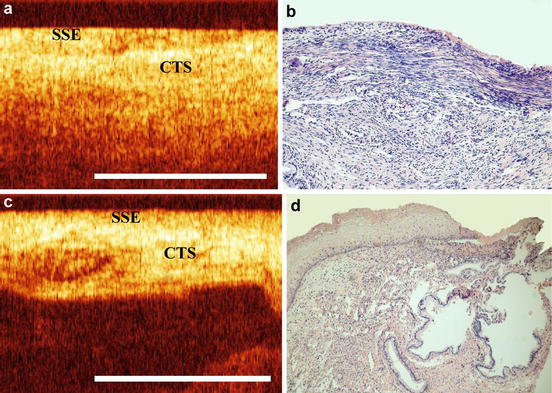
Fig. 77.9
OCT images (a, c) and histology (b, d) of the cervical mucosa with cervicitis. SSE is the thinned stratified squamous epithelium. CTS is the connective tissue stroma
As in normal cervical mucosa, application of acetic acid reduces the stratification contrast and increase brightness of the upper layer (Fig. 77.10).
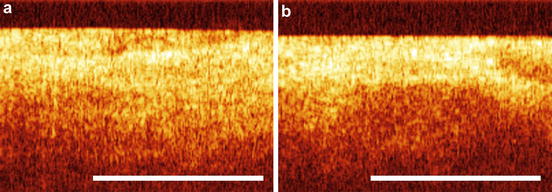
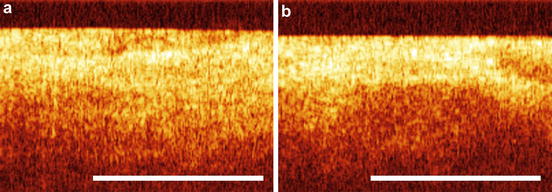
Fig. 77.10
OCT images of the cervicitis. (a) Before acetic acid application; (b) after the acetic acid application
In some cases, severe inflammation can completely erase the contrast of the epithelium-stromal interface, creating structureless OCT images (Fig. 77.11).
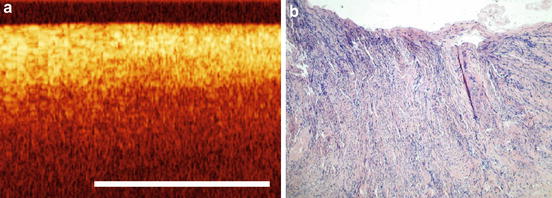
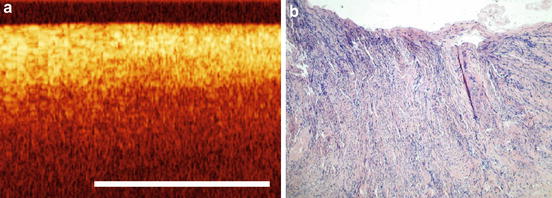
Fig. 77.11
ОCТ image (a) and histology (b) of the inflamed cervical mucosa
The inflammatory process can be accompanied by epithelial hyperplasia, acanthosis, and papillomatosis, which are visualized as an increase in the upper moderately scattering layer thickness and discontinuous nature of the interlayer interface (Fig. 77.12).
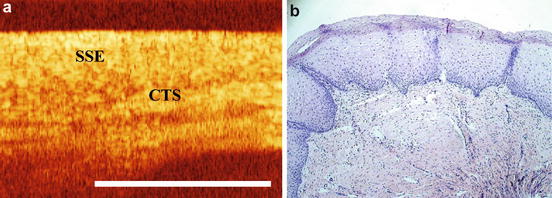
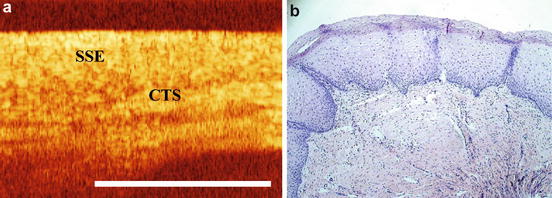
Fig. 77.12
ОCТ image (a) and histology (b) of cervical mucosa with inflammatory process of the viral etiology (HPV). SSE is the hyperplastic stratified squamous epithelium, CTS is the connective tissue stroma
77.2.3.3 Cervical Leukoplakia
Hyperkeratosis
In the presence of mild hyperkeratosis, the cervical mucosa is still visualized in OCT as a structural layered image (Fig. 77.13). The keratinization is responsible for an increase in the superficial brightness of the image. The interface between the layers could be discontinuous with reduced contrast, because of papillomatosis, which frequently accompanies hyperkeratosis.
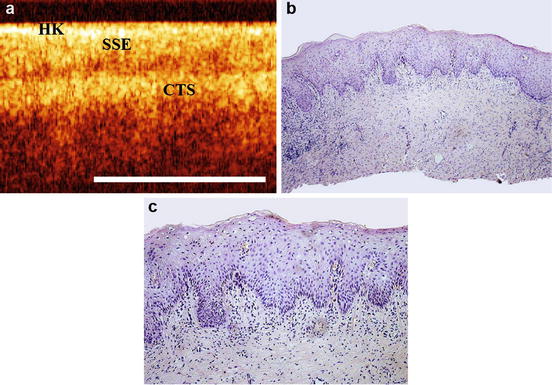
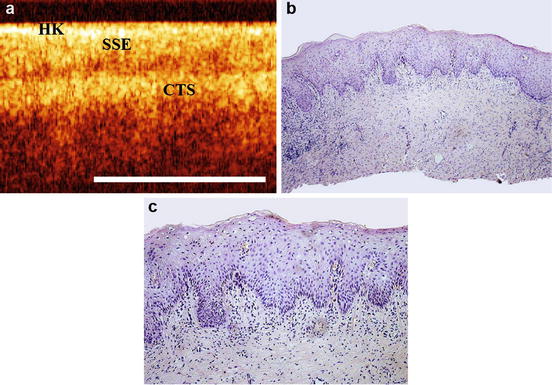
Fig. 77.13




ОCТ image (a) and histology (b, c) of the cervical mucosa with the mild hyperkeratosis. HK is the hyperkeratosis, SSE is the stratified squamous epithelium, and CTS is the connective tissue stroma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


