 he story of neovascular glaucoma never ends. The treatment—both medical and surgical—is difficult and failures are common. Lifelong follow-up and appropriate management are required. The Fugo blade, with its unique cutting properties, now offers a better way to handle this intractable condition.
he story of neovascular glaucoma never ends. The treatment—both medical and surgical—is difficult and failures are common. Lifelong follow-up and appropriate management are required. The Fugo blade, with its unique cutting properties, now offers a better way to handle this intractable condition.
The most important causes of neovascular glaucoma are central retinal vein occlusion, proliferative diabetic retinopathy, and branch-vein occlusion. Vascular endothelial growth factor is considered to be the cause of new vessel formation. Rubeosis of the iris and growth of a fibrovascular membrane over the trabecular meshwork cause a rise in intra-ocular pressure. Delayed diagnosis and unsuccessful medical management of neovascular glaucoma are common, as is the relentless progression of the disease toward painful glaucoma and blindness.
Surgical methods currently used to treat neovascular glaucoma include trabeculectomy with or without an antifibrotic agent, valve-implant surgery, and cyclodestructive procedures. Filtration surgery for neovascular glaucoma is particularly challenging. The fragile blood vessels from the angle of the anterior chamber start leaking the moment intra-ocular pressure falls during the course of any filtration surgery.
Dr. Singh first used the Fugo blade to treat neovascular glaucoma in a patient with an extremely painful blind eye. The patient’s intra-ocular pressure was over 60 mm Hg. After giving the patient a retrobulbar injection of lignocaine, Singh and Dow made a single transconjunctival transciliary filtration (TCF) track with a 100-µm Fugo blade tip. The patient never suffered pain in that eye again, although his intraocular pressure remained at around 35 mm Hg while taking local antiglaucoma medication.
We became interested in TCF for neovascular glaucoma for several reasons:
- No trauma to the vascularized angle of the anterior chamber occurs. The iris with rubeosis is not traumatized by iridectomy.
- A filtration channel is created through the ciliary body, which is free from neovascularization. No fibrovascular membrane forms at the site of the inner opening behind the iris. The filtration track is made through the relatively healthy tissues.
- Leaked blood in the anterior chamber does not conflict with the filtration track and is less of a cause of surgical failure than other more important factors, like fibrosis and inflammation.
We have operated on over a dozen cases of neovascular glaucoma, using two techniques: TCF after making a fornix-based conjunctival flap and the direct transconjunctival approach. In nearly half the cases, blood oozed from the angle of the anterior chamber during the course of surgery. Postoperative hyphema did not drain through the TCF track, but absorbed spontaneously over a period of days or weeks. Filtration failed as a result of subconjunctival scarring or tenon cyst formation. Reoperation was done whenever there was failure (almost 50% of cases). None of the patients who had progressed to a painful blind eye needed relief through a retrobulbar alcohol injection, a cyclodestructive procedure, or enucleation.
In all operated cases, neovascularization of the iris was seen to regress or disappear as long as the intraocular pressure was not high. The vision of these six patients was preserved; they all had branch-vein occlusion.
The ups and downs of surgical care of neovascular glaucoma are illustrated by the description of one patient, as shown below.
CASE STUDIES
Case 1
A 55-year-old woman with diabetes and multiple systemic problems had lost the vision in one eye to retinal detachment; the intra-ocular pressure in the other eye was over 40 mm Hg. There were vascular changes in the iris and the angle. Medical management with multiple local drops and oral acetazolamide (Diamox) were successful for about 6 months, after which the pressure shot up to 50 mm Hg and her vision rapidly deteriorated. Surgery was decided on.
As a preliminary treatment, paracentesis was done and bevacizumab (Avastin) injected in the anterior chamber. The operation was done the next day as described below.
Surgical Technique
- Visualize the surgical limbus under the conjunctiva. Make a depression mark 1 mm behind the limbus by pressing on it with the noncutting back side of a diamond blade (Fig. 34.1).
- Slide the loose conjunctiva about 4 to 5 mm proximal to the depression mark over the underlying tenon capsule, using the edge of a nonmagnetic noncutting blade. In our case, we used a purposely blunted diamond knife. In this state it did not cut when pressed on the eyeball, but it did hold down the dragged conjunctiva in the gutter made moments before. The gutter was about 1 mm away from the limbus.
- Set a 300-µm Fugo blade tip at medium power and high intensity. The tip is bent at a convenient angle to easily direct it toward the posterior chamber. Lightly push the activated tip along the edge of the diamond conjunctival rectractor. It instantly goes through the conjunctiva and partly through the sclera. Withdraw the tip, and touch it very briefly deeper in the track another two to three times until fluid starts to flow from the posterior chamber. Small air bubbles issue from behind the iris as they enter the anterior chamber. This ensures that the track is indeed in the posterior chamber.
- In our case, blood was seen leaking from many points in the angle of the anterior chamber. We therefore irrigated the eye from the TCF track. It helped to some extent, yet the leakage continued. To stem, it a large air bubble was introduced through the posterior chamber track (Fig. 34.2).
- For a further tamponade, make a stab incision at the limbus and inject sodium hyaluronate (Healon) into the anterior chamber.
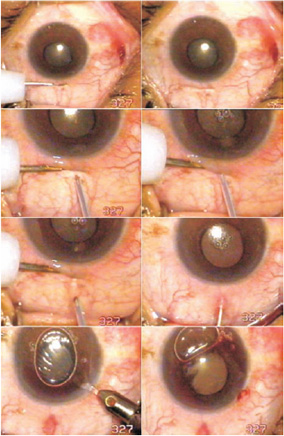
Figure 34.1. A linear scleral depression is made with a blunt nonmagnetic device. The conjunctiva is slid toward the limbus, activated, and pressed into the depression. Transconjunctival transciliary filtration is done with a 300-µm Fugo blade. Irrigation and air injection is done through the transciliary track. Sodium hyaluronate (Healon) is injected through a stab incision.
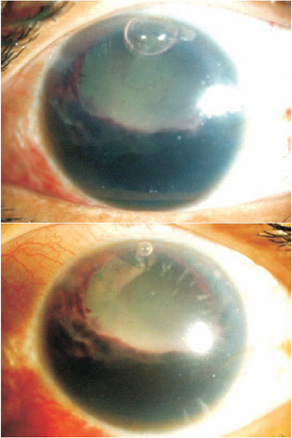
Figure 34.2. The anterior chamber before and 1 day after sodium hyaluronate removal.
It is not certain whether the injection of sodium hyaluronate helped in our case to retard the blood leaking from the fragile vessels in the angle, but it did raise the intra-ocular pressure. It may have do so by pressing the iris backward, which caused the internal opening in the ciliary body to close, and by occluding the angle of the anterior chamber. Therefore, as an emergency, sodium hyaluronate was aspirated within 4 hours of surgery. The blood ooze seen in the anterior chamber at the time of surgery was now manifesting as a blackball hemorrhage occupying the lower half of the anterior chamber (Fig. 34.2). It was left alone for the time being.
Postoperative Management
There was no significant spontaneous blood clearing in the coming days and the patient felt her vision slipping away. On the 4th postoperative day, urokinase (10,000 units per milliliter) was repeatedly irrigated in the anterior chamber to attack the blackball hemorrhage. There was partial success. The irrigating process pushed some dissolved blood through the transciliary track under the conjunctiva that appeared as a blood stain at the outer opening (Fig. 34.3). Intraocular pressure was still under control.
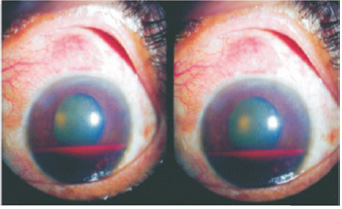
Figure 34.3. The anterior chamber 3 days after urokinase wash. The dark blood is clearly visible. The bleb is still functional.
The patient was comfortable and the blood was allowed to absorb spontaneously; eventually no blood remained. Intra-ocular pressure rose once again but was controlled with local and oral medications. Finally, 2 months later, the surgery failed completely. The patient was not in pain, but her sight was in jeopardy. A reoperation was done in an adjoining area, exactly as performed in the first procedure. Transconjunctival TCF was performed in an adjoining healthy area (Fig. 34.4). One month after the surgery (Fig. 34.5 and 35.6), the patient’s intra-ocular pressure had returned to normal and the anterior chamber was clear.
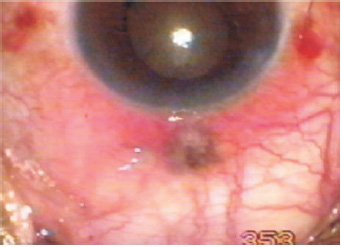
Figure 34.4. Transconjunctival transciliary filtration has been repeated on the temporal side of the failed track.
Figure 34.5. The filtering bleb under high power 1 month after repeat surgery. The image shows very clearly that the bleb is widespread and the conjunctiva is healthy and transparent.
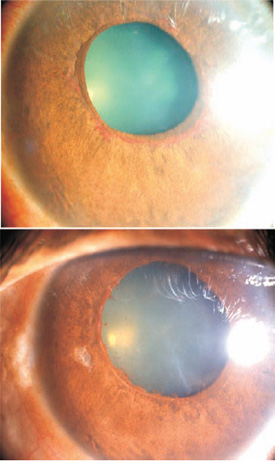
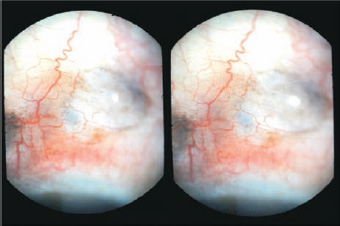
Figure 34.6. Preoperatively there was new vessel formation close to the pupil. One month after surgery, no neovascularization is apparent.
Case 2
The following case describes TCF surgery in a case of neovascular glaucoma. The anterior chamber was full of blood.
Surgical Technique
- After detaching the conjunctiva from the limbus and obtaining hemostasis, make a scleral pit on the sclera 1.5 mm from the limbus (Fig. 34.7).
- Apply a small sponge soaked with mitomycin to the undersurface of the retracted conjunctiva.
- Clear blood from the anterior chamber by irrigation and aspiration through two different ports.
- Reach the posterior chamber by ablating through the ciliary body with a 100-µm Fugo blade at maximum energy settings.
- Repeat two-port irrigation and aspiration to wash out the anterior chamber.
- Suture the conjunctiva.
- Inject intravitreal bevacizumab.
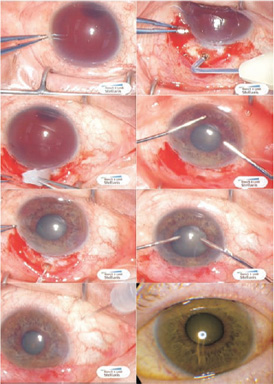
Figure 34.7. Top left to bottom right: Neovascular glaucoma with hyphema; transciliary filtration scleral ablation; mitomycin application; anterior chamber washout of hyphema; transciliary filtration penetration; repeat anterior chamber washout after wound suture; intravitreal bevacizumab injected; patient’s appearance on 6th postoperative day shows complete regression of rubeosis (intra-ocular pressure, 7 mm Hg).
Neovascular glaucoma is an intractable disease, and surgery often fails. The Fugo blade offers the surgeon a variety of credible solutions for the treatment of this condition. Transconjunctival TCF seems to be the least traumatic choice and can be redone at the original failed track or in an adjoining area.
New vessel formation in the iris decreases or disappears as the intra-ocular pressure is controlled. The use of anti–vascular endothelial growth factor medicine in the anterior chamber probably helps. We have limited experience, but mitomycin might be a useful adjunct to treatment. Dark-skinned patients do not have a predictable response.
Suggested Reading
Albert DM, Jakobiec FA. Neovascular glaucoma. In: Principles and practice of ophthalmology, clinical ophthalmology [book on CD-ROM]. Philadelphia, Pa: Saunders, chapter 215.
Epstein DL, Allingham RR, Schuman JS. Chandler and Grant’s glaucoma. 4th ed. Philadelphia, Pa: Lea & Febiger, 1997:309–318.
Gupta V, Agarwal HC. Contact trans-scleral diode laser cyclophotocoagulation treatment for refractory glaucomas in the Indian population. Indian J Ophthalmol. 2000; 48:295–300.
Lieberman MF, Ewing RH. Drainage implant surgery for refractory glaucoma. Int Ophthalmol Clin. 1990;30:198–208.
Parodi MB, Iacono P. Photodynamic therapy with verteporfin for anterior segment neovascularizations in neovascular glaucoma. Am J Ophthalmol. 2004;138:157–158.
Shields MB. Textbook of glaucoma. 4th ed. 1998:269–286. Sivak-Callcott JA, O’Day DM, Gass JD. Evidence-based recommendations for the diagnosis and treatment of neovascular glaucoma. Ophthalmology. 2001;108:1767–1800.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree