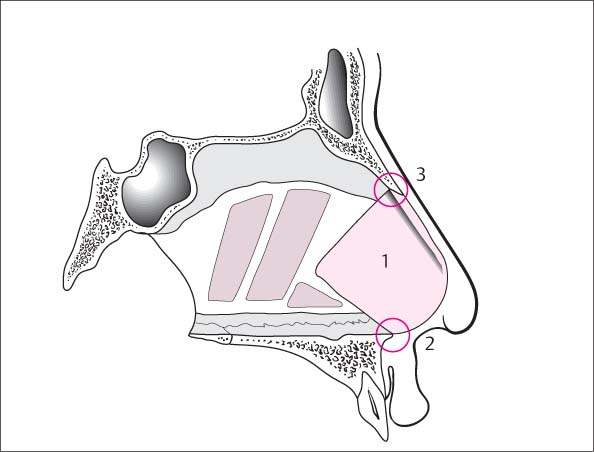
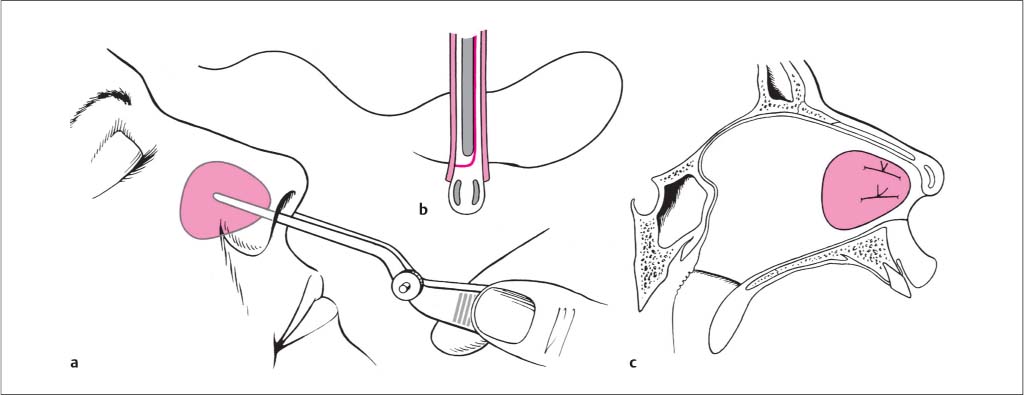
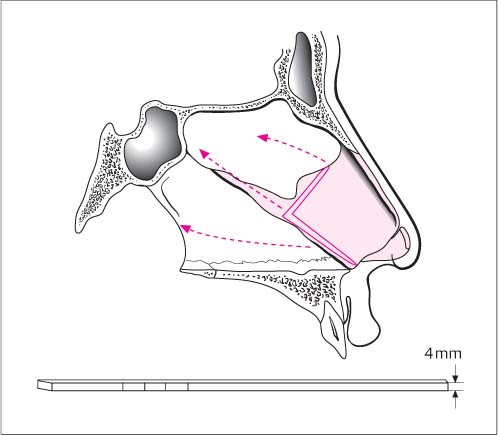
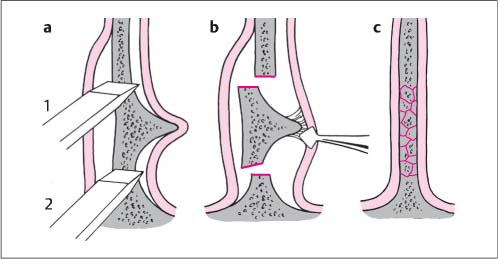
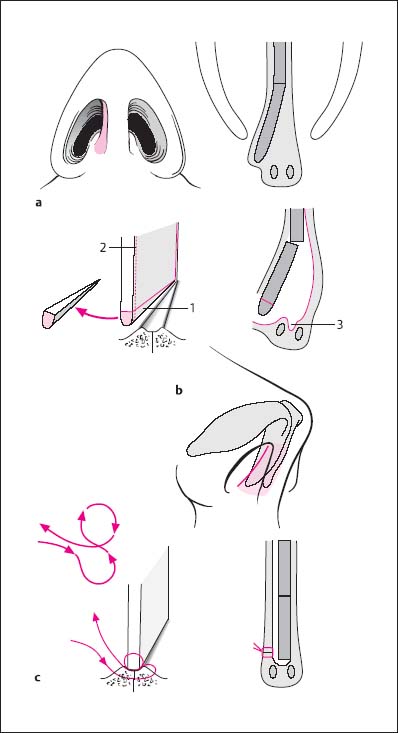
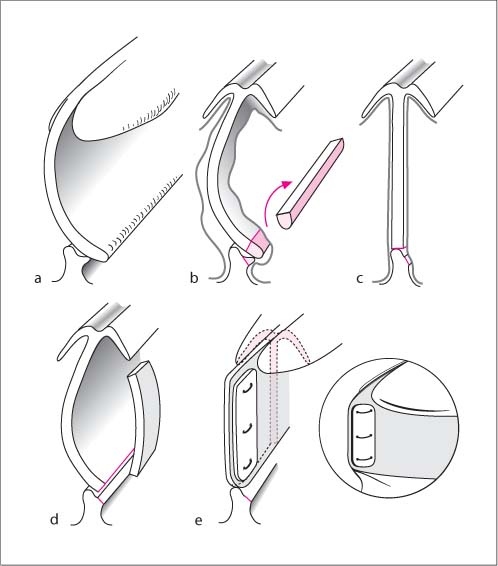
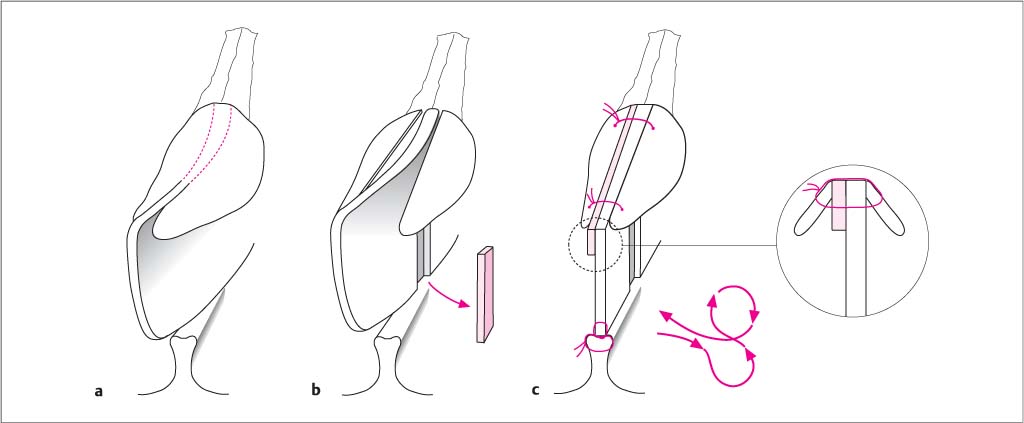
6 Nasal Surgery A basic distinction is made between the internal and the external nose. Common to both is the supporting structure of cartilage and bone, which is covered by skin (externally) and mucosa (internally). The supporting tissues are referred to as the bony and cartilaginous frameworks. The terminology for the position of individual parts is orientated according to the upright patient (Fig. 6.1), which requires a certain amount of thought during surgery. A flat muscle layer is embedded in the subcutaneous layer (s ubcutaneous m usculo a poneurotic s ystem = SMAS) which, together with the muscles of the nose, allows limited movements of the cartilaginous nasal segments as well as regulation of the width of the vestibule (see Fig. 6.31b). These muscles are largely spared during surgery if the soft tissues are elevated directly off the perichondrium of the upper lateral cartilages (degloving of the dorsum of the nose). On the inside of the nose, the lumen is adjusted by the erectile tissue of the mucosa. This tissue is found not only in the region of the nasal turbinates (particularly the inferior turbinate), but also in the middle part of the nasal septum (the so-called septal turbinate or intumescentia septi). The nasal frameworks are shown in detail in Figs. 6.1 and 6.2 and some special aspects are also mentioned here for a better understanding of operative techniques. The basic structure of the framework consists of the bony nasal pyramid (nasal bones and the frontal process of the maxilla), into which is inserted a cartilaginous pyramid made up of the nasal septum (cartilaginous septum, quadrilateral cartilage) and the upper lateral cartilages (triangular cartilages). The upper lateral cartilages and the septal cartilage form a single cartilaginous unit (the septodorsal cartilage) and are therefore not joined by cartilaginous sutures (Figs. 6.1c and 6.2b). Their positional relationship to each other is determined by internal cartilaginous forces, which may be disrupted by cartilage-splitting incisions, e. g., between the upper lateral cartilages and the septal cartilage (“division of the upper lateral cartilages”). The cartilaginous and bony frameworks are held together at three surgically relevant sites. First, the nasal bones overlap the upper lateral cartilages by a few millimeters. The integrity of this unit, consisting of nasal bones and upper lateral cartilages (Cottle’s “keystone” or K-area, Fig. 6.1d [3]), is particularly important for correction of the deviated nose, and it is separated when reducing a prominent nasal hump, for example. A further junction is the suture line between the perpendicular plate of the ethmoid and the cartilaginous septum (chondroethmoid suture), which is embedded with a sphenoid process between this suture line and the vomer (Fig. 6.2b [4]). A so-called “ascending septal ridge” can form at this interface. During septoplasty, e. g., for resection of this type of ridge, this attachment is separated by means of a complete vertical chondrotomy. The third anchorage point involves the septal cartilage and the premaxilla. The premaxilla is a distinct and separate bone (the os incisivum) which is inserted anterior to and between the maxillary bones (Fig. 6.2a [9]). Within the groove of the nasal floor, bordered on either side by bony extensions (premaxillary wings) and anteriorly by the anterior nasal spine, the septal cartilage rests in a fibrous sling that allows slight articulated movements. The premaxillary wings can appear asymmetrical and laterally protruding, thus causing septal deviations in the vestibular area, which can have an effect on breathing (the so-called basal crest). A horizontal chondrotomy during septoplasty will free this connection. At least two of the above-mentioned connections are essential to ensure sufficient stability of the cartilaginous pyramid and must either be preserved intraoperatively or reconstructed. Fig. 6.1a–d Infrastructure of the nose. a Architecture of the cartilaginous and bony pyramids. b Frontal section through the bony dorsum of the nose (“bony vault”). c Frontal section through the cartilaginous dorsum of the nose (“pointed arch”). d Sagittal section through the keystone area (“K-area”). 1 root of the nose (nasion, intersection between the internasal suture line and the nasofrontal suture line) 2 nasal bone 3 keystone area (“K-area”) 4 upper lateral cartilage (triangular cartilage) 5 septum (anterior–inferior corner), not covered by upper lateral cartilages (Converse’s weak triangle) 6 lower lateral cartilage: lateral crus 7 lower lateral cartilage: medial crus 8 maxilla: frontal process 9 frontal bone: nasal spine (together with the nasal bones, forms a solid bony block at the root of the nose) The nasal base is made up of the nasal tip, columella, and nasal alae. Its foundation is the paired lower lateral cartilages (Fig. 6.2c), which consist of a medial and lateral crus. The middle part diverges and is known as the intermediate crus. The degree of divergence determines, among other things, the width of the nasal tip. The nasal base is highly mobile with respect to the adjacent structures. The medial crus forms the cartilaginous base of the membranous septum, which can be moved in all directions against the relatively static caudal septal margin. The crura of the lower lateral cartilages are hinged to the adjacent upper lateral cartilages (Fig. 6.3), whose caudal margin is often curled outward for better stability (“returning” or “scrolling” of the upper lateral cartilages). The following details of the bony pyramid are of particular interest from a surgical point of view. A strong crest is relevant during osteotomies at the level of the nasal radix (lacrimal crest), behind which the lacrimal sac is found and into which the medial canthal tendon inserts. It is at this level that lateral osteotomies usually end, with the thickness of the bone protecting the canthal tendon and lacrimal sac from injury. The nasal radix, or root of the nose, also lies at the level of the me-dial canthus and defines the level of transverse osteotomies. In complete mobilization of the nasal radix, which is necessary for a markedly crooked nose, a solid block of bone, made up of the nasal spine of the frontal bone and the overlying nasal bones, needs to be divided (Fig. 6.1d). This osteotomy line usually lies caudal to the nasofrontal suture line. The internal nose starts with the vestibule (Fig. 6.3). This is defined anteriorly by the margin of the nostril and posteriorly by the nasal valve region. The vestibule consists medially of the membranous septum and laterally of the nasal alae, which are stabilized to only a small extent by the crura of the lower lateral cartilages. Large areas, reaching as far back as the bony piriform aperture, are free of cartilage and thus relatively unstable (see Correction of Alar Collapse, Fig. 6.62). The narrowest point of the nasal passage is the valve region (internal valves) at the junction of the vestibule and the nasal cavity. It includes the nasal valve proper, which is the space between the most caudal margin of the upper lateral cartilage laterally and the nasal septum medially. The width of this space, characterized by the nasal valve angle, which under normal circumstances is about 15°, is variable and depends on the activity of the nasal muscles—hence the use of the dynamic term “valve.” The head of the lower turbinate is also situated at the level of the nasal valve and contributes to regulating its width. Given the narrowness of this cross-section (Fig. 6.3a), even small irregularities of the nasal septum can result in considerable obstruction of nasal breathing (nasal valve stenosis—not to be confused with vestibular stenosis). Certain malformations of the external nose are typically associated with narrowing (tension nose, Fig. 6.3d) or pathological dilation (saddle-nose deformity, Fig. 6.3e). Cephalad to the nasal valve region the nasal cavity widens, with the cartilaginous roof appearing pointed and the bony roof taking on a vaultlike form (Fig. 6.1b, c). Fig. 6.2a–c The three basic units of the infrastructure. a Bony pyramid. 1 nasal bone 2 frontal bone 3 maxilla: frontal process 4 perpendicular plate 5 vomer 6 premaxilla: body and wing 7 incisive canal: nasal foramen 8 maxilla: palatine process 9 premaxilla: anterior nasal spine 10 piriform crest b Septodorsal cartilage. The septodorsal cartilage “inserts” into the bony pyramid. 1 upper lateral cartilage 2 “returning”: the caudal border of the upper lateral cartilage scrolls upward 3 septal cartilage: quadrilateral plate 4 septal cartilage: sphenoid process c Lower lateral cartilage. 1 medial crus 2 intermediate crus 3 lateral crus 4 dome Fig. 6.3a–e Nasal vestibule and nasal valve. a Structure of the nasal vestibule. 1 septal cartilage: caudal margin 2 lower lateral cartilage: lateral crus 3 upper lateral cartilage: caudal margin (returning) 4 lower lateral cartilage: protrusion of the lateral crus 5 inferior turbinate: head 6 nasal valve: angle between the upper lateral and the septal cartilage Enlarged inset (scroll area): 7 “cul-de-sac” between the caudal margin of the upper lateral cartilage and the undersurface of the lower lateral cartilage 8 transition between skin and mucosa (dark area) b Plane of section of c–e. c Normal nasal valve angle (ca. 15°). d Tension nose: excess growth of the septum produces a high nasal dorsum with reduction of the nasal valve angle and functional valve stenosis. e Saddle nose: depressed nasal dorsum with a wide nasal valve angle (“ballooning phenomenon”). The nasal septum divides the nasal cavity into two parts. It consists of the septal cartilage (quadrangular cartilage), which is in fact a “septodorsal cartilage,” and two bony parts (see also Fig. 6.15). The perpendicular plate of the ethmoid bone is a thin bony lamella; only at its junction with the septal cartilage is it thick enough to contain marrow. Any division made in this region should be done with an instrument and not by fracturing, which could result in dislocation of the adjacent cribriform plate of the skull base. The vomer, in contrast, is a very thick bone, which rises steeply up to the anterior wall of the sphenoid sinus. To mobilize it, the vomer should always be osteotomized or divided with nasal bone scissors. Small parts of the maxillary bone and palatine bone form the basis on which the vomer rests (Fig. 6.2a). The septal mucosa is firmly attached to the suture lines between the cartilaginous and bony parts of the septum, where it must be detached by sharp dissection. The attachment between premaxilla and septal cartilage in the region of the anterior nasal spine and the premaxillary wings is particularly strong. The vascular supply of the anterior parts of the nose originates from the internal carotid artery (ophthalmic artery → anterior ethmoid artery), that of the posterior parts from the external carotid artery (maxillary artery → sphenopalatine artery) (Fig. 6.4). Tributaries from both systems unite in the caudal septal mucosa (Kiesselbach’s plexus), which is a favored site for anterior nose bleeds. More serious nasal hemorrhage from the posterior nasal parts usually originates from the spheno-palatine artery, near its exit from the sphenopalatine (pterygopalatine) foramen. The course of the sensate nasopalatine nerve (incisive nerve) is important during septoplasty. After exiting from the sphenopalatine foramen, the nerve takes an anterior course in the septal mucosa and exits on either side through foramina in the nasal floor, ca. 1.5 cm dorsal to the piriform crest (lower osseous margin of the piriform aperture), in two bony canals toward the palatine side, which then unite to form the incisive canal. There the nerves innervate the mucosa behind the incisor teeth. When the septal mucosa is dissected in the vertical plane, the nerve can normally be protected. If the floor of the nose is also tunnelled, however, and septal tunnel and nasal floor tunnel are connected in the anterior part (the so-called maxillary–premaxillary approach; see Septoplasty, p. 57), then the nerve needs to be divided at its entrance into the bony canal. Without this division, connection of the vertical septal tunnel with the horizontal nasal floor tunnel will not be achieved. This may result in sensory disturbances of the mucosa behind the incisor teeth, which patients often perceive as “blisters.” Usually, however, this type of sensory disturbance is no longer noticed after a few weeks. The most important functions of the nasal airways are conditioning of the inspired air (humidification, warming, filtration) and olfaction. The most important organ for this processing of inspired air is the respiratory mucosa. The nasal turbinates provide a large contact area between inspired air and mucosa, and control the width of the airways by their erectile tissue. Larger particles (>10 μm diameter) are retained in the nasal mucosa; within a few minutes they are conveyed by mucociliary transport into the nasopharynx, from where they are swallowed. Humidification is accomplished by mucosal glands, which are primarily concentrated in the region between the internal valves and the heads of the turbinates. It is mainly there that the inspired air is humidified, although moisture is also regained during expiration. Conditioning of inspired air and olfaction are closely associated with the structure of the nasal airways. Essentially, three segments can be distinguished (Fig. 6.5). The air flows from below into the nasal vestibule and is greatly accelerated through the bottleneck of the nasal valve area. This creates a negative pressure during inspiration, which can subsequently lead to “alar collapse” in the presence of insufficient stability or malformation of the nasal alae. The nasal airways widen considerably behind the nasal valve and the airflow now adopts a more horizontal course. During inspiration, the nasal valve acts like a nozzle (diffuser) ensuring that the air is distributed throughout all parts of the nasal cavity and thus comes into close contact with the mucosa. The inspiratory resistance created by the nasal valve is therefore an important physiological prerequisite for the conditioning of the inspired air. Surgical widening of the nasal valve to make it wider than normal does indeed lower airway resistance, but at the expense of warming and humidification, which can lead to desiccation of the mucous membranes not only of the nose and pharynx, but also of the larynx and trachea. Long-term effects on the bronchial system can be expected. In the region of the turbinates and the nasopharynx the air flow is accelerated and once again diverted by 90°. On its way from the nasal vestibule to the pharynx the air thus follows a semicircular path, turning through 180° (Fig. 6.5). Fig. 6.4a–c Nerves and vessels of the nasal septum and the premaxilla. Arteries red, nerves black. a Sagittal section through the septum. b Sagittal section through the premaxilla (dotted line: plane of section of c). c Frontal section through the premaxilla. 1 external carotid artery 2 maxillary artery 3 sphenopalatine foramen, sphenopalatine artery and nasopalatine nerve 4 posterior ethmoid artery 5 anterior ethmoid artery and nerve 6 Little area (Kiesselbach’s plexus) 7 dorsal nasal artery 8 nasopalatine artery and nerve 9 descending palatine artery (light red) 10 external nasal artery 11 premaxilla with anterior nasal spine 12 premaxillary wing 13 maxillary bone: palatine process 14 incisive canal 15 incisive papilla 16 septal cartilage 17 vomer Fig. 6.5 Functional sections of the nasal cavity. A Nasal vestibule: inflow section with “diffusor” (nasal valve) B Turbinate area: air conditioning area C Main nasal cavity: air conditioning area D Choana: outflow section with “manifold” (nasopharynx) 1 Internal nasal valve area 2 Upper lateral cartilage 3 Head of inferior turbinate During expiration the air contacts particularly the cranial parts of the nasal cavity, where the olfactory mucosa is found, both on the septum as well as on the medial surfaces of the middle and superior turbinates. In this way, odors pass from the oral cavity to the olfactory organ (“gustatory olfaction”). Small drops of water are deposited in the region of the head of the turbinates and are then available again to humidify the inspiratory air. The oxygen-deficient air is accelerated in the nasal valve area and so transported away from the nasal vestibule. This prevents the “used” air from being drawn in again with the next intake of breath. For these physiological reasons, two basic principles may be deduced, which are important for the functional surgery of the nose: There are no routine procedures available to measure the conditioning of inspired air—warming, humidification, and particle filtration. (Active, anterior) rhinomanometry is an established procedure for measuring the respiratory function of the nose, which is merely the prerequisite for these basic functions. It quantifies nasal airway patency. On one side of the nose respiratory volume is measured during inspiration and expiration, and on the other side the pressure difference required to move the air between the atmosphere and the pharyngeal cavity is measured. The values are valid only with an intact nasal septum; in the presence of a septal perforation they are distorted. Generally speaking, in addition to recording the values on a chart, volume flow as a measure of nasal breathing is given at a fixed pressure difference of 150 Pa. It is subject to considerable variation, but values between 300 and 500 mL/s are generally considered normal. In the presence of an obstruction to nasal breathing, a comparison of the measured values before and after decongestion of the nasal mucosa can provide information as to whether the problem is structural (e. g., septal deviation), mucosal (turbinate hypertrophy), or a combination of the two. As a rule, rhinomanometry can only provide an overall statement about the function of one side of the nose, not a more exact spatial indication of the location of a functional impairment. A more detailed assessment of the shape of the graph makes this possible to some extent, but is only rarely undertaken in practice. The results obtained by measuring pressure gradient and volumes are very variable, so they are usually only regarded as supplementary to the information already found by inspection. Rhinomanometry is nevertheless recommended before operations on the internal and external nose, to provide pre- and postoperative comparison. Using the echo sonographic technique, acoustic rhinometry measures the cross-section of the nasal cavity in relation to the distance from the nasal vestibule. It is a static procedure, which allows only conditional conclusions to be drawn on dynamic inspiration and expiration. The precision of the cross-section measurement decreases with the distance from the nasal vestibule, and assessment of nasal vestibule and nasal valve area is significantly limited by the need for a tight-fitting nasal adapter. Olfaction should be determined preoperatively with the aid of a screening test (subjective, various odor qualities), mainly for medicolegal reasons. Disturbances of smell may well arise after surgery, e. g., as a result of scar formation or of infection or toxicity, but they may have been already present before surgery. Although they are only noticed later by the patient. A multitude of instruments are available for septoplasty and rhinoplasty and are often offered in different variations, depending on individual experience. The selection shown in Fig. 6.6 has been chosen largely on the basic principle that it is not necessary to have a special instrument for each and every operative step. On the contrary, as few instruments as possible should be used for as many functions as possible. Novices in functional and aesthetic surgery of the nose can familiarize themselves with the instruments presented here and, as they gain experience, may decide to dispense with some instruments or replace them with variations more suitable to their needs. Fig. 6.6a, b Instruments (selection). a Septoplasty b Rhinoplasty The double elevator has a blunt and a sharp end. The blunt end is for subperichondrial dissection of septal mucosa (“over cartilage”), the sharp end for subperiosteal dissection (“over bone”). With more significant hemorrhage and subsequently unclear conditions, the suction elevator may also be used, with the suction opening pointing to the cartilage or bone. The Cottle nasal knife is used to divide cartilage (chondrotomy), as well as for detaching fibrous strands, particularly in the area around the premaxilla. This bone contact soon makes the knife blunt, and it should be sharpened before any subsequent work on cartilage. The McKenty curved elevator is used to create the inferior septal tunnel and should be only slightly bent to avoid placing the septal mucosa under too much tension. It is important to distinguish between a chisel and an osteotome. The chisel has an oblique cutting surface, which allows the instrument to be driven into the bone away from the cutting surface (see arrows in Fig. 6.6). This is particularly required when there is a need to progress from thin bone into more solid bone. An osteotome, with two cutting surfaces, usually glides straight ahead and would at this point tend to glide away from the more solid bone. In septum surgery, therefore, a chisel is more helpful when making an osteotomy of the vomer near the more solid bone of the nasal floor. An all-round forceps for septum surgery is the Adson–Brown forceps (or “plastic surgery forceps”), which has a row of teeth on either side of the forceps jaw (in this way acting like a multiple surgical forceps), allowing a gentle but stable grasp of soft tissues or cartilage. Good visualization is essential for work on the nasal dorsum. So-called “Aufricht retractors” (named after an American rhinosurgeon) should therefore be wide enough. Sharp double-pronged retractors for incisions and dissections in the nasal vestibule can be comfortably held with the aid of a thumb ring, freeing the surgeon’s fingers for use as a counter-support. Osteotomes for nasal hump reduction should be as wide as possible, so that the bony part of the hump can be mobilized in one piece and thus avoiding multiple attempts, with the subsequent risk of producing unequal cutting levels. The corners of the blade should be rounded, to avoid inadvertently perforating the skin as it is elevated by the osteotome. It should be possible to hold the osteotome horizontally steady so it does not tilt laterally during osteotomy. This requires a stable handle. Lateral and transverse osteotomies can be performed with either narrow chisels or osteotomes (e. g., 3 mm) directly through the skin via stab incisions; the usual practice, however, is via the nasal vestibule. The so-called “guarded osteotome” is effective for lateral osteotomies, especially for thicker bone, as it can be easily hooked into the piriform aperture while allowing stable guidance and control with the aid of the guard, which glides along the outside of the bony pyramid. Variously curved guarded osteotomes are available for left and right lateral osteotomies, although a straight osteotome is usually quite adequate. A transverse osteotomy can also be performed via the nasal vestibule with a chisel that is curved at the end (“transverse chisel”). If the cartilaginous nasal septum is “too high” at the nasal dorsum after hump reduction, it may be successively reduced to the correct level under direct vision using scissors with angled blades. Small teeth on the serrated cutting surfaces prevent the mobile cartilage from evading the scissors. If smaller irregularities still remain over the nasal dorsum after hump reduction, they may be smoothed down with a rasp or file. The difference between the two instruments lies in the fact that files remove bone during both the forward and the backward movement, while rasps normally only remove bone with the backward movement. Because files only remove a small amount of bone with each movement, it is usually recommended to use a rasp as the main instrument for smoothing out irregularities. When using these instruments, it should be borne in mind that both types can work only on bone and not cartilage. Sharp ridges are often found at the transition between cartilaginous and bony dorsum, due to bulges of the upper lateral cartilages, and these can only be removed with the aid of a scalpel. Depending on the frequency of their use, sharp instruments become blunt. They must therefore be sharpened regularly (scissors, chisel, osteotome) or exchanged (rasp). It is the sharpness of the osteotome in particular that determines the quality of osteotomies. With a sharpening stone available on the instrument table, osteotomes can be sharpened by the surgeon immediately before use. Soft-tissue injuries must be managed using atraumatic technique. With multilayered injuries, management proceeds from the inside out, especially with perforating injuries. With avulsions (e. g., secondary to dog bites) replantation has a prospect of success only with superficial injuries. Gaping cutaneous wounds, perforations, defects. The patient needs to be informed about tissue transplantation, the possibility of staged procedures, later fine adjustments, and potential functional and aesthetic impairment, especially with regard to more complex procedures to manage defects. Treatment should be initiated as soon as possible. Immediate reconstruction is preferable for defects, because healing by secondary intention makes later reconstruction more difficult due to extensive scar areas and distortions. With disrupted tissues, even small viable skin bridges are often enough to ensure adequate perfusion of injured areas. They should be carefully preserved. Atraumatic needle–suture combinations are required to achieve good aesthetic results on the face. Monofilament sutures should be used for repair of the skin. Lacerations can be adequately treated with tissue glue instead of sutures, especially in children. Occlusive dressings promote wound healing, especially with abrasions. General anesthesia may be required, depending on the scale of the injury and time needed for repair. In principle, however, the use of a local anesthetic is possible by infiltrating the injured area in a fan-shaped pattern. Perforating injuries are closed in layers from the inside out (Fig. 6.7). Wound edges should be slightly everted to avoid the subsequent formation of retracted scars. Longer linear scars running perpendicular to the RSTL are converted into zigzag lines by creating small Z-plasties (W-plasty), which then come to lie partially in the RSTL and are thus cosmetically less conspicuous (see Chapter 5). In the nasal vestibule, semicircular shear injuries can occur at the piriform aperture, with involvement of the head of the turbinate. In these cases, the wound margins should be exactly re-approximated to preclude the development of a scar contracture with a pinhole stenosis of the vestibule. Fig. 6.7 Full-thickness laceration of the complete ala. Closure in layers from the inside out: suture repair of 1 vestibular skin and mucosa 2 cartilage 3 external skin Avulsions can arise after dog bites, for example; often the victims are children. The missing piece of tissue is often lost or rendered unusable for replantation by severe crushing. A full-thickness skin graft is an option for defects involving only skin. The retroauricular skin is a suitable donor site. With chondrocutaneous defects of up to 1 cm in size, a free chondrocutaneous graft from the auricle is an option (see Chapter 5). Free grafts should be immobilized for 10 days by an external dressing and possibly supported from within the nose by suitable packing. Antibiotic cover is recommended, particularly when nasal packs are used. If the skin has been soiled by ingrained dirt (a so-called “dirt tattoo”) during an accidental injury (e. g., a cycling accident), then the particles must be scrubbed out intraoperatively with a sterile hand-washing brush. This is best done during the initial treatment; later attempts at cleaning the skin are usually much less effective. If, despite all due care and attention, unfavorable scar formation or even the distortion of adjacent structures due to the scars has occurred, then at least 6 months should elapse before revision surgery is attempted. Only then will sufficiently stable scar conditions have developed. Foreign bodies of every description are inserted into the nose, especially by small children, but also by psychotic patients. Unilateral, intractable purulent discharge from the nose should always prompt the search for a foreign body. A round foreign body is removed by placing the end of a right-angle hook behind the object and pulling it forward (Fig. 6.8). Foreign bodies which have remained in the nasal cavity for a longer period of time can become encrusted and form a so-called rhinolith (preferentially in the inferior nasal meatus). Usually this can only be extracted after mobilization with a chisel. Typical fracture patterns occur, depending on the direction and strength of the force applied (Fig. 6.9): – moderate force: lateral depression without involvement of the septum – severe force: bony, crooked nose with associated septal fracture. – moderate force: dorsal nasal depression (saddle-nose deformity) – severe force: saddle-nose deformity with impacted fracture of the nasal septum. The diagnostic examination includes inspection and palpation, ensuring that the nasal septum is examined for septal hematoma or septal fracture. With major trauma, associated injuries of adjacent organs should also be assessed (anterior skull base, frontal sinus, orbital walls, zygoma, maxilla). Imaging is particularly appropriate in these cases (CT for major injury). Assessment of slight displacements of the nasal pyramid may be rendered difficult by soft-tissue swelling. In such cases it is advisable to repeat the examination a few days later, after the edema has resolved. Fresh fractures should be treated within 8 days of the injury. Fig. 6.8 Removal of a round foreign body from the nasal cavity. The blunt 90° hook is placed behind the foreign body. Fig. 6.9a–d Fractures of the nasal pyramid: injury mechanisms. a Lateral impact injury (moderate force): lateral impression without lateral displacement of the pyramid; septum intact → endonasal reduction. b Lateral impact injury (severe force): crooked nose with fracture of the septum → endonasal and external reduction of septum and pyramid; septoplasty may be necessary. c Frontal impact injury (moderate force): dorsal nasal depression (localized saddle-nose deformity) → endonasal reduction. d Frontal impact injury (severe force): saddle-nose deformity with impacted fracture of the septum → endonasal reduction and septoplasty. The management of fractures of the nasal septum should adhere to the principles of septoplasty (see below, p. 57 ff). Dislocated bony walls of the pyramid are reduced (Fig. 6.10). Here the following principles apply: Isolated depressions of the lateral nasal wall may give the misleading impression of a deviation of the nasal dorsum. Fresh fractures (up to 8 days old) associated with cosmetically and/or functionally relevant sequelae. Septal fractures with mucosal injury or septal hematomas require immediate treatment, otherwise a wait of up to 8 days is possible (edema reduction). Fractures older than 2–3 weeks. In this case it is better to wait 6–12 months and then correct the pyramid by means of a rhinoplasty after performing osteotomies. Fresh injuries may be superimposed on old fractures, rendering reduction impossible. The patient should therefore always be asked whether the nose was already “crooked” before the presenting injury. In a fresh lateral impact injury, deviation of the nasal dorsum without significant depression can be manually reduced to the midline without anesthetic. Depressions secondary to a lateral or frontal impact injury are best reduced from an endonasal approach under general anesthesia. For endonasal reduction, a blunt instrument is introduced (e. g., the blunt end of a Cottle elevator), either to lift the nasal dorsum or to displace the lateral nasal wall outward (Fig. 6.10). If the cartilage fragments do not interlock by themselves, then they will need endonasal support in the form of packing for 8–10 days. In these cases, antibiotic prophylaxis is recommended. If the cartilage fragments have interlocked in the wrong position and disimpaction is difficult, they will need instrumental mobilization first. This is best achieved with a disimpaction forceps, which is introduced with one of its jaws into the nose to mobilize the lateral nasal pyramid wall with slight rotary movements. After reduction an external splint is required, not so much for stabilization as for protection and to avoid any significant postoperative swelling. It is applied in the same manner as for elective septo-rhinoplasty (Fig. 6.11). The nasal dorsum is covered with a dressing consisting of overlapping strips of adhesive tape. The tissue in the supratip region has a tendency to swell considerably, and a swelling with the subsequent formation of a “polly beak” deformity (see Fig. 6.42) may develop if a hematoma appears. To counteract the development of swelling there, a strip of tape should be applied firmly over the supratip. The actual splinting can be achieved with a thermoplastic splint, or with plaster of Paris or other material. Care should be taken to ensure that no sharp edges penetrate the skin of the medial canthal region and that the eyelids can open and close without hindrance. A grid-patterned splint has the advantage that the vertical components of the grid are helpful for orientation and assist in bringing the nasal dorsum back into its midline position. The splint is secured with further strips of tape, similar to those laid on initially. Fig. 6.10a–c Nasal pyramid reduction and septal revision. a Frontal impact injury with fractures of the pyramid and septum. b Reduction of the nasal dorsum using an elevator after management of the septal fracture. c Appearance after reduction and fixation of the septum with septal splints. Septal fractures that affect breathing require mobilization and correction of the nasal septum, in addition to reduction of the external bony pyramid (Fig. 6.10). The technique does not in principle differ from that used for septoplasty (see below, p. 57 ff). Bleeding occurs if the perichondrium is stripped from the underlying cartilage, resulting in the formation of a septal hematoma (Fig. 6.10a). Without treatment, the hematoma leads within a few days to absorption of the cartilage, which is dependent upon the perichondrium for its blood supply by diffusion. The result is the complete loss of the supporting function of the cartilaginous septum, with the development of a cartilaginous saddle-nose deformity. A septal hematoma can also develop relatively quickly into a septal abscess, which then leads to the destruction of the cartilage within a matter of hours. Apart from fever caused by infection, the presenting signs are complete blockage of nasal breathing with erythema and swelling of the skin in the region of the dorsum, columella, and nasal tip. Even light pressure on the nasal tip is painful. Such septal hematomas and abscesses can also develop after minor injuries (particularly in children), or even without any apparent external cause. The results of culture swabs taken from abscess fluid often return as sterile; occasionally staphylococcus or streptococcus is isolated. Antibiotic treatment is indicated in addition to surgery. After incision and drainage of the hematoma or abscess, any cartilage necrosis will require debridement and immediate reconstruction. Prevention of recurrence is essential, e. g., by the use of septal splints. Children can still develop disturbances of growth in the course of time, despite appropriate management (see Fig. 6.28). Parents should be informed that definitive surgical treatment of residual deformities may possibly still be required after growth is complete. In cases requiring immediate reconstruction of the nasal septum, mention should be made of the possible need to harvest cartilage from the auricle or the use of foreign cartilage. After incision and drainage of the hematoma and abscess, intraseptal granulations should be curetted and the operative site irrigated with an antibiotic solution. Fig. 6.11a, b Nasal dressing and splinting. a Nasal dressing consisting of overlapping strips of adhesive tape. A “suspension” around the tip of the nose takes the tension off the endonasal sutures. Swelling of the supratip region must be avoided by firmly applying a strip of tape (arrow). b Splinting and fixation: a splint constructed from grid-patterned thermoplastic material is trimmed to form so that the grid is orientated exactly vertically over the dorsum of the nose (1). This helps in bringing the mobile nasal dorsum exactly into its midline position. The splint must spare the medial canthal regions (2). General anesthesia is advisable. The region of the hematoma/abscess is exposed via a hemitransfixion incision (see Septoplasty, p. 57 ff) and a tunnel is developed beneath the mucosa until healthy cartilage or bone is reached. Soft, unstable nasal septal cartilage is removed and a culture swab of the abscess fluid is taken. After irrigating the cavity several times, the perichondrium and the periosteum are freed of granulations with a curette. These measures may need to include the undersurface of the upper lateral cartilages as well as the region around the membranous septum. After several rinses with an antibiotic solution, the perichondrial surfaces should be smooth on all sides. If the caudal septal cartilage has been destroyed, immediate reconstruction is advisable, even in the presence of a septal abscess, to prevent contraction of the soft tissues. Options for autologous supporting material include either bony parts of the vomer and perpendicular plate or autologous conchal cartilage from the auricle. If it is available, solvent-dehydrated irradiated human costal cartilage is very suitable and can be rehydrated in an antibiotic solution. Even if these grafts and implants only act as temporary spacers, they not only prevent soft-tissue contracture, but also considerably facilitate any later definitive treatment. Prophylaxis against renewed intraseptal fluid collection can be achieved either by trans-septal absorbable mattress sutures or by sutured-in septal splints (Fig. 6.10c; see also Fig. 6.18). Unlike sutures, intranasal septal splints have the advantage of providing compression over a larger surface area. They should remain in situ for approximately 1 week. The packs should remain for 3 days and the septal splints for up to 1 week under antibiotic protection. Otherwise postoperative care does not differ from that for septoplasty. Localized unilateral septal hematomas (but not abscesses) may also be aspirated with a needle and then packed. If they are not too large, they may be left for spontaneous absorption, given that any aspiration is associated with the possibility of bacterial spread and secondary infection. A unilateral hematoma does not carry the risk of cartilage necrosis because nutrition of the cartilage is guaranteed by the perichondrium of the contralateral side. Hematomas situated over bony regions of the septum are less at risk because the bone does not receive its nutrition by diffusion, but via blood vessels. The cartilaginous nasal septum is the central supporting structure for the cartilaginous nose and the enveloping soft tissues. Septal deviations have functional consequences especially in the areas of natural narrowings, i. e., the nasal vestibule and at the level of the nasal valve area. Deviations situated more posteriorly (e. g., vomerine spur) can also represent a breathing obstruction, although they tend to be less serious than anterior deformities. Deviations of the cartilaginous septum are therefore of particular functional importance and must be corrected by mobilization, reduction, resection, and, if necessary, reconstruction. Consideration must be given to the supporting function of the caudal nasal septum, which needs to be reconstructed by septoplasty or preserved during straightening procedures. As Fig. 6.12 clearly shows, it is not merely a problem involving the internal nose; loss of the supporting function of the nasal septum also has manifold consequences which also affect the external form of the nose. The left column in Fig. 6.12 shows the normal situation, with cross-sections parallel to the columella at the level of the lower lateral cartilages (1) and the nasal valve (2), as well as a cross-section through the columellar base and the alae of the nose (3). By comparison, the right column shows the effects resulting from destruction of the septal cartilage, with subsequent reduction in the height of the caudal septal margin. The lower lateral cartilage domes usually have an acute-angled form as seen from the basal view, with the fibrous tissue between the domes riding on the anterior septal margin, thus determining the height of the nasal tip (the nasal tip projection is the distance between the nasal tips as seen from the vertical facial plane—see Figs. 6.39 and 6.40). Cartilage and soft tissues are thus under tension. The nostrils are oval and the columellar base is only slightly wider, due to the diverging medial crura of the lower lateral cartilages. The intact septodorsal cartilage has a nasal valve angle of approximately 15°. In the transverse section through the columellar base, the latter lies caudal to the alar rims, the membranous septum is elongated and the cross-sections of the medial crura of the lower lateral cartilages are close together. This creates a space between the membranous septum and the alar rim, which is large enough to prevent the nostrils from being sucked in toward the membranous septum during inspiration. The alterations encountered when the septum height is reduced are correspondingly complex in nature. The nasal basal view now demonstrates a reduction in nasal tip projection. The fibrous tissue between the lower lateral cartilages is no longer held under tension by the nasal septum; the domes flatten off and diverge. The result is a wide nasal tip, which is amorphous or undefined because of the loss of the domes. The loss of height results in excessive soft tissue, which widens, so the distance between the two nostrils is greater and the normally oval nostrils adopt a more rounded form. Reduction of the cartilaginous nasal dorsum causes the nasal valve angle to increase up to 90° (a situation known as the “ballooning phenomenon”). This results in a deflection of the principle air flow toward the floor of the nose, which is associated with an overloading and desiccation of the mucous membranes. The transverse section through the columella now shows the columella to be lying at the same level as the alar rims (retracted or “hidden” columella) and at the same time widened as a result of the loss of tension (the cross-sections of the medial crura of the lower lateral cartilages are farther apart). The now reduced distance between nostrils and columella results in vestibular stenosis, with the risk of total collapse from negative pressure during inspiration. Fig. 6.12a–d The role of the nasal septum as the central supporting structure for the nasal tip, nasal dorsum, and nasal base. Left column: normal situation. Right column: sequelae after loss of the supporting function of the septal cartilage. a Lateral view indicating the section planes 1–3. b Section through the nasal tip (1): the domes are supported over the upper septal margin and held under tension by fibrous tissue. This gives the domes an acute angle, making the tip of the nose slender (left). Loss of height of the caudal edge of the septum “relaxes” the cartilage, making the domes and the tip as well as the nostrils “round.” Nasal tip projection is reduced and the columella becomes wide and short. The distance between the alae is increased (right). c The angle of the nasal valve is widened (ballooning phenomenon). d The columellar base is held in a caudal direction by the septum and placed under tension. This makes it narrow. The medial crurae of the lower lateral cartilages are close together and their distance from the nostrils is wide (double arrow left). If the caudal edge of the septum is displaced posteriorly, the columellar base retracts and becomes wider. The vestibule is then narrower (double arrow right). This list of the dynamic processes that result from the loss of the supporting function of the cartilaginous nasal septum shows that three aspects in particular must be borne in mind during surgery of the nasal septum: Fig. 6.13 The objectives of septoplasty/septal reconstruction. Preservation or reconstruction of the cartilaginous support by: 1 adequate size, form and stability 2 preservation or reconstruction of the connection with the premaxilla 3 adequate fixation by (partial) preservation of the suture line to the perpendicular plate or by suturing the upper lateral cartilages and septum at the level of the keystone area Surgery of the nasal septum usually involves mobilization of the cartilaginous septum. It is therefore essential to have knowledge of the natural fixation points, which need to be either preserved or reconstructed after separation (Fig. 6.13 [2, 3]): The literature often describes submucous resection of the septum (Killian) and septoplasty (Cottle) as if they were basically equivalent. These two operative techniques are, however, different in principle. During submucous resection of the septum the central cartilaginous and osseous components of the nasal septum are removed, while preserving a sufficiently large cartilaginous frame at the nasal dorsum and columella. If the stability of this frame becomes inadequate after extensive resection, a typical deformity will result, as shown in Fig. 6.12. Because it is important not to disrupt the unit of mucosa and cartilaginous frame, the incision through the mucosa to gain access to the area of resection lies immediately at the anterior border of the intended cartilaginous window. This approach therefore does not allow the exposure of deviations of the cartilaginous frame. Submucous resection of the septum thus corrects mainly septal ridges at the junction between septal cartilage, vomer, and perpendicular plate, or corrects a vomerine spur. It has already been pointed out that obstruction of nasal breathing due to this deformity is often only moderate. In contrast, the principle of septoplasty not only permits correction of the central parts of the septum, but also allows surgery of the cartilaginous framework. Cottle’s standardized approach (maxillary–premaxillary approach) enables the complete exposure of the infrastructure of the nasal septum. Because deviations of the cartilaginous framework lie at the narrow parts of the nasal airways, they are of considerably greater functional importance than deviations of the central septum. Although the procedure has undergone changes over the years, certain basic operative steps still apply: 2. Approach: subperichondrial and subperiosteal septal tunnels. 3. Mobilization (chondrotomies, osteotomies). 4. Resections (cartilage and/or bone). 5. Reconstruction/replacement. 6. Fixation (suture, septal splints). Only knowledge and use of an approach which provides access to all parts of the septum will allow its correction, and this is therefore recommended as the basic technique. Depending on the presenting pathology, an adapted modification is then possible. Cottle’s technique is to proceed along the floor of the nose from bilateral tunnels, which are developed beginning at the piriform aperture in a dorsal direction (maxillary approach). These nasal floor tunnels are connected to superior septal tunnels, proceeding from the caudal septum and the premaxilla (premaxillar approach). Connecting the septal tunnels to the nasal floor tunnels, however, necessitates division of the nasopalatine nerve at the incisive canal (Fig. 6.4), which is why the maxillar–premaxillar approach is mainly recommended only for special indications (protruding basal crest of the nasal septum, difficult revision surgery, closure of septal perforations). Otherwise, tunnelling of the septum should only be performed in a vertical plane, sparing the horizontal nasal floor. It is to be expected that any cartilage material still available from earlier injuries or operations will be insufficient to restore an adequate supporting function of the cartilaginous nose. The so-called “cotton bud test” can assist in providing an estimate: the nasal septum is palpated with a cotton bud to identify any areas that are still stable or free of cartilage. The possible harvesting of a graft should be provisionally included in the informed consent, to avoid resorting to compromises when faced with a lack of cartilage during the operation. In difficult cases, especially with re-explorations, it may be useful to include subsequent revision surgery to remove residual deformities in the operation plan. A selection of instruments for septoplasty is shown in Fig. 6.6a. Septoplasty is usually performed under general anesthesia. Only in selected cases of isolated operations in the vestibular area (e. g., isolated dislocation of the caudal septal margin—very rare) can local anesthesia be sufficient. The operation is divided into the following steps: – caudal septal margin (see Fig. 6.22). – superior septal margin (see Fig. 6.23). These measures, on the other hand, are usually performed in a uniform manner. Because of the mainly uniform approach, independent of the presenting pathology, points (a) and (d) will be discussed together (Figs. 6.14, 6.15, 6.16, 6.17, and 6.18). Preparation. The head is positioned slightly elevated (chin in the direction of the chest) to allow visualization of both the nasal floor and the superior parts of the septum, without the surgeon having to adopt extreme head positions. The operative site is prepared before sterile draping: decongestion of the mucous membranes (e. g., by inserting strips of sponge soaked in xylometazoline), possibly cleansing the nasal vestibule with alcohol (where staphylococci are found in about half of all patients), infiltration of the membranous septum (for practical reasons a ready-prepared combination of local anesthetic and epinephrine 1:200 000 has proved useful). Extensive infiltration of the septal mucosa to facilitate later tunnelling (so-called “hydraulic dissection”) is not generally recommended, as this usually inflates only the mucosa and does not separate the perichondrium from the cartilage, in addition to the complications that have been described (blinding). Disinfection of the face is an option, but not absolutely necessary. Antibiotic prophylaxis (e. g., for re-explorations using grafts, potentially infected adjacent regions) should be administered in the form of perioperative prophylaxis. A right-handed surgeon stands to the right of the patient. Incision: right hemitransfixion (Fig. 6.14). For the right-handed surgeon, the right nasal vestibule is more easily visualized than the left, which is why the incision is always performed on the right, even if the caudal septal margin is dislocated to the left. The caudal septal margin is exposed using a columella forceps and an alar retractor: the clamp grasps only the mobile membranous septum. The skin covering the cartilaginous margin is placed in tension by moving the clamp to the left and posteriorly. The alar retractor (assistant) exposes the attachment of the upper lateral cartilage and at the same time protects the ala from an inadvertent laceration. The middle finger of the surgeon’s right hand can displace to the right a septum which has dislocated to the left and stabilizes the septal cartilage for the incision. Fig. 6.14a, b Incision. a Right hemitransfixion. b Identification of the caudal septal margin and the subperichondrial plane of dissection (approach to the left anterior tunnel). Fig. 6.15 Position of the four septal tunnels (unilateral) over the: 1 quadrangular plate 2 perpendicular plate 3 vomer 4 vomer and premaxilla The hemitransfixion (Latin: hemi = half, transfigere = to pierce through) incision is made, using a No. 15 scalpel blade, in the skin (not in the mucosa) about 2 mm behind the cartilage edge, from the anterior nasal spine to just before the attachment of the upper lateral cartilage (the anterior–inferior septal corner). The incision proceeds in a posterior-to-anterior direction to avoid blood dripping down and obstructing the view. Incision of the cartilage should be avoided. Note: A transfixion (see Fig. 6.32a) differs from a hemitransfixion in that it not only transects the entire membranous septum through to the opposite side, but also lies caudal to the septal end. It enables the membranous septum to be completely separated from the nasal septum, together with the columella and the medial crura of the lower lateral cartilages. Approach: septal tunnels (Figs. 6.15 and 6.16). The cartilaginous framework is exposed by subperichondrial septal tunnels and the bony framework by subperiosteal septal tunnels. It is generally recommended, whenever possible, to leave the cartilage attached on one side to the septal mucosa, as this reduces the risk of a too generous mobilization and dislocation. With a unilateral anterior deviation, one would create an anterior tunnel only on that side. The left tunnel is routinely created first when dealing with an ascending septal ridge on the left side. Finding the correct plane for the dissection is essential. The fibrous strands are separated from the caudal septal margin with a pointed instrument (e. g., closed small pointed scissors, Fig. 6.14b). At times they will require transection. The correct plane can often only be identified 2–3 mm behind the cartilage edge. After elevating the perichondrium, the cartilage shines through with a bluish tinge. The “incorrect plane” is recognized by its reddish color and pinpoint bleeding. In this case, the remaining perichondrial layer must once again be separated from the cartilage with a pointed instrument. Once the subperichondrial layer has definitely been reached, tunnelling beneath the quadrangular plate to its junctions with the perpendicular plate (chondroethmoid suture) and the vomer (chondrovomerine suture) is usually achieved without difficulty using the blunt end of a Cottle elevator, provided no significant deviations are encountered which place the mucosa under tension, or old cartilage fractures to which the mucosa is attached by scar tissue. At these points, further sharp dissection must be undertaken. In this manner, a left anterosuperior tunnel is created. The mucosa is elevated off the junction with the perpendicular plate using the sharp end of the Cottle elevator and a posterosuperior tunnel is dissected, ensuring constant contact of the instrument with bone as far as the junction between the perpendicular plact and the vomer (or the sphenoid process of the septal cartilage). On completion of these steps, a left anterosuperior and a left posterosuperior septal tunnel will have been created. Fig. 6.16a–e Septoplasty: standard approach to the infrastructure. Presentation of the individual steps in the frontal, horizontal, and sagittal planes; the horizontal section plane is marked in each case in the right column. a Superior tunnel left anterior (1) and posterior (2). b Inferior tunnel left anterior (3) and posterior (4). c Horizontal chondrotomy at the cartilaginous base of the septum. d Vertical chondrotomy at the osseocartilaginous junction, sparing the region immediately below the nasal bones (x) and the right posterosuperior (5) and inferior (6) tunnels. e Anteroinferior tunnel on the right. The posteroinferior tunnel may be opened from above by sharp division of the fibers at the bony suture (the so-called “posterior approach”) to allow the anterior section to be exposed from here (7). The left inferior tunnels may be created relatively simply in a posterior-to-anterior direction via the superior tunnel, provided there is no relevant septal deviation. For this purpose, the mucosa is elevated in the posterior septal segment at the junction between perpendicular plate and vomer, using the sharp end of the elevator, and the tunnel is then exposed from above down to the nasal floor (the so-called posterior approach to the inferior tunnel). With contact between the instrument and the bone of the nasal floor, this posteroinferior tunnel may then be easily enlarged in a posterior-to-anterior direction as far as the level of the premaxillary wing and the anterior nasal spine. Dissecting in the vertical plane in this region avoids injuring the nasopalatine nerve. At the end of this stage, a complete left-sided tunnel of the nasal septum will have been developed (Fig. 6.16b). With a protruding ascending septal ridge or a basal crest, this posterior approach to the inferior tunnel is not possible. Instead, the mucosa must be elevated from the undersurface of the ridge or crest from an anterior direction. For this purpose, the strong fibrous strands are first separated from the bone at the piriform aperture, exposing the transition from premaxilla (septum) to nasal floor at the piriform crest. This then allows a curved elevator (e. g., a McKenty elevator) to be inserted, with bone contact, to separate the mucosa subperiosteally from the premaxillary wings and from the undersurface of an ascending septal ridge (Fig. 6.16b). In this case the mucosa is not elevated off the protruding parts of the ridge until it has been mobilized by osteotomy, thus taking the tension off the mucosa which is often very thin at this point. In the case of ridges and crests, therefore, the superior and inferior tunnels are not initially connected. To develop the right posterior tunnel, the septal cartilage must be mobilized and displaced to the right. For this purpose, a horizontal chondrotomy is made first (Fig. 6.16c). A sharp instrument (e. g., Cottle knife, No. 15 scalpel blade) is used to transect the cartilage at its attachment to the premaxilla and vomer to about the middle of the septum (the beginning of the sphenoid process of the cartilage). Then the attachment to the perpendicular plate is subtotally released by a vertical chondrotomy (Fig. 6.16d). Immediately before the osseocartilaginous junction, the cartilage is incised (e. g., with a Cottle elevator) and the incision extended in a caudal-to-cranial direction. Whenever possible, at least 5 mm of the suture line should be preserved to avoid rotation of the septum after any bilateral elevation of the mucosa and chondrotomies (see Fig. 6.29). If, however, there are significant septal deviations beneath the nasal dorsum, then the vertical chondrotomy must be extended until bony contact with the nasal bones is obtained, to be directly repaired at a later time (see below). Access is gained via the chondrotomies to the right side, in the correct plane directly beneath the periosteum, after displacing the mobilized cartilage to create the right posterior tunnels (superior and inferior) (Fig. 6.16c). The posteroinferior tunnel may be extended into an anteroinferior tunnel via the posterior approach. At the end of this step, the septal cartilage is still partially attached to the perpendicular plate, to the nasal bones via the upper lateral cartilages, and to the septal mucosa of the right side. It may now be swung to the side like a swinging door, allowing complete visualization of the remaining septal parts, from the nasal floor to the dorsum and from the premaxilla to the choanae. Replacement. After correction of the nasal septum pathology is complete (see below), it is necessary to initiate replacement and fixation of the mobilized nasal septum, followed by packing of the nasal cavity to achieve hematoma prophylaxis and stabilization (Fig. 6.17). At the end of the operation, as few areas of the septum as possible should remain free of cartilage and bone. Any supporting tissue which is not required for reconstruction should be replaced after straightening with the cartilage and bone crusher. The nasal cavity should first be packed, at least temporarily (e. g., with foam packs), to avoid dislocation of the fragments. The packs press both mucosal layers lightly together, while replacement is being accomplished in a posterior-to-anterior direction. Fixation. Before suture repair of the hemitransfixion, fixation of the cartilaginous septum must be checked. For this purpose, the caudal septal margin is grasped with an Adson–Brown forceps and moved. If it can be pushed into the nose, then it will definitely need suture fixation to the anterior nasal spine (Fig. 6.17). Mobility of the septal cartilage is to be anticipated, particularly when the septum has been tunnelled on both sides and the posterior chondrotomy extends as far as the undersurface of the nasal bones. In this case, the cartilaginous nasal septum is “hanging on” only by the upper lateral cartilages, and soft-tissue pressure will lead to inward rotation of the cartilaginous nasal septum (see Fig. 6.29). Packing or other stabilization measures. Stabilization and prophylaxis of a septal hematoma may be accomplished by nasal packs, septal splints, or trans-septal mattress sutures. Depending on the complexity of the operation and the extent of mobilization, a combination of these methods is recommended, with nasal packs nearly always being beneficial. Prophylaxis against hematoma formation over the cartilage is imperative (see p. 54). Trans-septal continuous mattress sutures using absorbable suture material are well suited for stabilization and hematoma prophylaxis in the cartilaginous region and near bone-free septum regions. They should not be placed too closely together, however, nor tied too tightly, in order avoid mucosal necrosis. A combination with nasal packing is recommended, at least for one night. The same applies for septal splints (Fig. 6.18), which are positioned with the aid of a septal-splint clamp and secured with two or more trans-septal mattress sutures. These should be absorbable sutures because small pieces of residual suture material tend to remain within the septum on removal. Septal splints compress the mucosa over a wider area than sutures alone and thus have less tendency to produce mucosal necrosis, provided the mattress sutures are not pulled too tightly. Care should be taken to ensure that the splints reach as far as the columellar margin, but do not cut into the upper nostril rim. Injury to the soft triangle there (see Fig. 6.33a) can result in an irreparable deformity from scar contracture. The septal splints are removed after 3–6 days, depending on the complexity of the reconstruction. Fig. 6.17 Replacement and fixation. Straightened pieces of cartilage and bone are used to fill the “empty mucosal pockets” and to support the mobilized septal cartilage from below. The caudal septum must be of adequate size (1) and secured (2 and 3) before the hemitransfixion can be repaired. Fig. 6.18a–c Fixation of the septum with septal splints. a The fashioned septal splints are fitted and secured using a septal-splint clamp. b Horizontal section demonstrating the absorbable mattress suture. c The septal splints secured by two mattress sutures. Nasal packs, inserted together with mattress sutures or septal splints, may be removed on the first postoperative day. A wide variety of materials are used for packing. Basically, they should exert a sufficient amount of pressure on the septal mucosa across as wide an area as possible, safeguard the mucosal surface, be easily removed, and provide safety against slipping down the nasopharynx. The use of several unsecured packs should be avoided, given that parts may be easily overlooked during removal and thus left behind. Fig. 6.19 Osteotomy of an ascending septal ridge and mobilization of the perpendicular plate. Three osteotomies are made using the 4-mm chisel and residual bony bridges are fractured or, with thick bone, selectively osteotomized. Resection of an ascending septal ridge/basal crest (Figs. 6.19 and 6.20). Ridges and crests are formed of septal cartilage in their cranial part and of bone on their undersurface. Basal crests can significantly narrow the piriform aperture. They are composed of the bony premaxillary ala covered by the septal cartilage, which usually deviates to the ipsilateral side. They are exposed via superior and inferior tunnels, initially leaving the mucosal attachment untouched over its lateral prominent part. Cartilage and bone are removed tangentially, using a sufficiently wide chisel or osteotome, and thus mobilized. This relaxes the mucosa, allowing the basal crest to be dissected out. Hemorrhage from the wound surface of the bone is controlled by compression. Because this bleeding can impair visibility when working on the posterior parts of the septum, removal of the basal crest is delayed until all parts of the septum have been clearly exposed. Fig. 6.20a–c Resection of a vomerine spur. a Osteotomies, first above (1), then below (2) the spur. b Elevation of the mucoperiostium from the tip of the spur, followed by extraction. c Replacement after straightening with a crusher. Ascending septal ridges follow the cranial margin of the vomer. Their undersurface consists of the bony vomerine sulcus and their cartilaginous part mainly of the sphenoid process of the septal cartilage (Fig. 6.19). Here too anterior and posterior septal tunnels are required, bearing in mind again that, on the side of the ridge, the superior and inferior tunnels should not at first be connected at the ridge margin. The posterior cut surface of the vertical chondrotomy in fact serves as the starting point for the osteotomies, preferably using the 4-mm chisel or bone scissors. At first, the thinner bone of the perpendicular plate is osteotomized above the ridge, followed by the thicker vomer below. In the dorsal region, the thin bony lamella toward the anterior wall of the sphenoid cavity is easily fractured with the elevator, allowing the ridge to be mobilized. If fracturing is unsuccessful because of dense bone, then a curved transverse chisel (see Fig. 6.6b) is placed in front of the anterior wall of the sphenoid cavity against the septum bone, which is perforated with a few blows and then mobilized. The ridge can then be displaced to the contralateral side, thus relaxing the still-attached mucosa. Superior and inferior tunnels are then connected over the margin of the ridge using an elevator and the mobilized osseocartilaginous fragment is removed (Fig. 6.20b). With ascending septal ridges the perpendicular plate of the ipsilateral side is often slanted, so it is mobilized by osteotomy below the nasal dorsum. The bone of the perpendicular plate is very thick only in the region of the bony nasal pyramid and becomes paper-thin beneath the skull base. Once the thicker bone has been divided, the lamina can usually be fractured off the skull base with mild pressure of the elevator and then extracted. Dislocation of the caudal septal margin (Fig. 6.21). An isolated dislocation of the caudal septal margin into a nostril is extremely rare. Usually the underlying cause is an osseocartilaginous crooked nose, which must be corrected accordingly (see Crooked Nose, p. 87). With an incomplete vertical cartilaginous fracture, however, it may be that only the caudal cartilaginous nasal septum has come out of the premaxillary groove on one side. Often the cartilage of the nasal septum is even found on the floor of the nose. Fig. 6.21a–c Displacement (dislocation) of the caudal septal margin and cartilaginous crooked nose with an otherwise straight nasal dorsum (basal view and horizontal section). a Lateral displacement of the caudal septal margin in the presence of a vertical cartilaginous fracture, stenosis of the right vestibule. b Shortening of the septum at the base (septum table) (1) and if necessary at the caudal margin (2). Vertical chondrotomy of the cartilage fracture resulting in a “swinging door.” Columellar pocket (3) from the nasal spine to the upper margin of the nostril (shaded area in the lateral view). c Repositioning of the septum and fixation to the periosteum of the nasal spine with a figure-of eight suture. The caudal septum is exposed via a right hemitransfixion incision. Usually both anterosuperior tunnels need to be created because the septum has deviated to one side where it is fixed in this position by the septal mucosa. This is followed by horizontal and vertical chondrotomies. The horizontal chondrotomy should simultaneously shorten the septum, which is relatively too high, sufficiently to allow it to be settled in a mid-line position without leaving too large a gap to the premaxilla. The vertical chondrotomy lies in the region of a (usually present) cartilaginous fracture line. The septum mobilized in this way is still attached to the upper lateral cartilages. Positioning of the caudal septal margin is facilitated by creating a columellar pocket, which should extend from the anterior nasal spine to the upper margin of the nostril (not to the tip of the nose). This pocket should not be dissected too deeply, especially in the lower area, otherwise a retracted and widened columella could result. Shortening of the caudal septal margin if it seems “too long” should also be considered. The caudal septum normally projects beyond the nasal spine by 1–2 mm (with a normalsized nasal spine). Even shortening it to the level of the nasal spine will result in retraction of the columella, especially if a columellar pocket has been created. The caudal septal margin should therefore only be resected, with care, if it projects beyond the spine by more than 1–2 mm. Fixation of the mobilized caudal septum to the nasal spine is accomplished with an absorbable or nonabsorbable figure-of-eight suture to ensure it is securely anchored over the middle of the nasal spine. In the region of the nasal spine, the suture is placed through the abundant fibrous tissue found there. In order to place such an anchoring stitch it is therefore necessary to avoid laying the bone completely bare when exposing the nasal spine with an elevator (e. g., Cottle knife). Deviations of the septal cartilage: caudal margin (Fig. 6.22). If the septum is placed under excessive tension by pressure from above, it dislocates out of the premaxillary groove (basal crest) and buckles. Release of septal tension can be accomplished by resection of “excess” cartilage at the premaxilla, if necessary together with part of the premaxillary ala (Fig. 6.22b). Unlike the tangential resection of a basal crest, here a complete strip of cartilaginous septum must be resected. Tension in the cartilage is only completely released, however, if the septum is tunnelled on both sides; otherwise the mucosa on the concave side, which is relatively short, keeps the septum bent like a bow. If the cartilage can be straightened up by these measures alone, then no further surgery to the cartilage is necessary. However, despite maximal release of tension, the cartilage usually remains deviated because its growth has been disrupted. In this case, either the entire cartilaginous septum can be removed and a complete septum replacement (see below) performed, or other measures are available. Often, superficial cross-hatching of the cartilage on one side is recommended. This exploits the tension forces within the cartilage: if they are neutralized on the scored side, the contraction forces on the contralateral side prevail and the cartilage arches away from the scored side (the scored surface becomes convex). This effect was examined in detail by Gibson and Davis and may be useful, e. g., for correction of the auricle (see Chapter 15), but it has significant disadvantages for the nasal septum: Fig. 6.22a–e Bending of the caudal septum. a Extensively bent cartilage with basal crest. b Relaxation of the cartilage by bilateral tunnelling and shortening at the base. c Straightening and refixation. d Residual bowing despite relaxation of the cartilage: prepared cartilaginous strut, bent in the contralateral direction. e Straightening achieved with strut, sparing out the nasal valve. Nevertheless, superficial scoring may be useful when combined with cartilage reinforcement. For this purpose, a thin, straight or slightly curved strip of cartilage is harvested from the posterior septum and sewn onto the caudal nasal septum. If it is curved, then its concave surface should come to lie on the concave side of the septum (Fig. 6.22d). The two cartilages are joined together with several absorbable mattress sutures. The cartilaginous frame straightens and reinforces the caudal septal margin. It must lie caudal to the attachment of the upper lateral cartilage, to avoid narrowing the nasal valve. A “nasal spine suture” is recommended. Deviations of the septal cartilage: cartilaginous nasal dorsum (Fig. 6.23). A C-shaped or reverse C-shaped deviation of the nasal dorsum rarely presents as an isolated finding. It is commonly a component of an osseocartilaginous crooked nose. In this case, the bony pyramid, in addition to the cartilaginous part, must be straightened by osteotomies (see Crooked Nose, p. 87). Fig. 6.23a–c Bending of the superior septal margin (cartilaginous C-shaped crooked nose). a Reverse C-shaped curve of the nasal dorsum (in the presence of a vertical cartilaginous fracture at the junction with the perpendicular plate). b Partial resection of the fracture area and detachment of the septum at the base and at the upper lateral cartilages. c Spreader graft has been inserted on the right and the upper lateral cartilages and septum have been reattached to the nasal spine. Dislocation of the caudal septum in the same direction as the deviation of the nasal dorsum is an almost regular feature. The cartilaginous septum must be mobilized accordingly via bilateral tunnels and chondrotomies, leaving it still attached only to the upper lateral cartilages and the K-region. Since in this case the nasal dorsum is also involved, it will need to be exposed by degloving. The appropriate techniques are shown and described in Figs. 6.32 and 6.33. At this point, only the operations involving the framework itself are discussed, because it belongs in the section related to nasal septum deviations. Although in this situation too, the “relatively short” upper lateral cartilage on the concave side contributes to the deviation of the nasal septum, its separation from the septum will not normally correct the bowing entirely. Maximal release of the superior septal margin is achieved by separating both upper lateral cartilages. For this purpose, an Aufricht retractor is inserted under the nasal dorsum and then the upper lateral cartilages are separated from the septum with a No. 15 blade via the superior tunnel, beginning on the undersurface of the nasal bones and extending to the nasal valve. After bilateral division, the septal cartilage remains connected only by its superior attachments to the perpendicular plate, where it must therefore be protected. As in the procedure for a deviation of the nasal septum, the cartilaginous deviation is corrected by suturing on a (or bilateral) strip (s) of cartilage (a so-called “spreader graft”). This extends from the nasal bones to the anterior inferior corner of the septum, with a height of 3–4 mm. Fixation is achieved with absorbable sutures, placed in the following manner: right upper lateral cartilage—spreader graft—septal cartilage—spreader graft, (if bilateral)—left upper lateral cartilage. This suture brings each cartilage included in the stitch to the same level, with no edges becoming visible afterward. Fixation of the spreader graft is difficult, which is why the more easily placed caudal suture is best inserted first. Once the cartilage has been secured at one point, the remaining one or two sutures are more easily placed. Here too, a nasal spine suture is recommended because of the mobilization of the septum over the premaxilla. Defects of the caudal septum: partial septal reconstruction (Fig. 6.24). Even with extensive deformities or defects of the caudal septum, there is often a strip of cartilage still present beneath the nasal dorsum. This can form the base for a reconstruction. The advantage lies in the fact that this strip of cartilage forms a pivot point with its attachment to the K-region, thus already providing two essential fixation points for the nasal septum. The aim of partial septal reconstruction is then “merely” to stably fill the gap between this residual cartilage and the premaxilla. Autologous cartilage serves as a graft, taken either from residual septum, the auricle (Figs. 6.26 and 6.27), or even a rib (see Fig. 6.52). The sufficiently long, or even too long, cartilaginous graft is first secured to the residual septum with two absorbable mattress sutures. One of these is brought out as a guide suture through the columella in the midline at the level of the upper nostril rim (Fig. 6.24b
Preliminary Remarks
Surgical Anatomy
Respiratory Function
 A certain amount of respiratory resistance is essential; the nasal airways must not be too wide.
A certain amount of respiratory resistance is essential; the nasal airways must not be too wide.
 The mucosal organ must be preserved. Extensive destruction of the mucosal surface compromises warming and humidification, as well as mucociliary transport.
The mucosal organ must be preserved. Extensive destruction of the mucosal surface compromises warming and humidification, as well as mucociliary transport.
Measuring Respiratory Function
Instruments Required for Septoplasty/Rhinoplasty
Septoplasty Instruments
Rhinoplasty Instruments
Management of Fresh Nasal Injuries
Soft-Tissue Injuries
Surgical Principle
Indications
Specific Points Regarding Informed Consent
Operative Planning
Special Instruments
Anesthesia
Surgical Technique
 Risks and Complications
Risks and Complications
Foreign Bodies
Fractures of the Bony Nasal Pyramid
 Lateral impact injury (Fig. 6.9a, b):
Lateral impact injury (Fig. 6.9a, b):
 Frontal impact injury (Fig. 6.9c, d):
Frontal impact injury (Fig. 6.9c, d):
Reduction of Fractures
Surgical Principle
 Depressions can only be reduced from an endonasal approach. Only lateral deviation of the nasal dorsum can be corrected by external pressure.
Depressions can only be reduced from an endonasal approach. Only lateral deviation of the nasal dorsum can be corrected by external pressure.
Indications
Contraindications
Anesthesia
Surgical Technique
Postoperative Care
Septal Fracture/Septal Hematoma/Septal Abscess
Surgery for Septal Hematoma/Abscess
Surgical Principle
Specific Points Regarding Informed Consent
Special Instruments and Implants
Anesthesia
Surgical Technique
Postoperative Care
Alternatives
Surgery of the Nasal Septum
Functions of the Nasal Septum

 The caudal third of the nose, including the nasal base, represents a complex system under tension. This tension is produced by the size, form, and position of the septal cartilage.
The caudal third of the nose, including the nasal base, represents a complex system under tension. This tension is produced by the size, form, and position of the septal cartilage.
 Straightening of a caudal septal deviation must not be achieved at the cost of the supportive function, otherwise the changes mentioned above may develop in more or less pronounced form.
Straightening of a caudal septal deviation must not be achieved at the cost of the supportive function, otherwise the changes mentioned above may develop in more or less pronounced form.
 If deformities have developed as a result of the loss of the supportive function, then they should not, if at all possible, be corrected by surgery of individual issues (e. g., nasal tip correction or cartilage grafting for the depressed nasal dorsum), but rather an attempt should be made to correct the underlying pathology: restoration of stability, size, and position of the caudal nasal septum (Fig. 6.13).
If deformities have developed as a result of the loss of the supportive function, then they should not, if at all possible, be corrected by surgery of individual issues (e. g., nasal tip correction or cartilage grafting for the depressed nasal dorsum), but rather an attempt should be made to correct the underlying pathology: restoration of stability, size, and position of the caudal nasal septum (Fig. 6.13).
 preservation of the connection with the perpendicular plate and/or the premaxilla, or
preservation of the connection with the perpendicular plate and/or the premaxilla, or
 fixation to the upper lateral cartilages at the junction with the nasal bone and at the anterior nasal spine.
fixation to the upper lateral cartilages at the junction with the nasal bone and at the anterior nasal spine.
Septoplasty
Surgical Principle
 1. Incision (right hemitransfixion).
1. Incision (right hemitransfixion).
Indications
 Obstruction of nasal breathing secondary to dislocation of the caudal margin of the septum, deviations of the cartilaginous nasal dorsum or the caudal septal margin, septal basal crest (caudal septum and premaxilla), ascending septal ridge and vomerine spur (septal cartilage, vomer, perpendicular plate), deviated perpendicular plate.
Obstruction of nasal breathing secondary to dislocation of the caudal margin of the septum, deviations of the cartilaginous nasal dorsum or the caudal septal margin, septal basal crest (caudal septum and premaxilla), ascending septal ridge and vomerine spur (septal cartilage, vomer, perpendicular plate), deviated perpendicular plate.
 Septal fractures or their sequelae (in particular vertical fractures at the level of the nasal valve, transverse fracture), vestibular stenoses associated with a crooked or tension nose.
Septal fractures or their sequelae (in particular vertical fractures at the level of the nasal valve, transverse fracture), vestibular stenoses associated with a crooked or tension nose.
 Septal reconstruction for saddle-nose deformity.
Septal reconstruction for saddle-nose deformity.
 For improved access during surgery of the paranasal sinuses, for posterior epistaxis, as an approach for choanal atresia, and for access to the hypophysis.
For improved access during surgery of the paranasal sinuses, for posterior epistaxis, as an approach for choanal atresia, and for access to the hypophysis.
Contraindications
 Acute rhinitis.
Acute rhinitis.
 Severe general disorders, especially coagulopathies.
Severe general disorders, especially coagulopathies.
 High-grade atrophy of the septal mucosa (e. g., after multiple previous operations).
High-grade atrophy of the septal mucosa (e. g., after multiple previous operations).
Specific Points Regarding Informed Consent
 Alterations of the form of the external nose.
Alterations of the form of the external nose.
 Olfactory dysfunction.
Olfactory dysfunction.
 Septal perforation.
Septal perforation.
 Possibility of harvesting a graft (auricle, rib).
Possibility of harvesting a graft (auricle, rib).
Operative Planning
Special Instruments and Implants
Anesthesia
Surgical Technique
(a) Preparation, Incision, Approach
 These are identical for the majority of septal deformities, with just a few exceptions.
These are identical for the majority of septal deformities, with just a few exceptions.
(b) Correction of Various Septum Deformities
 Ascending septal ridge, basal crest (see Figs. 6.19 and 6.20).
Ascending septal ridge, basal crest (see Figs. 6.19 and 6.20).
 Dislocation of the caudal septal margin (see Fig. 6.21).
Dislocation of the caudal septal margin (see Fig. 6.21).
 Deviation of the septal cartilage:
Deviation of the septal cartilage:
(c) Defects or Insufficiency of the Caudal Septum
 Partial septal reconstruction
Partial septal reconstruction
 Total septal reconstruction (septal replacement) (see Figs. 6.25, 6.26, 6.27)
Total septal reconstruction (septal replacement) (see Figs. 6.25, 6.26, 6.27)
(d) Replacement, Fixation, Packing
Correction of Individual Septal Deformities or Defects
 It is not known how many and how deep incisions should be made on the concave side of the septal cartilage to straighten an existing deviation exactly.
It is not known how many and how deep incisions should be made on the concave side of the septal cartilage to straighten an existing deviation exactly.
 Cartilage scoring weakens stability, so that its supportive function may be compromised in the long term.
Cartilage scoring weakens stability, so that its supportive function may be compromised in the long term.
 It is a dynamic process, the final state of which cannot be exactly predicted.
It is a dynamic process, the final state of which cannot be exactly predicted.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


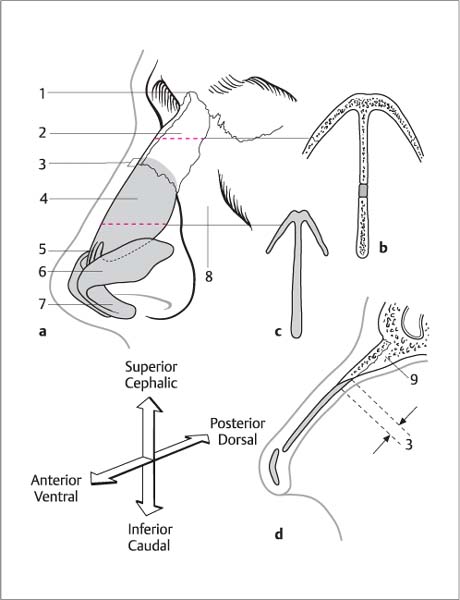
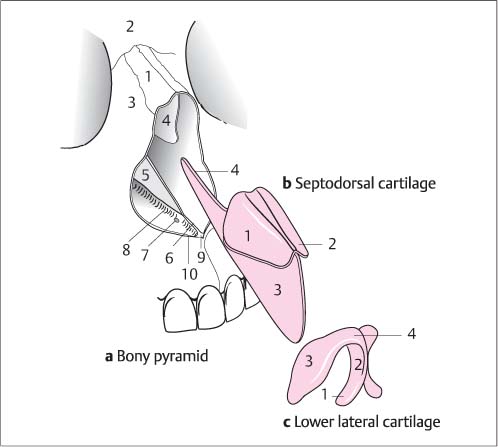
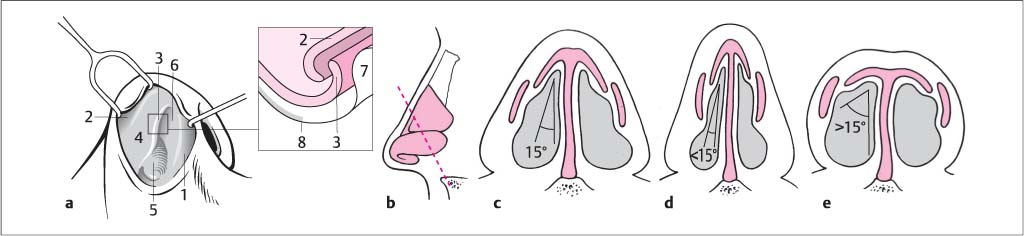
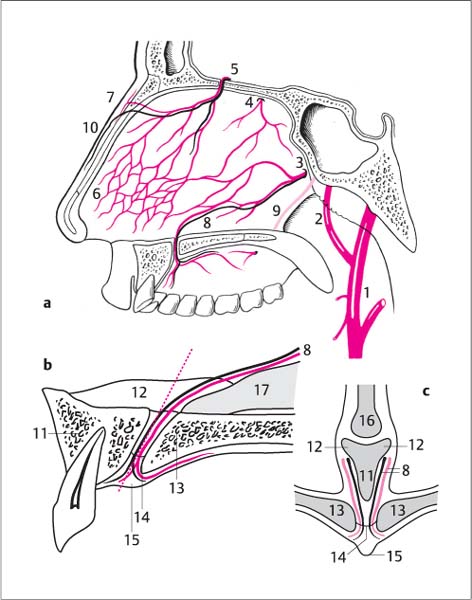
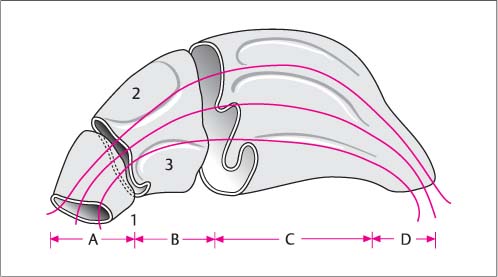
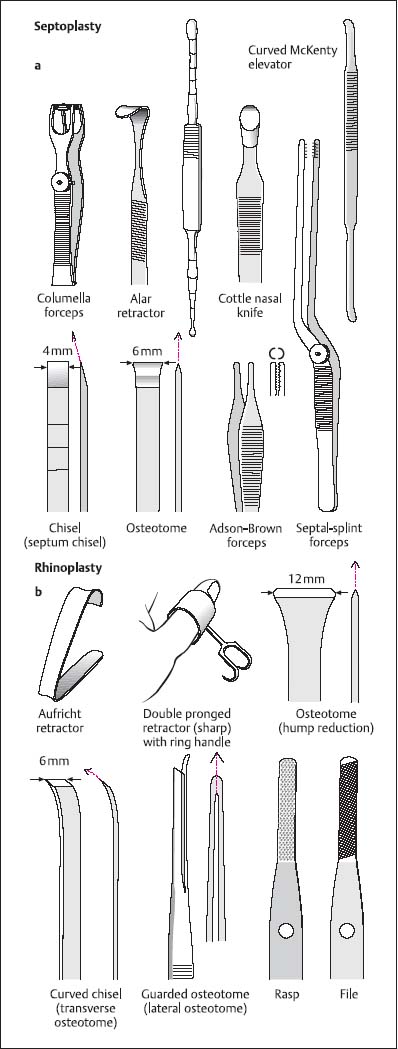
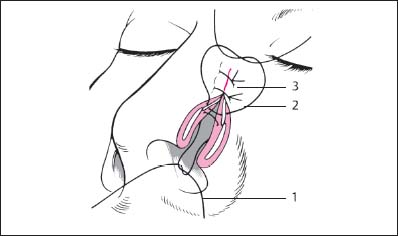
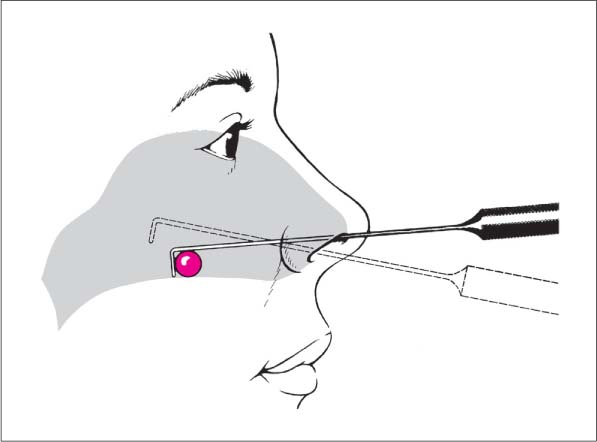
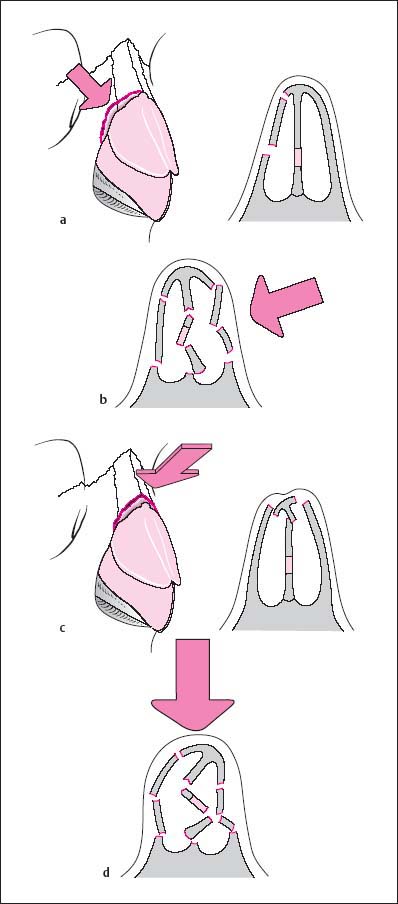
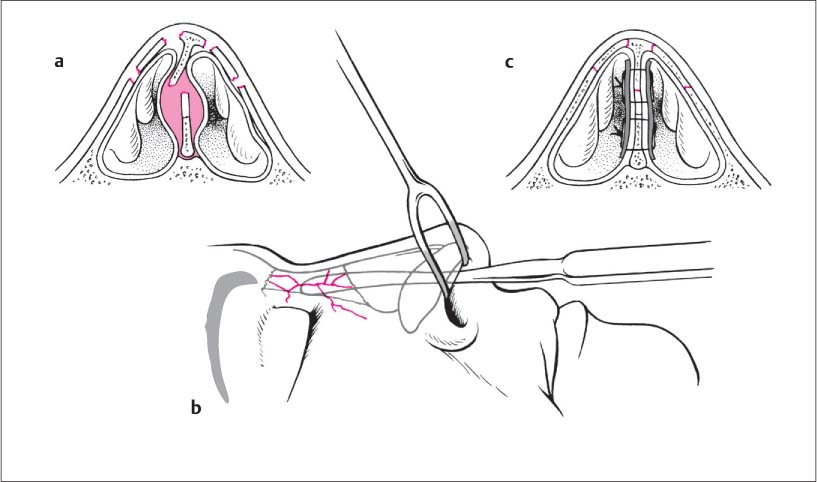
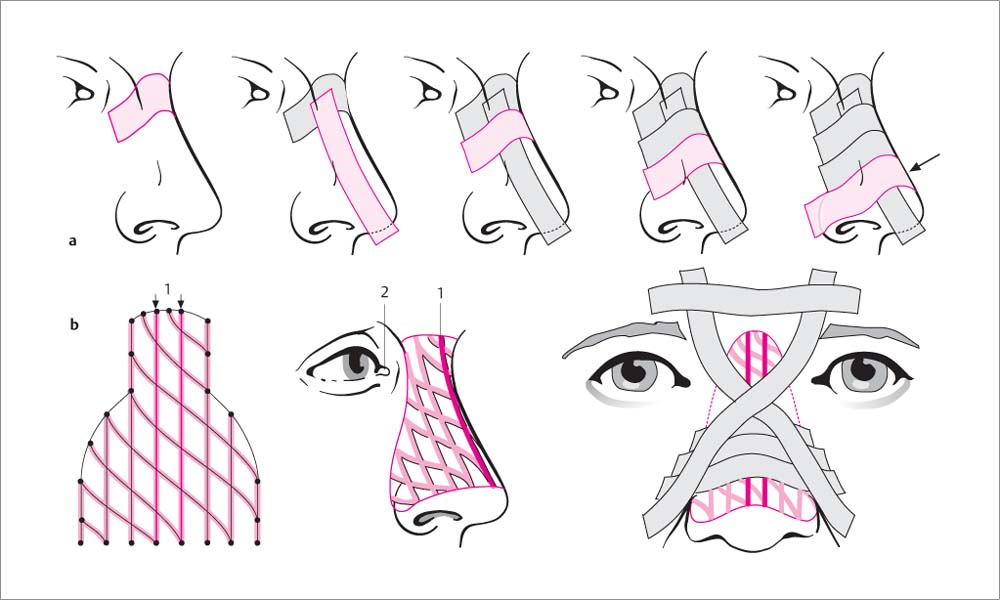
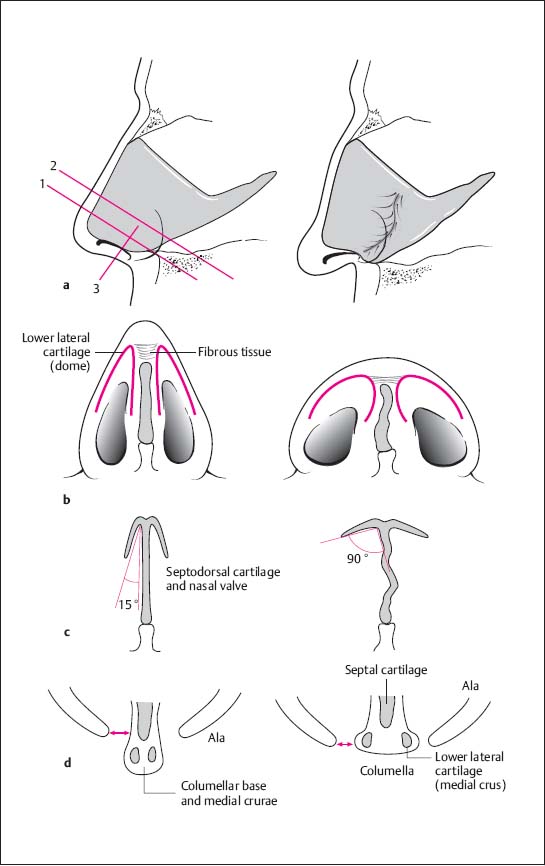
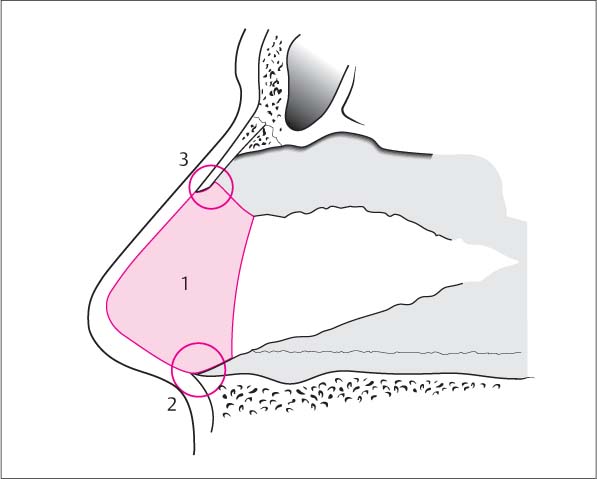
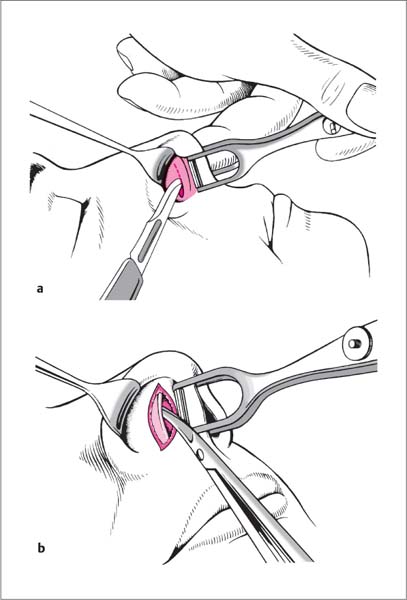
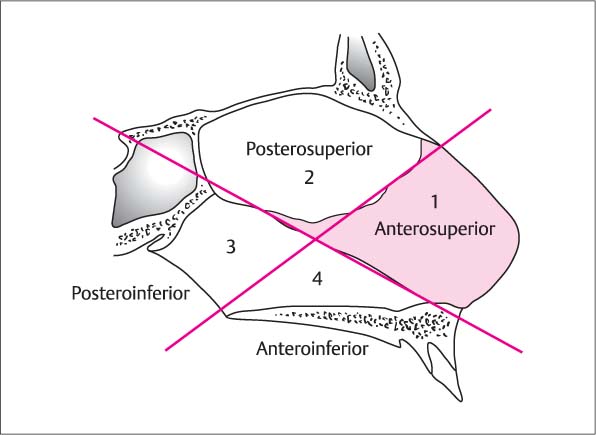
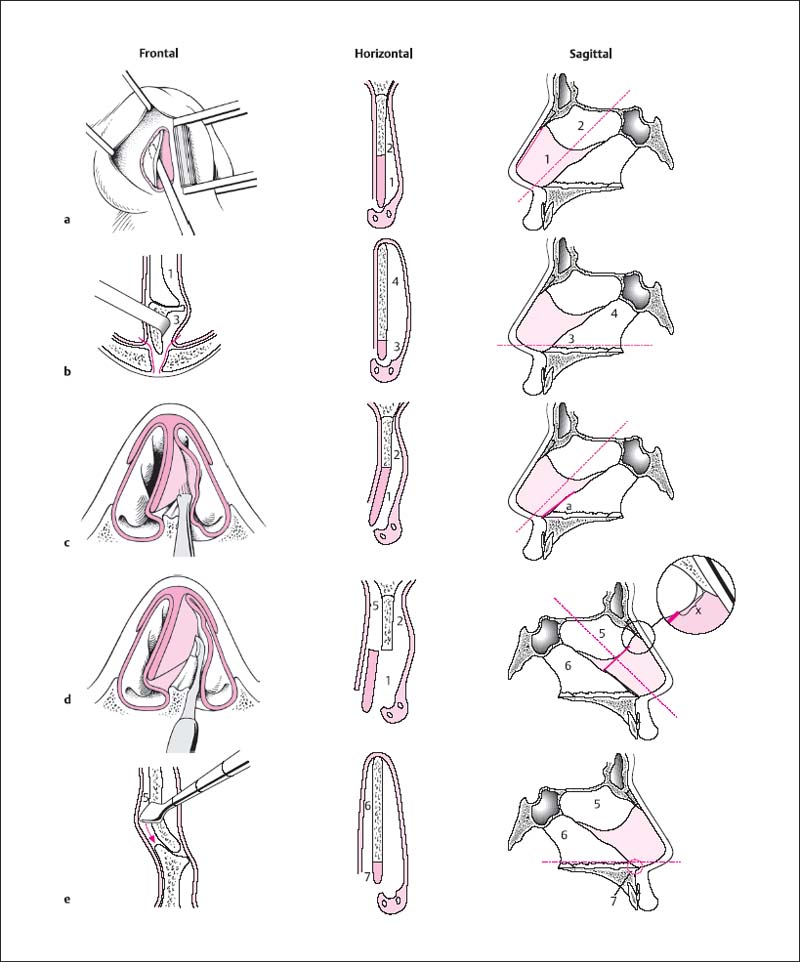
 Tunnelling over cartilage is done with blunt instruments to avoid injury to the cartilage, whereas sharp instruments are used over bone.
Tunnelling over cartilage is done with blunt instruments to avoid injury to the cartilage, whereas sharp instruments are used over bone.