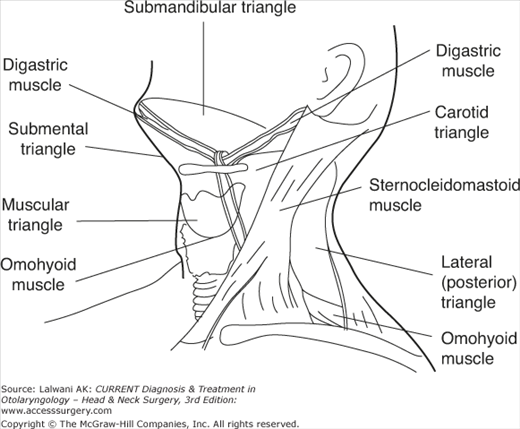
Anatomy
Knowledge of the anatomy of the neck is essential for both the diagnosis and the treatment of disease processes in the region. Contained within the neck are several triangles, defined anatomically (Figure 27–1). Familiarity with these specific areas assists in generating a differential diagnosis of neck masses by the exact anatomic location.
The following anatomic points define the anterior compartment of the neck: (1) the inferior border of the mandible superiorly, (2) the anterior border of the sternocleidomastoid muscle laterally, (3) the clavicle inferiorly, and (4) the vertical midline from mental symphysis to suprasternal notch medially. The structures that make up the anterior neck include the larynx, trachea, esophagus, thyroid and parathyroid glands, carotid sheath, and suprahyoid and infrahyoid strap muscles.
Triangular regions also define the anterior neck anatomically.
The submandibular triangle is a region contained in the anterior neck bordered by the inferior margin of the mandible and the digastric, stylohyoid, and mylohyoid muscles. This region contains the submandibular gland and the marginal mandibular branch of the facial nerve. The submental triangle defines a region bordered by the hyoid bone, the paired anterior bellies of the digastric muscles, and the mylohyoid muscle. The upper belly of the omohyoid muscle in the anterior neck further divides the anterior neck into an upper carotid triangle and a lower muscular triangle.
The lateral neck, also referred to as the posterior triangle, is defined by the posterior aspects of the sternocleidomastoid muscle medially, the trapezius muscle laterally, and the middle third of the clavicle inferiorly. The lateral neck contains lymph node-bearing tissue, the spinal accessory nerve, and the cervical plexus. The inferior belly of the omohyoid muscle further defines a lower subclavian triangle in the lateral neck that contains the brachial plexus and subclavian vessels.
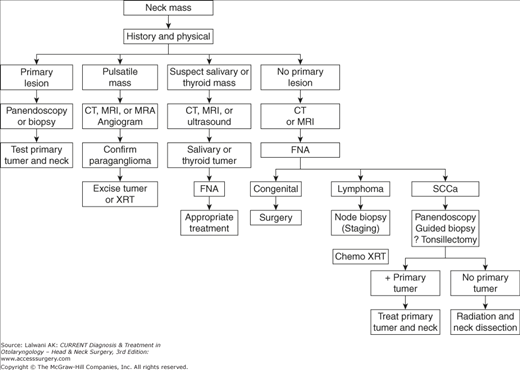
Diagnosis
The differential diagnosis in a patient presenting with a neck mass is broad and extensive. Therefore, a thorough history and physical examination make up the critical first step in the evaluation of a neck mass. Information gathered from a detailed history and physical examination alone often narrows the differential diagnosis to a more manageable level (Figure 27–2).
The most important element in the evaluation of a neck mass is the age of the patient. Most pediatric neck masses are inflammatory or congenital and resolve spontaneously or after appropriate medical therapy. In contrast, a neck mass in an adult over the age of 40 should be considered neoplastic in origin unless proven otherwise. The probability of a benign neck mass in this age group is low, particularly in the setting of tobacco or alcohol use.
The duration, growth pattern, and absence or presence of pain are all critical aspects of the history. A region-specific review of systems, such as a change in voice, hoarseness, difficulty with swallowing, and ear pain are important symptoms to note in addition to generalized complaints such as fever, night sweats, and weight loss. Questions related to a patient’s social history, such as alcohol and drug use, smoking, and recent travel, should also be included.
The physical examination should include a systematic investigation of all mucosal and submucosal areas of the head and neck. The mobility, consistency, and tenderness of the mass should be assessed carefully. The location of the neck mass is particularly important in congenital and developmental masses because these masses typically appear in consistent locations. For example, a lateral neck mass in a child is suggestive of a branchial cleft cyst or laryngocele, whereas a midline neck mass is more suggestive of a thyroglossal duct cyst. The location also may be helpful in assessing adult patients. A neck mass located in the supraclavicular region of an older adult should focus the physician’s attention to metastasis from a primary lesion located in a site other than the upper aerodigestive tract (eg, a gastrointestinal or pulmonary source). An isolated posterior triangle lymph node in an Asian adult should raise suspicion for a nasopharyngeal carcinoma.
Imaging studies provide useful information in diagnosing the etiology of a neck mass. Computed tomography (CT) and magnetic resonance imaging (MRI) can (1) differentiate solid, cystic, and vascular masses; (2) localize a mass in relation to the vital structures of the neck; and (3) identify a potential head and neck source for the neck mass. Ultrasonography may be helpful in distinguishing solid from cystic masses, especially in the setting of a suspected thyroid lesion. Chest X-rays may be helpful if there is a high index of suspicion for granulomatous diseases such as sarcoidosis or tuberculosis. A chest film is also able to detect a metastasis from a head and neck cancer or a primary malignant neoplasm within the lungs. Positron emission tomography (PET), which detects increased metabolic activity, is now often used in the detection and surveillance of head and neck cancer.
