CHAPTER 121 Neck Dissection
Historical Perspective
In publications that came out before the 20th century, little attention was given to the indications or techniques for treating cervical lymph node metastases. The first conceptual approach for removing nodal metastases was made by Kocher in 18801; he described the removal of the lymph nodes located within the contents of the submandibular triangle to gain surgical access to a cancer of the tongue. Later, Kocher recommended that nodal metastases should be removed more widely through a Y-shaped incision, with the long arm extending from the mastoid to the level of the omohyoid at its junction with the anterior border of the sternocleidomastoid muscle. Around the same time, Packard supported the concept of removing the surrounding lymph nodes for lingual cancer.2 The first description of the radical neck dissection was by Jawdynski, a Polish surgeon.3 However, the individual credited the most for developing and reporting the efficacy of this procedure is George Crile.4 Crile believed that distant (hematogenous) metastases were uncommon in head and neck cancer and that metastases more commonly occurred in the neck through the permeation of lymphatics. The descriptions by both of these surgeons of a block resection encompassing all of the cervical nodal groups from the level of the mandible above to the clavicle below became the basis for the radical neck dissection we know today. Relevant to the modifications of radical neck dissection that were subsequently made, Crile recommended preservation of the internal jugular vein and the sternocleidomastoid muscle for patients in whom there were no palpable nodes. In addition, his technique was to remove only the regional lymph nodes that were known to drain the field of the original focus of disease when metastases could not be seen. Also, it is interesting to note that, in the accompanying illustrations of the more radical en bloc resections, the spinal accessory nerve was preserved.
This philosophy of radical en bloc resection based on Crile’s descriptions remained popular with the head and neck surgeons during the first half of the 20th century, in part because of the works of Blair and Brown5 and Martin,6 who were strong proponents of the radical en bloc technique of neck dissection in a manner similar to the radical surgery that had evolved for breast cancer. Martin, in particular, categorically insisted that the spinal accessory nerve, internal jugular vein, and sternocleidomastoid muscle should be removed as part of all cervical lymphadenectomies. It may be useful to remember that, during this time, radiotherapy had not yet been developed as an effective adjuvant modality, and radical surgery represented the only hope for cure.
Associated with the procedure of the radical neck dissection was the presence of significant postoperative morbidity related to shoulder dysfunction; the operation also had limitations as a bilateral procedure.7 In the 1950s Ward and Robben8 reported that the neck dissection could be modified in some circumstances by sparing the spinal accessory nerve and thereby preventing postoperative shoulder drop. Later, Saunders, Hirata, and Jaques9 compared the functional results of cases undergoing radical neck dissection with those in whom the spinal accessory nerve was spared; this demonstrated that shoulder symptoms were only mild or moderate in more than 80% of the patients who had the nerve preserved or cable grafted. The concept of conservation neck surgery was further popularized during the 1960s by Suarez10 in Argentina and promoted by Bocca and Pignataro,11 who independently described an operation that removed all of the lymph node groups while sparing the spinal accessory nerve, sternocleidomastoid muscle, and internal jugular vein. They emphasized that fascial compartments surrounding the lymphatic contents of the neck could be removed without sacrificing the nonlymphatic structures, as mentioned.
Other authors reported the sparsity of nodal disease within the posterior triangle for carcinoma of the oral cavity, pharynx, and larynx, thus setting the stage for modifications directed toward preserving lymph node groups.12–15 These observations paved the way for another type of neck dissection modification: one in which there was selective preservation of one or more lymph node groups.16–18 Some of the initial proponents of this concept were the surgeons at MD Anderson Cancer Center, who called the procedure “modified neck dissection.”19,20 Two of the variations of the modified neck dissection were also called “supraomohyoid” and “anterior” neck dissections.16 However, the term selective neck dissection (SND) subsequently became associated with the concept of preserving lymph nodes in one or more of the neck levels through the American Academy of Otolaryngology’s classification.17,21 The lymph node groups removed are based on the pattern of metastases, which are predictable relative to the primary site of cancer.
Terminology of Neck Dissection
The evolution of cervical lymphadenectomy procedures during the 20th century has provided the modern head and neck surgeon with a repertoire of surgical techniques for removing nodal metastases. Concurrent with this expansion has been the emergence of a multitude of terms used to describe these procedures. Originally proposed by authors without any uniformity of terminology, this lack of standardization unfortunately resulted in redundancy, misinterpretation, and even confusion among clinicians. Realizing the importance for standardizing the diverse nomenclature, the Committee for Head and Neck Surgery and Oncology of the American Academy of Otolaryngology–Head and Neck Surgery convened a special task force in 1988 to address the problems of terminology related to cervical lymphadenectomy. The specific objectives of the group were as follows: (1) to recommend terminology that adhered to more traditional terms such as “radical” and “modified radical” neck dissection, and to avoid the use of eponyms and acronyms; (2) to define which lymphatic structures and other nonlymphatic structures should be removed or preserved relative to the radical neck dissection; (3) to provide standard nomenclature for the lymph node groups and the nonlymphatic structures; (4) to define the boundaries of resection for lymph node groups; (5) to use terms for the neck dissection procedures that are basic and easy to understand; and (6) to develop a classification on the basis of the biology of the cervical metastases and the principles of oncologic surgery.17
Recently updated by the Committee for Neck Dissection Classification of the American Head and Neck Society (AHNS), the classification is outlined in Table 121-1).9,22,23 The new versions included modifications of the original classification in an effort to remain contemporary and to follow the current philosophy of managing lymph node metastases.
Table 121-1 Types of Neck Dissection
| Terminology | Definition |
|---|---|
| Radical | Removal of lymph node levels I to V, sternocleidomastoid muscle, spinal accessory nerve, and internal jugular vein. |
| Modified | Removal of lymph node levels I to V (as in radical neck dissection [ND]), but preservation of at least one of the nonlymphatic structures (sternocleidomastoid muscle, spinal accessory nerve, and internal jugular vein). |
| Selective | Preservation of one or more lymph node levels relative to a radical ND. |
| Extended | Removal of an additional lymph node level or group or a nonlymphatic structure relative to a radical ND (muscle, blood vessel, nerve). Examples of other lymph node groups are superior mediastinal, parapharyngeal, retropharyngeal, peri-parotid, postauricular, suboccipital, and buccinator. Examples of other nonlymphatic structures are external carotid artery, hypoglossal, and vagus nerves. |
Cervical Lymph Node Groups
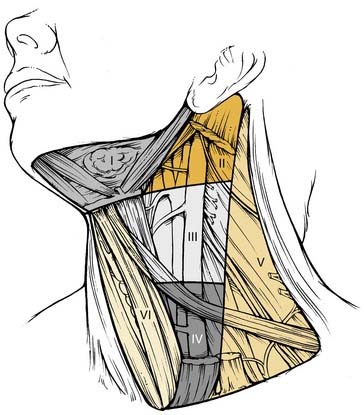
The patterns of spread of cancer from various primary sites in the head and neck to the cervical lymph nodes have been documented by retrospective analyses of large series of patients undergoing neck dissection.12,16,24 The nodal groups at risk for involvement are widespread throughout the neck, extending from the mandible and skull base superiorly to the clavicle inferiorly and from the posterior triangle of the neck laterally to the midline viscera and to the contralateral side of the neck. It is now recommended that the lymph node groups in the neck be categorized according to the level system originally described by the Memorial Sloan-Kettering Group (Fig. 121-1).19
Level VI encompasses the lymph nodes of the anterior compartment of the neck.19,21 This group is made up of nodes that surround the midline visceral structures of the neck, extending from the level of the hyoid bone superiorly to the suprasternal notch inferiorly. On each side, the lateral boundary is formed by the medial border of the carotid sheath. Located within this compartment are the perithyroidal lymph nodes, paratracheal lymph nodes, lymph nodes along the recurrent laryngeal nerves, and precricoid (Delphian) lymph node. These lymph nodes and their connecting lymphatic channels represent pathways of spread from primary cancers originating in the thyroid gland, apex of the piriform sinus, subglottic larynx, cervical esophagus, and cervical trachea.
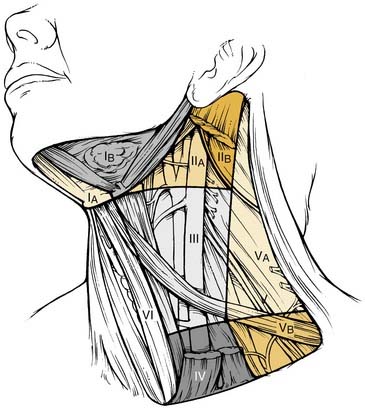
Division of Neck Levels by Sublevels
The 2001 report of the American Head and Neck Society’s Neck Dissection Committee recommended the use of sublevels for defining selected lymph node groups within levels I, II, and V on the basis of the biologic significance, independent of the larger zone in which they lay.21 These are outlined in Figure 121-2 as sublevels IA (submental nodes), IB (submandibular nodes), IIA and IIB (together composing the upper jugular nodes), VA (spinal accessory nodes), and VB (transverse cervical and supraclavicular nodes). The boundaries for each of these sublevels are defined in Table 121-2.
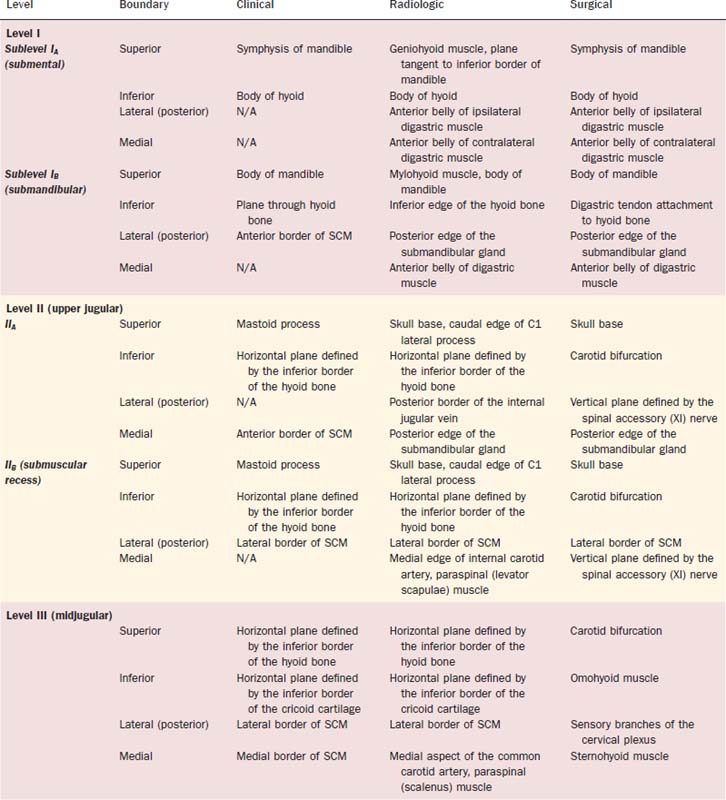
Table 121-2 Lymph Node Groups Found within the Six Neck Levels and the Six Sublevels
| Lymph Node Group | Description |
|---|---|
| Submental (sublevel IA) | Lymph nodes within the triangular boundary of the anterior belly of the digastric muscles and the hyoid bone; these nodes are at the greatest risk of harboring metastases from cancers arising from the floor of the mouth, anterior oral tongue, anterior mandibular alveolar ridge, and lower lip (see Fig. 121-2). |
| Submandibular (sublevel IB) | Lymph nodes within the boundaries of the anterior belly of the digastric muscle, the stylohyoid muscle, and the body of the mandible, including the preglandular and postglandular nodes and the prevascular and postvascular nodes. The submandibular gland is included in the specimen when the lymph nodes within this triangle are removed. These nodes are at greatest risk for harboring metastases from cancers arising from the oral cavity, the anterior nasal cavity, and the soft tissue structures of the midface and the submandibular gland (see Fig. 121-3). |
| Upper jugular (sublevels IIA and IIB) | Lymph nodes located around the upper third of the internal jugular vein and the adjacent spinal accessory nerve, extending from the level of the skull base above to the level of the inferior border of the hyoid bone below. The anterior (medial) boundary is the stylohyoid muscle (the radiologic correlate is the vertical plane defined by the posterior surface of the submandibular gland), and the posterior (lateral) boundary is the posterior border of the sternocleidomastoid muscle. Sublevel IIA nodes are located anterior (medial) to the vertical plane defined by the spinal accessory nerve. Sublevel IIB nodes are located posterior (lateral) to the vertical plane defined by the spinal accessory nerve. The upper jugular nodes are at greatest risk for harboring metastases from cancers arising from the oral cavity, nasal cavity, nasopharynx, oropharynx, hypopharynx, larynx, and parotid gland (see Fig. 121-3). |
| Middle jugular (level III) | Lymph nodes located around the middle third of the internal jugular vein, extending from the inferior border of the hyoid bone above to the inferior border of the cricoid cartilage below. The anterior (medial) boundary is the lateral border of the sternohyoid muscle, and the posterior (lateral) boundary is the posterior border of the sternocleidomastoid muscle. These nodes are at greatest risk for harboring metastases from cancers arising from the oral cavity, nasopharynx, oropharynx, hypopharynx, and larynx (see Fig. 121-3). |
| Lower jugular (level IV) | Lymph nodes located around the lower third of the internal jugular vein, extending from the inferior border of the cricoid cartilage above to the clavicle below. The anterior (medial) boundary is the lateral border of the sternohyoid muscle, and the posterior (lateral) boundary is the posterior border of the sternocleidomastoid muscle. These nodes are at greatest risk of harboring metastases from cancers arising from the hypopharynx, thyroid, cervical esophagus, and larynx (see Fig. 121-3). |
| Posterior triangle (sublevels VA and VB) | This group is composed predominantly of the lymph nodes located along the lower half of the spinal accessory nerve and the transverse cervical artery. The supraclavicular nodes are also included in the posterior triangle group. The superior boundary is the apex formed by the convergence of the sternocleidomastoid and trapezius muscles; the inferior boundary is the clavicle, the anterior (medial) boundary is the posterior border of the sternocleidomastoid muscle, and the posterior (lateral) boundary is the anterior border of the trapezius muscle. Sublevel VA is separated from sublevel VB by a horizontal plane marking the inferior border of the anterior cricoid arch. Thus sublevel VA includes the spinal accessory nodes, whereas sublevel VB includes the nodes that follow the transverse cervical vessels and the supraclavicular nodes (with the exception of Virchow’s node, which is located in level IV). The posterior triangle nodes are at greatest risk for harboring metastases from cancers arising from the nasopharynx, oropharynx, and cutaneous structures of the posterior scalp and neck (see Fig. 121-3). |
| Anterior compartment (level VI) | Lymph nodes in this compartment include the pretracheal and paratracheal nodes, the precricoid (Delphian) node, and the perithyroidal nodes, including the lymph nodes along the recurrent laryngeal nerves. The superior boundary is the hyoid bone, the inferior boundary is the suprasternal notch, and the lateral boundaries are the common carotid arteries. These nodes are at greatest risk for harboring metastases from cancers arising from the thyroid gland, glottic and subglottic larynx, apex of the piriform sinus, and cervical esophagus (see Fig. 121-2). |
| Superior mediastinum (optional—level VII) | These nodes represent an extension of the paratracheal lymph nodes chain extending inferiorly below the suprasternal notch along each side of the cervical trachea to the level of the innominate artery. |
The risk of nodal disease in sublevel IIB is greater for tumors arising in the oropharynx as compared with the oral cavity and larynx.25–32 Thus in the absence of clinical nodal disease in sublevel IIA, it is likely not necessary to include sublevel IIB for tumors arising in these latter sites. The dissection of the node-bearing tissue of sublevel IIB (submuscular recess) creates a risk of morbidity. Adequate exposure necessitates significant manipulation of the spinal accessory nerve and may account for trapezius muscle dysfunction observed in a significant minority of patients after an SND. Sublevel IA is a zone from which many surgeons do not remove lymph nodes unless the primary cancer involves the floor of the mouth, the lip, or structures of the anterior midface or there is obvious lymphadenopathy.
Correlation of Neck Level Boundaries with Anatomic Markers Depicted Radiologically
Radiologists have now identified landmarks that more accurately identify the location of lymph nodes according to the level system (Table 121-3).33,34 Using radiologic landmarks, level I includes all of the nodes above the level of the lower body of the hyoid bone, below the mylohyoid muscles, and anterior to a transverse line drawn on each axial image through the posterior edge of the submandibular gland. Level IA represents those nodes that lie between the medial margins of the anterior bellies of the digastric muscles, above the level of the lower body of the hyoid bone, and below the mylohyoid muscle (these were previously classified as submental nodes). Level IB represents the nodes that lie below the mylohyoid muscle, above the level of the lower body of the hyoid bone, posterior and lateral to the medial edge of the ipsilateral anterior belly of the digastric muscle, and anterior to a transverse line drawn on each axial image tangent to the posterior surface of the submandibular gland on each side of the neck (these are also referred to as submandibular nodes). Level II extends from the skull base at the lower level of the bony margin of the jugular fossa to the level of the lower body of the hyoid bone. Level II nodes lie anterior to a transverse line drawn on each axial image through the posterior edge of the sternocleidomastoid muscle, and they lie posterior to a transverse line drawn on each axial scan through the posterior edge of the submandibular gland. However, any nodes that lie medial to the internal carotid artery (ICA) are retropharyngeal and thus not level II.
Neck Dissection Classification
The classification for neck dissection recommended by the American Head and Neck Society’s committee is based on the following rationale: (1) that radical neck dissection is the standard basic procedure for cervical lymphadenectomy, and all other procedures represent one or more modifications of this procedures; (2) when the modification of the radical neck dissection involves the preservation of one or more nonlymphatic structures, the procedure is called modified radical neck dissection; (3) when the modification involves the preservation of one or more lymph node groups that are routinely removed in the radical neck dissection, the procedure is called SND; and (4) when the modification involves the removal of additional lymph node groups or nonlymphatic structures relative to the radical neck dissection, the procedure is called extended radical neck dissection (see Table 121-1).
Radical Neck Dissection
DEFINITION
This procedure includes the removal of all ipsilateral cervical lymph node groups extending from the body of the mandible superiorly to the clavicle inferiorly and from the lateral border of the sternohyoid muscle, hyoid bone, and contralateral anterior belly of the digastric muscle anteriorly to the anterior border of the trapezius muscle posteriorly.22 Included are all lymph node groups from levels I through V, the spinal accessory nerve, the internal jugular vein, and the sternocleidomastoid muscle (Fig. 121-3). It does not include the removal of the postauricular and suboccipital nodes, the periparotid nodes (except for a few nodes located in the tail of the parotid gland), the perifacial and buccinator nodes, the retropharyngeal nodes, and the paratracheal nodes.
Technique
INCISION PLANNING
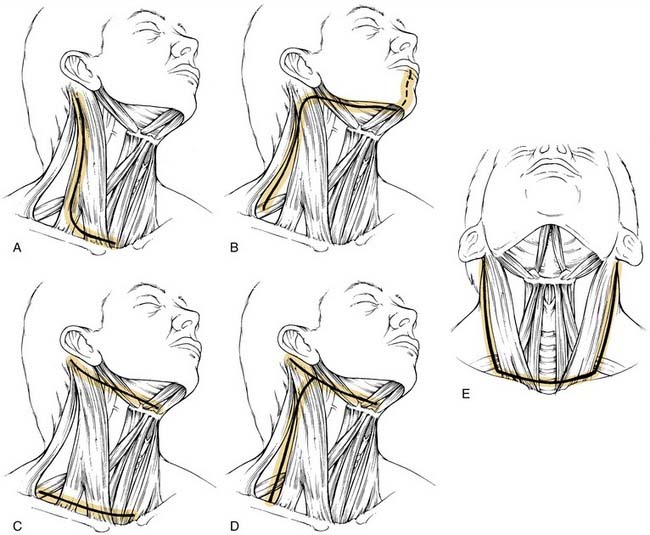
The incision is planned for optimal exposure of all lymph node levels to be dissected (levels I to V) and to preserve as much blood supply as possible. The neck flaps raised should be broadly based, either superiorly or inferiorly, and preferably to avoid any trifurcations, particularly overlying the carotid sheath. Incisions that best fit these criteria are the hockey stick and boomerang patterns; the McFee incision; and, in patients undergoing bilateral neck dissection, the apron incision, which is a bilateral hockey stick incision (Fig. 121-4). Other incisions use trifurcations that overlie the carotid sheath, although modifications of the Schobinger incision include placing the trifurcation more laterally based. Although the boomerang incision may be somewhat less aesthetically pleasing, it is an excellent alternative to use in conjunction with oral cavity and oropharyngeal tumors wherein exposure of the primary site involves extending the incision through the lip for a mandibulotomy approach.
FLAP ELEVATION
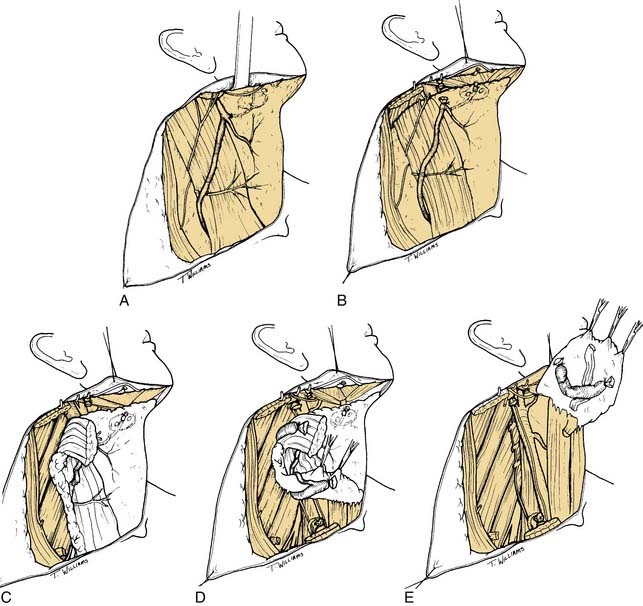
The initial incision is carried through skin and platysma muscle, although the platysma is deficient in the midline and the lateral-most parts of the incision. This anatomic feature can be used to reapproximate the flaps at the time of closure because the platysmal muscle edges serve as “natural hash marks.” The flap is raised in the subplatysmal plane so that the external jugular vein and the greater auricular nerves are not included in the flap (Fig. 121-5A). Although these structures will ultimately be sacrificed in the radical neck dissection, in SND procedures, they are routinely preserved. When there is gross pathologic evidence of tumor extension through the platysma muscle, with or without skin involvement, the area of disease involvement should also be removed and modifications of the skin flap may be required. Identification of the mandibular branch of the facial nerve is performed after complete elevation of the skin flaps superiorly and inferiorly to expose all of the lymph node levels of the neck. It is recommended that the anterior facial vein be ligated and retracted superiorly to protect this nerve only after the superior skin flap is raised. This allows proper assessment of the prevascular and postvascular lymph nodes in the submandibular triangle, which will need to be removed. Therefore it is best to incise the submandibular fascia at the lower border of the submandibular gland and to carefully raise this fascia off of the submandibular gland superiorly to the level of the lower border of the mandible as a separate flap. Usually the mandibular branch of the facial nerve may be seen as this fascia is raised (see Fig. 121-5B).
DISSECTION OF THE POSTERIOR TRIANGLE
The subsequent order of dissection is a matter of individual preference, although there is some oncologic rationale for dissecting from below upward rather than from above downward. Thus the next step is to expose the anterior border of the trapezius muscle from its superior aspect, where it converges with the posterior border of the sternocleidomastoid muscle, to its inferior aspect, where it approaches the clavicle (see Fig. 121-5C). The fibrofatty tissue is then incised along its anterior border beginning superiorly and working inferiorly to expose the muscular floor of the posterior triangle. In so doing, the spinal accessory nerve will be severed at the point at which it enters the trapezius muscle in the lower aspect of the posterior triangle. After this step has been completed, the floor of the posterior triangle at its inferior extent is next exposed by incising through the fibrofatty tissue immediately above the superior border of the clavicle. This requires incising through the inferior belly of the omohyoid muscle and the fibrofatty tissue overlying the brachial plexus. In this region, the transverse facial artery will be encountered immediately overlying the muscular floor of the triangle; this artery should be preserved unless there is gross disease involving the region. The fibrofatty contents of the posterior triangle are then mobilized anteriorly, lifting them away from the floor of the neck, which, in this region, is formed by the splenius capitis, levator scapulae, and scalene muscles. It is important to remain superficial to the prevertebral fascia during this step of the operation to prevent injury to the phrenic nerve and the brachial plexus. As the fibrofatty tissue is swept in a lateral-to-medial direction, the sensory branches of the cervical plexus will be encountered and divided.
ANTERIOR TRIANGLE DISSECTION
As the fibrofatty tissue is elevated medially toward the carotid sheath, it will be necessary to incise the mastoid attachment of the sternocleidomastoid muscle and the clavicular attachments (see Fig. 121-5D). The carotid sheath will be exposed, and identification of the common carotid artery and vagus nerve may be made. Attention should be given to preserving the cervical sympathetic chain, which is closely applied to the prevertebral fascia behind the carotid sheath. The plane of dissection will be carried between the vagus nerve and the carotid artery below and the internal jugular vein above. Thus the internal jugular vein may be mobilized from the skull base superiorly to its inferior aspect near the clavicle; ties may then be placed around the upper and lower ends of the internal jugular vein, thereby allowing ligation and complete mobilization. When incising the soft tissue contents of the lower medial aspect of the neck, lymphatic channels will be encountered, particularly on the left side. It is imperative to precisely identify these and ligate them immediately as they are encountered. The thoracic duct is located to the right of and behind the left common carotid artery and the vagus nerve. From here, it arches upward, forward, and laterally, passing behind the internal jugular vein and in front of the anterior scalene muscle and the phrenic nerve; it then opens into the internal jugular vein, subclavian vein, or angle formed by the junction of these two vessels. The duct is anterior to the thyrocervical trunk and the transverse cervical artery. To prevent a chyle leak, the surgeon should also remember that the thoracic duct may be multiple in its upper end and that, at the base of the neck, it usually receives the jugular trunk, a subclavian trunk, and maybe other minor lymphatic trunks that should be individually divided and ligated or clipped.
At this point, the posterior belly of the digastric muscle is identified, and the soft tissue attachments of the neck contents lying superior to the muscle are divided, including the sternocleidomastoid muscle as it attaches to the mastoid process, vascular channels extending into the postauricular region and parotid gland, the tail of the parotid gland that extends downward inferior to the level of the digastric muscle, and soft tissue attachments to the angle of the mandible. After completion of this part of the dissection, all of the lower contents of the neck dissection specimen should be freely mobile, and the only remaining attachments are the upper end of the internal jugular vein and the undissected contents of the submandibular triangle and the submental triangle (see Fig. 121-5E).
Modified Radical Neck Dissection
DEFINITION
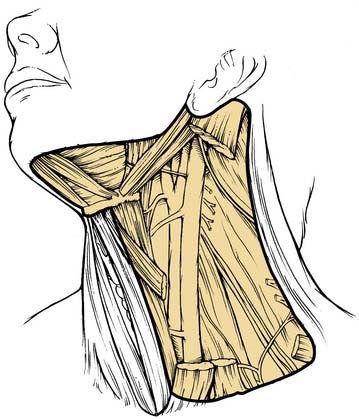
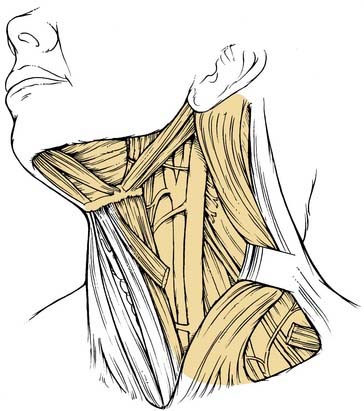
A modified radical neck dissection is defined as the en bloc removal of lymph node–bearing tissue from one side of the neck (levels I to V). The dissection extends from the inferior border of the mandible above to the clavicle below and from the lateral border of the strap muscles medially to the anterior border of the trapezius muscle laterally. Unlike the radical neck dissection, there is preservation of one or more of the following structures in the modified radical dissection: spinal accessory nerve, internal jugular vein, and sternocleidomastoid muscle (Fig. 121-6). The major purpose of these modifications relates to the morbidity encountered when the spinal accessory nerve is removed. Although the degree of morbidity is less for removal of the sternocleidomastoid muscle and the internal jugular vein, this issue becomes far more important if bilateral neck dissections are required. Simultaneous sacrifice of both internal jugular veins may result in severe swelling of the face with increased intracranial pressure.
TECHNIQUE
Unlike what is found in the radical neck dissection procedure, the next step is to identify the spinal accessory nerve. This is initially done in the posterior triangle from which the nerve exits at or around Erb’s point (Fig. 121-7A). The nerve lies superficially in the fibrofatty contents of the posterior triangle and usually may be identified by careful spreading of the fibrofatty tissue; the use of a nerve stimulator may assist this process. Once located, the nerve is isolated and dissected away from the underlying fibrofatty contents from Erb’s point medially to the point at which it enters the anterior border of the trapezius muscle laterally (see Fig. 121-7B). The nerve is next isolated in its superior third, which is done by incising the anterior border of the sternocleidomastoid muscle from its attachment superiorly at the mastoid to its lowermost attachment at the sternal head. The sternocleidomastoid muscle is retracted laterally as the fibrofatty soft tissue contents anterior to this muscle are dissected away from it, and the many arcades of small blood vessels coursing between the muscle and the soft tissue are divided. This part of the procedure mobilizes the anterior aspect of the sternocleidomastoid muscle along its full extent. As the muscle is retracted laterally in its upper portion, the spinal accessory nerve is seen entering its deep surface (see Fig. 121-7C
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree