Chapter 89 Nystagmus in childhood
Introduction
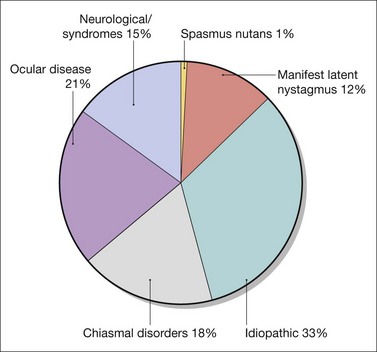
Nystagmus in childhood can be idiopathic or associated with retinal diseases, low vision in infancy, and a variety of syndromes and neurologic diseases. Nystagmus associated with neurologic disorders may be similar in appearance and pathophysiology to acquired nystagmus. Onset may also be after 6 months of age. The estimated prevalence of nystagmus (including both infantile and acquired nystagmus) is 24 in 10 000. The prevalence of infantile nystagmus is 14 per 10 000.1 Among the infantile forms of nystagmus, idiopathic nystagmus is the most common, followed by nystagmus associated with ocular disease. The diagnoses associated with infantile nystagmus are shown in Figure 89.1.
Causes of infantile nystagmus
The causes of most forms of infantile nystagmus are unknown. Infantile nystagmus is considered to be a disorder of gaze-holding and slow eye movement systems,2 leading to sinusoidal oscillations and/or drifts of the eye away from fixation. These involuntary slow eye movements constitute nystagmus slow phases. The slow phases are interrupted and shaped by the interposition of nystagmus quick phases which serve to realign the eyes.
Many types of infantile nystagmus are associated with sensory abnormalities during early visual development.3 With “afferent” diseases such as achromatopsia and congenital cataract, the nystagmus is the result of changes in the otherwise healthy ocular motor systems in response to afferent deficits present during visual development. For other conditions, such as albinism and various syndromes, it is uncertain whether the nystagmus is also due to afferent deficits or abnormalities in ocular motor neural circuitry.
Quality of life and infantile nystagmus
Quality of life studies of adults and children with infantile nystagmus show that the effects on visual function are considerable and are comparable to diseases such as age-related macular degeneration.4 Infantile nystagmus has a much wider impact than simply reducing vision. It affects social interaction, due to lack of confidence caused by the cosmetic appearance of nystagmus, and causes restriction in mobility of many patients, as they are not able to drive.5 Treatment of nystagmus should not only aim at improving visual acuity (VA) but also at improving cosmesis. This might include, for example, the correction of abnormal head postures and the reduction of nystagmus intensity in patients with poor visual potential. Patients may also benefit from counseling services and support groups such as:
Classification of infantile nystagmus
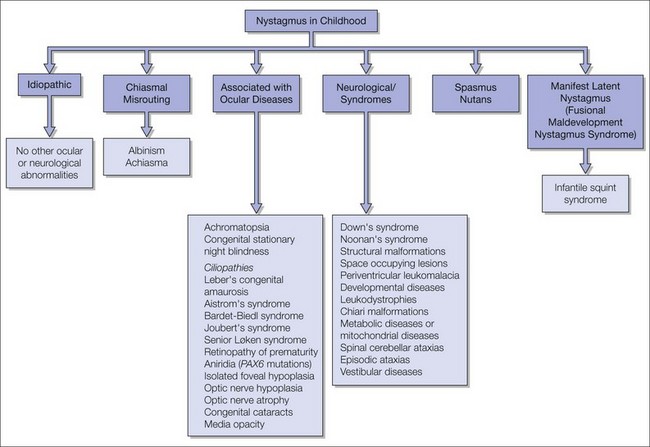
The advantages of using a classification of infantile nystagmus based on the associated diseases are that the clinical implications such as prognosis, possible genetic counseling, or treatment options are highlighted.6 Figure 89.2 lists examples of disorders using this type of classification. Idiopathic nystagmus is a diagnosis of exclusion where all other eye examinations are normal. VA is logMAR 0.3 (6/12, 20/40, 0.5) or better in most patients.7,8 Mutations in the FRMD7 gene have been identified as a major cause of X-linked idiopathic nystagmus.9,10 Several genetic mutations are known for other disorders such as albinism11,12 and achromatopsia.13 It is likely that the nystagmus genotype will be the principal method of classification in the future.
The Committee for the Classification of Eye Movement Abnormalities and Strabismus Workshop (CEMAS, http://www.nei.nih.gov/news/statements/cemas/pdf) have grouped idiopathic nystagmus, nystagmus associated with ocular diseases, and nystagmus associated with chiasmal misrouting into one category, “infantile nystagmus syndrome.” This classification makes unconfirmed assumptions about a common mechanism leading to nystagmus in all of the underlying pathologies.
Terminology used in nystagmus
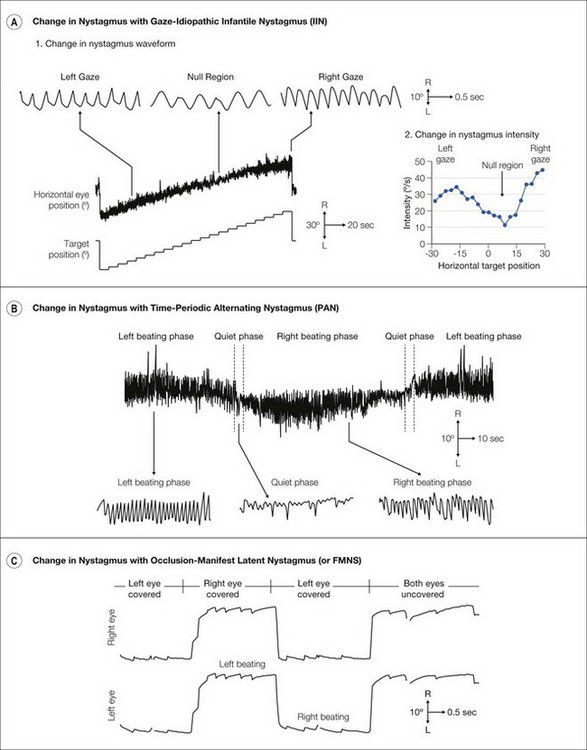
Nystagmus can be characterized by clinical examination of the patient. Eye movement recordings can provide greater precision in detecting and describing nystagmus waveforms which can assist in the diagnosis (Figs 89.3 and 89.4). The following parameters can be used to describe nystagmus:
Plane The plane of oscillation can be horizontal, vertical, torsional, or a combination of more than one plane (e.g. Fig. 89.3C,2).
Intensity The intensity of the nystagmus is a measure of the speed of the eye movements and is obtained by multiplying the nystagmus amplitude (in degrees) and frequency (oscillations per second in Hertz).
Waveform Nystagmus can be classified into jerk and pendular waveforms. Jerk nystagmus consists of alternating slow and quick phase eye movements. The nystagmus direction is defined using the quick phase. Slow phases can have increasing velocity profiles where the eyes start slowly and accumulate speed (e.g. Fig. 89.4A in right gaze). Alternatively, slow phases may have decreasing velocity (e.g. Fig. 89.4C) or linear velocity profiles. In contrast, pendular nystagmus consists of sinusoidal oscillations with small or no quick phases (e.g. Fig. 89.4A at null region). Dual jerk nystagmus is a combination of large jerk nystagmus waveforms with small pendular nystagmus waveforms superimposed along the same plane.
Conjugacy If both eyes move together, i.e. with the same amplitude, frequency and plane, the nystagmus is conjugate. Disconjugacy (dissociated nystagmus) occurs if the eyes move with different amplitude (e.g. torsional eye movements in Figure 89.3A,3), frequency, phase (e.g. vertical eye movements in Figure 89.3C,2), or along different planes.
Foveation Most types of infantile nystagmus show periods when the eyes move at a slower velocity. These slow periods are used to align the fovea to improve VA, and hence are called foveation periods.
Null region Many patients with infantile nystagmus prefer to use a particular gaze direction where the nystagmus is reduced in intensity and the VA is optimal. This is called the null region. If the null region is not in the primary position, patients may adopt an abnormal head posture (AHP) using the null region to improve vision when looking straight ahead (see Chapter 81). An example is shown in Figure 89.4A,2 where the null region is in right gaze.
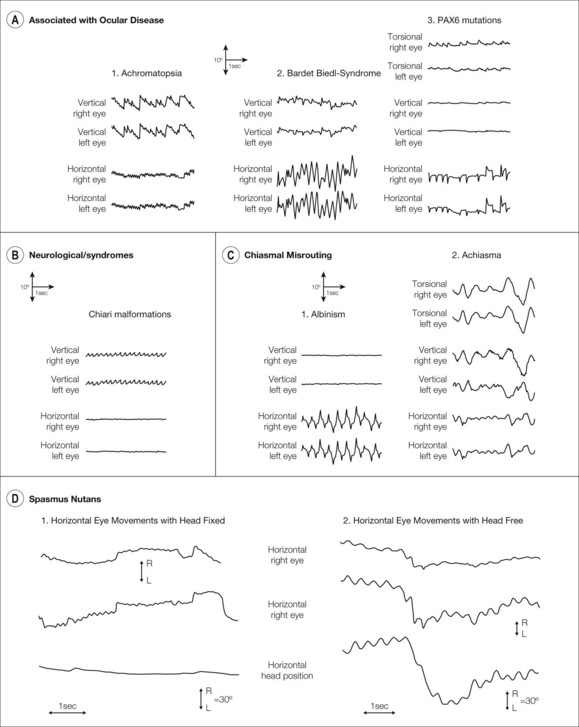
Fig. 89.3 The use of eye movement recordings in the diagnosis of nystagmus. Examples of eye movement recordings from patients with infantile nystagmus associated with (A) ocular diseases, (B) neurologic disorders and syndromes, (C) chiasmal misrouting disorders, and (D) spasmus nutans. (A) Ocular diseases. In achromatopsia a fine pendular nystagmus with a vertical component is often present. In the achromat shown (A,1) a fine mainly horizontal pendular nystagmus of 1−2° amplitude and 8 Hz frequency coexists with a vertical upbeat jerk nystagmus of approximately 5° amplitude and 1.5 Hz frequency. A patient with Bardet-Biedl syndrome (A,2) has horizontal pendular oscillations that are much larger than in the achromat (8−10° amplitude and 3 Hz frequency in the example shown) but the vertical component to the nystagmus is smaller. PAX6 mutations (A,3) lead to a variety of waveforms with the two eyes sometimes showing disconjugate eye movements. The example here shows unusual horizontal waveforms with both increasing and decreasing velocity components. A significant torsional component is apparent which is larger in the right eye. (B) Neurologic disorders and syndromes. These can be associated with vertical eye movements. The example shown is from a patient with a Chiari malformation leading to a downbeat jerk nystagmus of 2−3° amplitude and 3−4 Hz frequency with little horizontal nystagmus. (C) Chiasmal routing disorders. Similar to idiopathic infantile nystagmus (Fig. 89.4A), nystagmus associated with albinism (C,1) can have pendular or jerk waveforms but always along the horizontal plane and usually with a null region. Jerk waveforms can be left beating, right beating, or bidirectional as shown. Achiasmic disorders (C,2) lead to see-saw nystagmus: the eyes give the appearance of rotating around an invisible pivot positioned somewhere between the two eyes. As one eye moves up the other eye moves down leading to a disconjugate vertical waveform. The eye moving up intorts and the eye moving down extorts leading to a large amplitude torsional nystagmus. There is also a horizontal component to see-saw nystagmus. (D) Spasmus nutans. Nystagmus in spasmus nutans is altered by head movements. When the head is fixed, a rapid pendular oscillation develops which is disconjugate between the two eyes. When the head is free, head bobbing occurs with the eyes moving in the opposite direction due to the vestibulo-ocular reflex. This leads to suppression of the rapid oscillation.
(Reproduced from Gottlob I, Zubcov AA, Wizov SS, Reinecke RD. Head nodding is compensatory in spasmus nutans. Ophthalmology 1992; 99: 1024−31.)
Infantile nystagmus can change depending on several factors:
Change with gaze Patients with albinism and idiopathic nystagmus usually have a null region. The nystagmus becomes more jerk-like (Fig. 89.4A,1) and intense (Fig. 89.4A,2) away from the null region.
Change with time Most patients have a consistent oscillation when attempting to maintain a fixed gaze position. However, certain types of nystagmus vary with time. In periodic alternating nystagmus (PAN) the fast phase beats periodically to the right and to the left with quiet periods at the change-over periods (Fig. 89.4B).
Change upon covering one eye In manifest latent nystagmus (MLN) the fast phase of nystagmus changes direction beating toward the fixing eye (Fig. 89.4C).
Clinical assessment
History
As several forms of infantile nystagmus are hereditary, establishing whether other family members have nystagmus or associated ocular diseases can help with the diagnosis. If there is a positive family history, determining the mode of inheritance is important. Idiopathic nystagmus often occurs in an X-linked pattern in which heterozygous females are fully affected in approximately 50% of cases (i.e. 50% penetrance).9,10 In contrast, only males are fully affected in X-linked congenital stationary night-blindness,15 blue cone monochromatism,13 or ocular albinism.12 Oculocutaneous albinism11 and achromatopsia13 are usually autosomal recessive. The most common form of autosomal dominant nystagmus is caused by mutations in PAX6 genes.16
Establish whether the parents think the child has poor vision. Nystagmus can be of very large amplitude at onset and parents can have the impression that the child is visually unresponsive. Usually the amplitude is considerably smaller by 6 to 9 months of age17 ![]() Video 89.1). Explaining to parents that nystagmus changes and becomes less evident with age is important. Caution should be taken about predicting poor vision later in life.
Video 89.1). Explaining to parents that nystagmus changes and becomes less evident with age is important. Caution should be taken about predicting poor vision later in life.
Often children with nystagmus have head nodding or bobbing. This is an independent abnormal head movement which can decrease or disappear with age ![]() (Video 89.2). Only in spasmus nutans has head nodding been shown to be compensatory (minimizing the nystagmus) (Fig. 89.3D,
(Video 89.2). Only in spasmus nutans has head nodding been shown to be compensatory (minimizing the nystagmus) (Fig. 89.3D, ![]() Video 89.3).
Video 89.3).
Oscillopsia seldom occurs in infantile nystagmus. Some children, however, perceive oscillopsia if they look away from the null region18 or if the nystagmus changes, for example in MLN which can change with the degree of strabismus ![]() (Video 89.18). Oscillopsia in acquired nystagmus is usually sudden in onset and severe. When it occurs in infantile nystagmus, the time of onset is generally not well defined and the symptoms are milder.
(Video 89.18). Oscillopsia in acquired nystagmus is usually sudden in onset and severe. When it occurs in infantile nystagmus, the time of onset is generally not well defined and the symptoms are milder.
Clinical examination
Visual acuity
VA needs to be examined with the best optical correction and tested with both eyes open and either eye covered with a free head position. MLN, alone or superimposed on infantile nystagmus, can increase the nystagmus and decrease VA when one eye is covered. VA should be measured at distance and near. In infants, VA tests can be performed using preferential looking cards. In patients with horizontal nystagmus, measurement of VA can be assisted by vertically aligning the cards19 making it easier to identify changes in fixation when the child looks up or down. This can be masked by the horizontal nystagmus if the card is aligned horizontally. The presence of vertical (optokinetic nystagmus) OKN suggests the likelihood of better VA in horizontal nystagmus.
Abnormal head posture (torticollis)
AHP occurs commonly in nystagmus because patients can reduce their nystagmus by looking in a certain direction of gaze. In most patients, the full extent of torticollis is only observed during visual effort. To identify the full amount of AHP, ask the patient to read or look at pictures (Fig. 89.5A, ![]() Video 89.5). Glasses can prevent the patient adopting the full head turn due to the spectacle frame and optical decentration. VA measurements should be repeated, therefore, without spectacles. Figure 89.5B and
Video 89.5). Glasses can prevent the patient adopting the full head turn due to the spectacle frame and optical decentration. VA measurements should be repeated, therefore, without spectacles. Figure 89.5B and ![]() Video 89.6 show a child with idiopathic infantile nystagmus (IIN) and a right head turn increasing as he reads smaller letters. With a greater visual demand, a large head turn is adopted and he looks over his glasses or prefers to read without glasses since the full head turn is prevented by the glasses.
Video 89.6 show a child with idiopathic infantile nystagmus (IIN) and a right head turn increasing as he reads smaller letters. With a greater visual demand, a large head turn is adopted and he looks over his glasses or prefers to read without glasses since the full head turn is prevented by the glasses.