Serologic testing can be used in looking for systemic diseases. For example, antinuclear antibody may be positive in Sjogren syndrome, which can present with parotid enlargement and lymphadenopathy. Serologic testing is also important in the diagnosis of many infectious diseases that may present as a neck mass, including tuberculosis, atypical mycobacteria, mononucleosis, toxoplasmosis, and cat-scratch disease. Patients with lymphoma may also have abnormalities on serologic testing.
Fine-needle aspiration (FNA) biopsy has become a critical step in the evaluation of neck masses. The timing of the FNA biopsy in relation to imaging studies is debatable. Advocates of obtaining imaging studies prior to the FNA biopsy believe that the FNA distorts the architecture of the mass, thus making imaging more difficult to interpret. The procedure for a FNA entails the use of a 23- or 25-gauge needle in obtaining multiple aspirations of the neck mass. FNA biopsies can differentiate a cystic mass from an inflammatory mass and malignant tissue from benign tissue. It is important to know that FNA can differentiate lymphoma from carcinoma, a distinction that is critical in directing further workup and treatment. With the recent advances in molecular biology, polymerase chain reaction (PCR) can be conducted on FNA samples to identify disease processes such as Epstein–Barr virus (EBV), which will guide the physician to the diagnosis of primary nasopharyngeal carcinoma. When there is a suspicion on squamous cell carcinoma, FNA aspirates of a neck mass can also be analyzed for human papilloma virus (HPV), which has been implicated in oropharyngeal squamous cell carcinoma. Patients who are positive for HPV tend to be younger, nonsmokers, and nondrinkers. The primary tumor can usually be found in the tonsil or base of tongue region. These patients also have a much better prognosis than those who are HPV negative.
Congenital Neck Masses
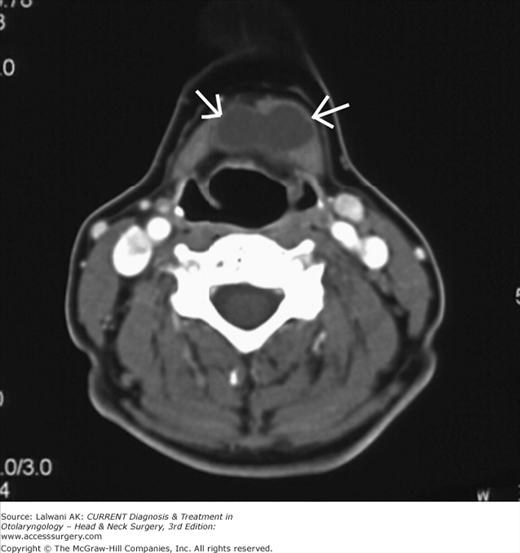
Branchial cleft cysts arise from the failure of the pharyngobranchial ducts to obliterate during fetal development. They most frequently present in late childhood or early adulthood, when the cysts become infected—usually after an upper respiratory tract infection. A branchial cleft cyst appears as a tender, inflammatory mass located at the anterior border of the sternocleidomastoid muscle (Figure 27–3).
Branchial cleft cysts fall into three categories: first, second, and third branchial cleft anomalies.
First branchial cleft anomalies make up less than 1% of all branchiogenic anomalies and usually appear on the face or near the auricle. There are two types of first branchial anomalies, Type I and Type II.
Type I first branchial cleft cysts are duplication anomalies of the external canal and are composed of ectodermally derived tissue. They may pass into the parotid gland and close to the facial nerve.
Type II anomalies may comprise ectodermally and mesodermally derived tissues. These lesions typically present below the angle of the mandible, pass through the parotid gland in close proximity to the facial nerve, and end either inferior to the external auditory canal or into the canal at the bony cartilaginous junction.
Second branchial cleft anomalies are the most common of the three types. They present as discrete, rounded masses below the angle of the mandible and at the anterior border of the sternocleidomastoid muscle. The potential tract of an associated sinus passes deep to the second arch structures (eg, the external carotid artery and the stylohyoid and digastric muscles) and superficial to the third arch derivatives (eg, the internal carotid artery), opening into the tonsillar fossa.
Third branchial cleft cysts present anterior to the sternocleidomastoid muscle and lower in the neck than either first or second branchial cleft anomalies. Third branchial cleft cysts are deep to the third arch derivatives (eg, the glossopharyngeal nerve and the internal carotid artery) and superficial to fourth arch derivatives (eg, the vagus nerve). These anomalies end in the pharynx at the thyrohyoid membrane or pyriform sinus.
The management of branchial cleft anomalies is initial control of the infection followed by surgical excision of the cyst and tract. As a general rule, incision and drainage procedures should be avoided; however, they may be necessary for acute abscess treatment before definitive excision. Needle aspiration and decompression can be beneficial in preventing incision and drainage, which increases the difficulty of definitive excision.
Thyroglossal duct cysts present as midline masses of the anterior neck (Figure 27–4). Like branchial cleft cysts, they may be asymptomatic and appear only when they become infected in the setting of an upper respiratory tract infection. Thyroglossal duct cysts make up approximately one-third of all congenital neck masses. Their location may be variable at times, with some cysts presenting more laterally (ie, superior to the hyoid) or as low as the level of the thyroid gland. Thyroglossal duct cysts that occur off the midline may be difficult to differentiate from branchial cleft cysts. A pathognomonic sign on physical examination is vertical motion of the mass with swallowing and tongue protrusion, demonstrating the intimate relation to the hyoid bone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree