(1)
Department of Ophthalmology, St. Thomas’ Hospital, London, UK
17.2 Vitreous Anomalies
17.2.2 Asteroid Hyalosis
17.2.3 Amyloidosis
17.4 Optic Disc Anomalies
17.4.2 Morning Glory Syndrome
17.6 Marfan’s Syndrome
17.8.1 Clinical Features
17.8.2 Surgery
17.9 Terson’s Syndrome
17.11 Retinal Prosthesis
17.12 Summary
Abstract
Symptomatic vitreous floaters are common. In most circumstances patients find the nuisance of floaters tolerable; however, there are some eyes which have considerable debris and some patients who require clarity of the vision, for example, musicians, in particular, find reading music difficult when floaters are present.
Electronic supplementary material
The online version of this chapter (doi:10.1007/978-3-642-31872-6_17) contains supplementary material, which is available to authorized users.
17.1 Vitrectomy for Vitreous Opacities
Symptomatic vitreous floaters are common. In most circumstances patients find the nuisance of floaters tolerable; however, there are some eyes which have considerable debris and some patients who require clarity of the vision, for example, musicians, in particular, find reading music difficult when floaters are present.
Common causes of persistent floaters:
Posterior vitreous detachment
Vitreous syneresis, for example, high myopia
Resolved vitreous haemorrhage
Uveitis
Asteroid hyalosis
Silicone oil emulsion
Make sure that the symptoms are consistent with floaters and not scotoma; see Chap. 4. It is reassuring to detect vitreous opacities on ophthalmoscopy before offering surgery. Watch out for previously undiagnosed conditions such as intermediate uveitis. Be aware that the vitreous is often not detached. It is helpful to determine if the vitreous is detached with ultrasound to look for gross detachment and OCT, to look for partial detachment or to confirm attachment of the vitreous. In the presence of an attached vitreous, the surgeon may expect an increase in the chance of complications such as retinal tear formation, macular ERM or hole formation, and vitreous haemorrhage or more likelihood for gas insertion. Overall complications have been described in xxx %. Ref. Patients are however very pleased to have no floaters after successful surgery. Careful preparation of the expectations of the patient and communication of the risks of surgery is particularly important preoperatively.
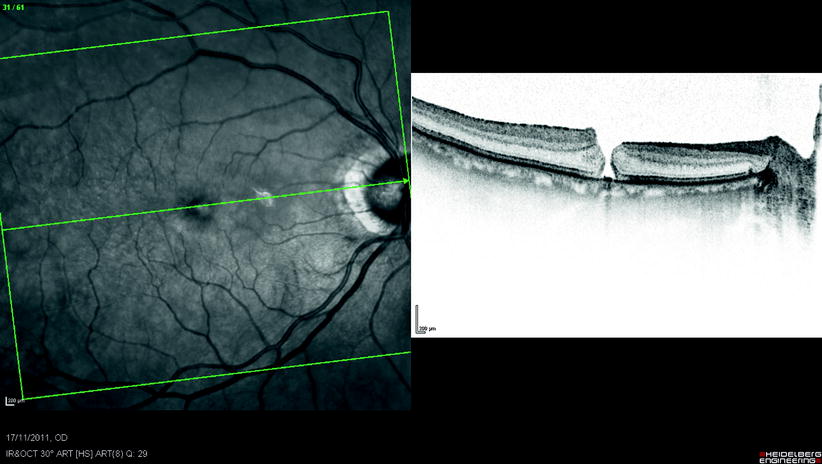
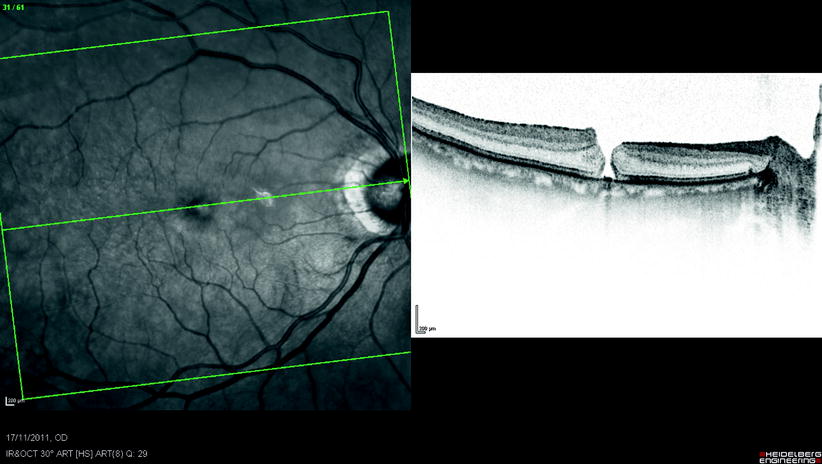
Fig. 17.1
This patient who was a surgeon had PPV for vitreous floaters from syneresis and developed a macular hole after the surgery which required further surgery
Surgical Pearl of Wisdom
Vitrectomy for floaters is surgery VR surgeons usually try to avoid, as often these patients have very good vision, and removal of floaters is considered unnecessarily risky.
Should the decision for surgery be made, a few points are useful to remember.
I operated a patient (female, 54 years old, portrait painter) using 25-gauge instrumentation for visible floaters in the right eye. On slit lamp examination, large floaters were visible and indicated a posterior vitreous detachment (PVD). However, during surgery, triamcinolone staining of the vitreous showed there was no PVD, rather the vitreous was extremely adherent to both the disc and the macula.
As surgery had been started, I was now obliged to induce the PVD, which was achieved with great difficulty. As the vitreous came off the disc, a spontaneous haemorrhage of a peripapillary vessel occurred due to traction. I raised the infusion bottle to 60 mmHg to stop the bleeding, but postoperatively there was a segment of disc swelling.
Vision is 6/6, but the patient had a small sickle-shaped scotoma, corresponding to the area of disc swelling.
Postoperatively we injected triamcinolone to try and reduce the inflammatory component. The scotoma is becoming smaller and ‘see through’, however, is still visually disturbing, especially in view of this patient’s profession.
Therefore:
1.
Check extensively for signs of a PVD before surgery.
2.
Stain the vitreous with triamcinolone at the time of surgery, as it helps confirm the PVD. Also, often there are areas of adherent vitreous in the posterior pole; these may contribute to the patient’s awareness of floaters.
3.
Take time to explain the risks of surgery very extensively.
Sarit Y Lesnik Oberstein, Dept of Ophthalmology, University of Amsterdam, Amsterdam, The Netherlands
17.2 Vitreous Anomalies
17.2.1 Persistent Hyperplastic Primary Vitreous
The most frequent severe developmental anomaly in the vitreous is persistent hyperplastic primary vitreous, which usually presents in infancy as a microphthalmic strabismic eye with leukocoria. Pupil dilatation may demonstrate dragging of the ciliary processes towards a central plaque of fibrovascular tissue which invades the lens posteriorly and ultimately causes a complete cataract and secondary angle closure glaucoma. Using vitrectomy techniques the anomaly can be removed but with little visual recovery (Laatikainen and Tarkkanen 1982).
17.2.2 Asteroid Hyalosis

Fig. 17.2
Asteroid hyalosis in the anterior vitreous
Asteroid hyalosis is a specific form of gel degeneration in which globules of calcium soaps (possibly hydroxylapatite, calcium and phosphate) aggregate on vitreous fibrils and move with the gel on eye movement (Winkler and Lunsdorf 2001). It has been found in 2 % of autopsy specimens (Fawzi et al. 2005) with increased prevalence with increasing age and the presence of PVD. The process of formation may be similar to lithiasis, stone formation in the body. Dense, asteroid bodies may preclude ophthalmoscopic visualisation of the retina, though they rarely impair the patient’s vision. They are not associated with any systemic condition, and their aetiology is unknown. Occasionally vitrectomy is required to improve vision (Parnes et al. 1998; Feist et al. 1990; Renaldo 1981); in my experience the vitreous is attached and is difficult to get off. This is probably because there is no pathological process at the vitreoretinal interface unlike conditions such as macular hole where a microvitreoretinal separation is present.
17.2.3 Amyloidosis
Amyloidosis of the vitreous is a rare condition usually associated with primary or familial (dominantly inherited) forms of amyloidosis. Proteinaceous material, probably derived from the retinal circulation, becomes coated on the collagenous framework of the gel bilaterally to produce a ‘glass-wool’ opacification; associated cellular invasion is conspicuous by its absence.
17.3 Retinal Haemangioma and Telangiectasia
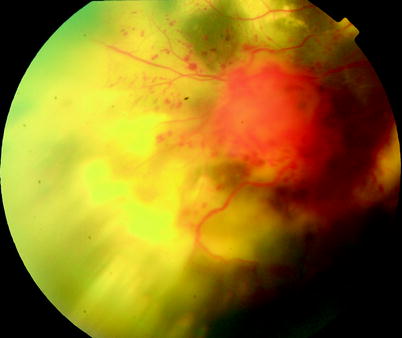
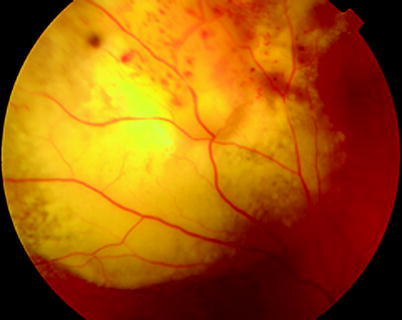
Fig. 17.3
A peripheral lesion in Coat’s disease

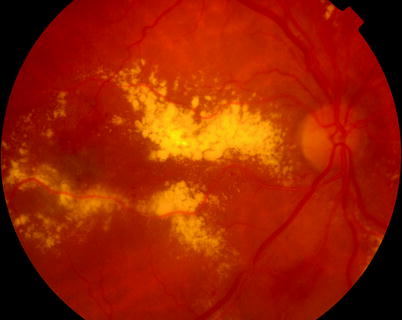
Fig. 17.4
Extension of exudate into the macula in Coat’s disease

Fig. 17.5
A patient with Coat’s disease with progression of exudation over 3 years in their third decade

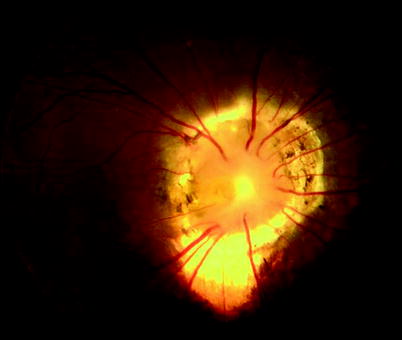
Fig. 17.7
There is a spectrum of retinal vascular anomalies which may affect the eye including Coat’s disease, isolated angiomas and von Hipple–Lindau. In this young patient there is angioma on the disc causing macular swelling. There is no effective way of treating the optic nerve disease. FFA confirms leakage (see Fig. 17.8)

Fig. 17.8
See previous figure

Fig. 17.9
A small angioma in von Hipple–Lindau. These angiomata can produce devastating problems within the retina, such as exudative retinal detachment, vitreous haemorrhage and subretinal and intraretinal exudation

Fig. 17.10
A large angioma in VHL
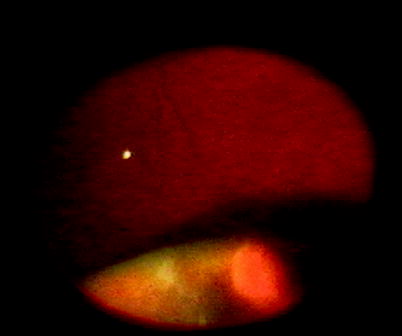
Fig. 17.11
A peripheral angioma seen on indentation
Retinal angioma (retinal capillary haemangioma) can occur as a solitary lesion not associated with systemic disease or as multiple lesions in von Hipple–Lindau disease (VHL). In the former, the mean age at presentation (36 years) is older than in von Hipple–Lindau (17 years) (Singh et al. 2001a, b). Most tumours are located in the superotemporal quadrant in the retinal mid-periphery (Singh et al. 2001c). Seventeen percent of angiomas in VHL occur on the optic nerve (Singh et al. 2002). New tumours are rare in patients without VHL. Isolated retinal angiomas have been described after RRD surgery (Gray and Gregor 1994).
In VHL a mean of four tumours are seen per eye, and new lesions tend to occur before the age of 47 years. In VHL extraocular lesions occur as:
1.
Central nervous system haemangioma
2.
Renal cyst, renal carcinoma
3.
Pancreatic cysts and adenoma, pancreatic islet cell tumours
4.
Phaeochromocytoma
5.
Endolymphatic sac tumour of the inner ear
6.
Cystadenoma of the epididiymis and broad ligament
Retinal angiomas may cause vitreous haemorrhage, tractional, exudative or rhegmatogenous retinal detachment and macular pucker or hole (Inoue et al. 2004; Schwartz et al. 1990; Laatikainen et al. 1989; Ferguson and Singh 2002; Loewenstein 1995; Machemer and Williams 1988). Treatment may involve
Unfortunately PVR formation is common making surgery hazardous.
External beam radiotherapy has been tried where other treatments have failed to regress the lesions (Raja et al. 2004), but as yet an appropriate therapeutic option is not available for optic nerve lesions (Garcia-Arumi et al. 2000).


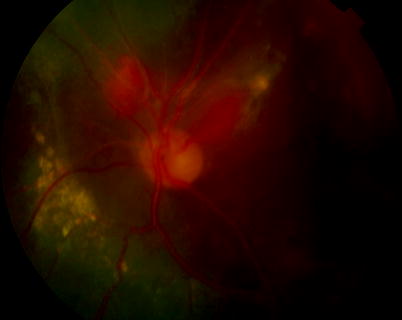
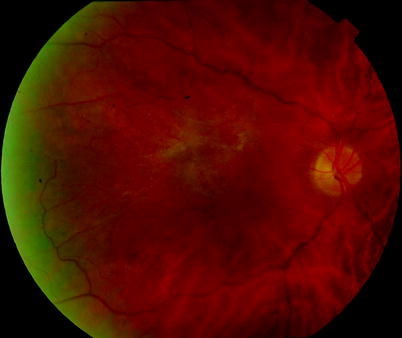
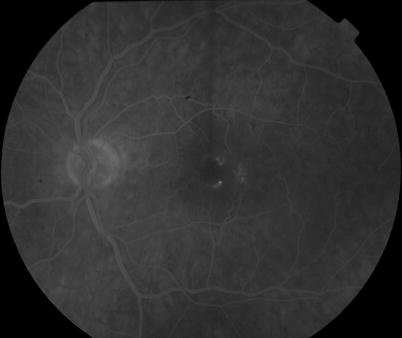

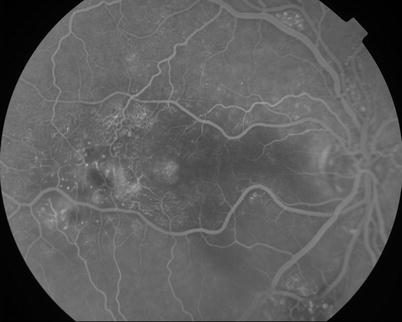
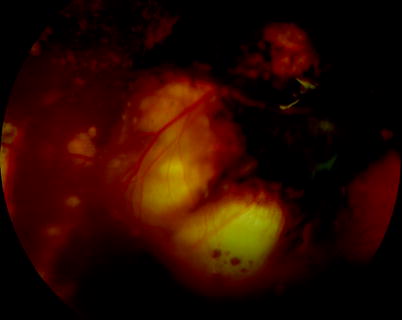
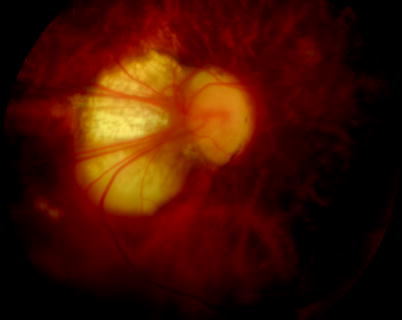

Fig. 17.12
A composite picture showing treated lesions, macular exudation and an optic nerve head angioma

Fig. 17.13
Vitreoretinal traction over a lesion in VHL
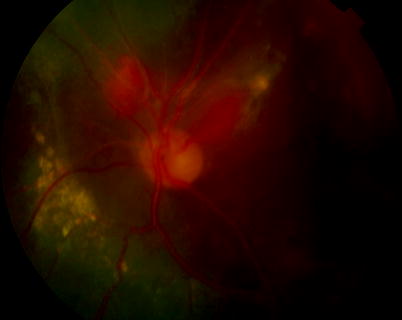
Fig. 17.14
This patient had 16 procedures on his eyes for the retinal complications of von Hipple–Lindau which included rhegmatogenous retinal detachment, exudative retinal detachment, PVR and cystoid macular oedema. Only the eye shown retained useful vision of 20/120 but with untreatable peripapillary angiomas
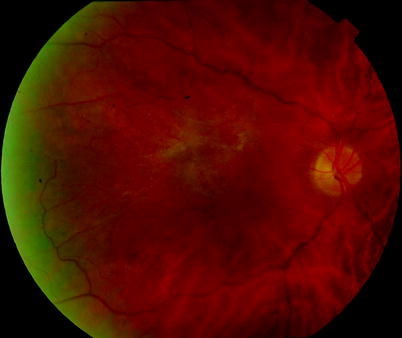
Fig. 17.15
Parafoveal telangiectasia causing an ERM
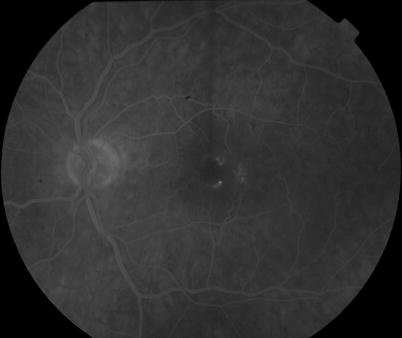
Fig. 17.16
FFA of parafoveal telangiectasia causing an ERM

Fig. 17.17
Multiple leaking telangiectasia sometimes called Leber’s miliary aneurysms
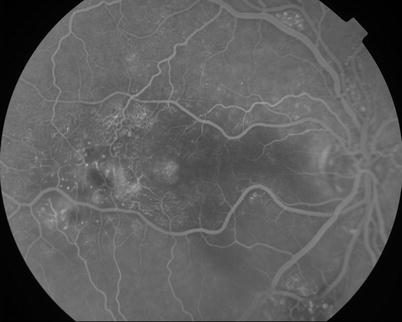
Fig. 17.19
See previous figure
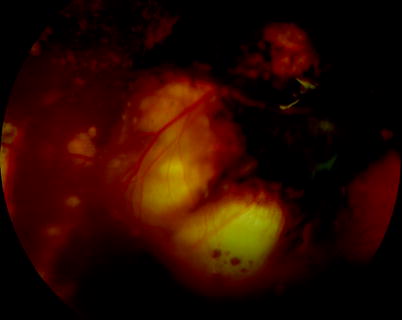
Fig. 17.20
Familial exudative vitreoretinopathy presents with a dragged disc and retinal telangiectasia. Occasionally RRD occurs but with a high chance of PVR as with most retinal telangiectatic disease
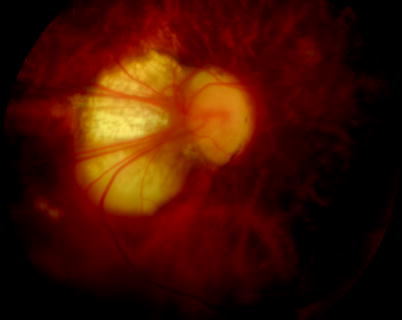
Fig. 17.21
The retina is dragged over the disc in this patient with FEVR, the macula is actually on the right of the disc in this right eye. The surgeon can be fooled during surgery into thinking that the macula is on the left running the risk that the macula will not be appropriately protected from surgical manoeuvres
17.4 Optic Disc Anomalies
Various optic disc anomalies are associated with retinal elevation.
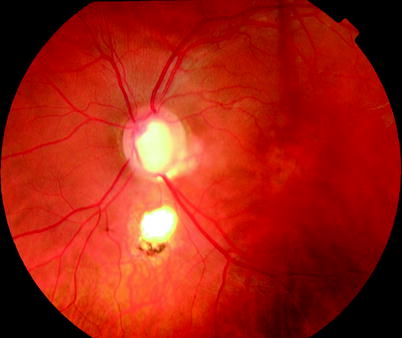
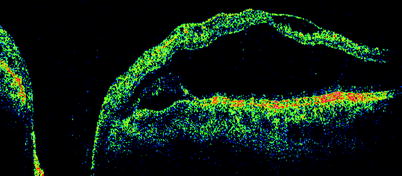
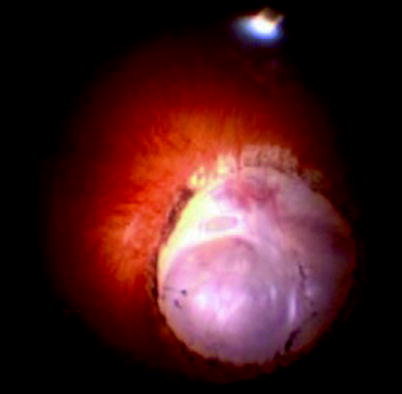
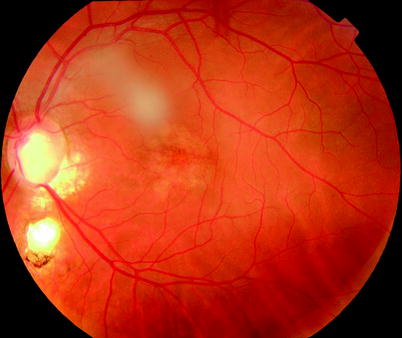
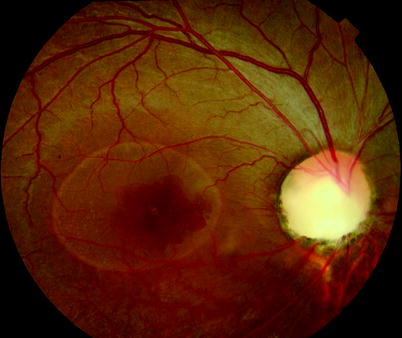
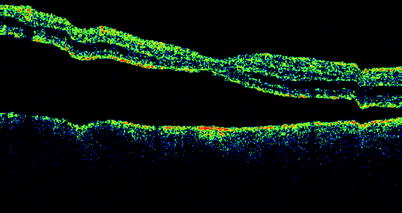
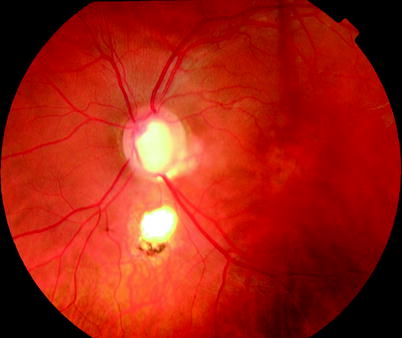
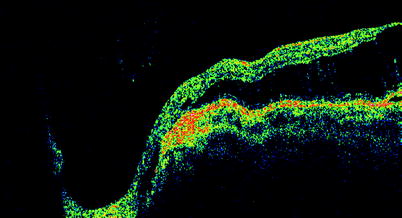
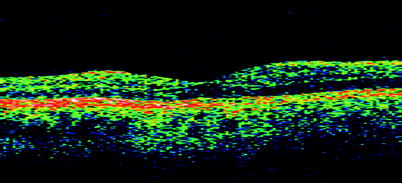
Fig. 17.22
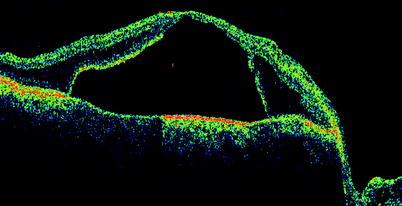
An optic disc coloboma causing a macular retinoschisis. OCT shows a retinoschisis post operatively after pneumatic displacement by pneumatic retinopexy with SF6 gas and peripapillary laser application. The OCT demonstrates closure of the schisis around the peripapillary area and reduction in height of the schisis associated with visual improvement to 20/30 see 17.23 and 17.25-27
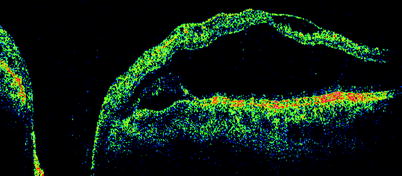
Fig. 17.23
See previous figure
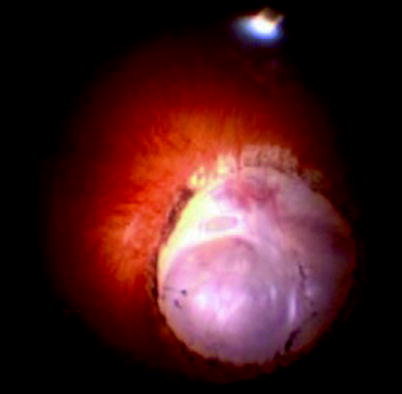
Fig. 17.24
Large optic disc coloboma
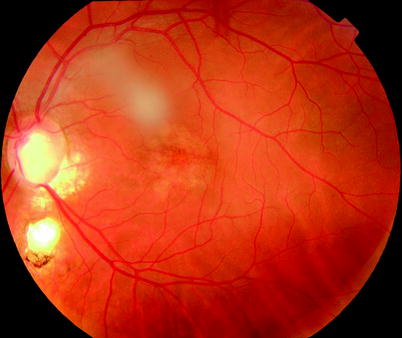
Fig. 17.26
Three years later the patient has a flat fovea
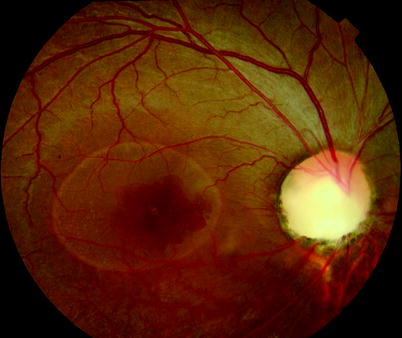
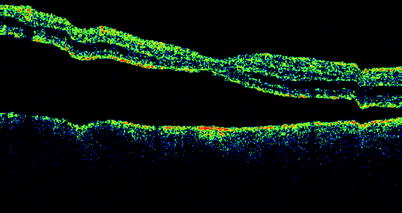
Fig. 17.30
Fluid has been displaced inferiorly by gas injection
17.4.1 Optic Disc Pits and Optic Disc Coloboma
The source of the intraretinal and subretinal fluid remains a mystery in these conditions with theories postulated that the fluid arises from the disc perhaps leaking from the subarachnoid space or from a defect in the surface of the disc allowing vitreous fluid to enter. Certainly it is usually impossible to detect a retinal break. The retinal elevation appears to consist of a multilayered schisis of the retina. Therapy is controversial with peripapillary laser applied to try to block any channels for the dispersion of fluid into the macula. Both pneumatic retinopexy and vitrectomy and gas have been used to oppose the peripapillary retina to allow the laser to seal and to disperse macular fluid (Guraya et al. 2004; Lincoff and Kreissig 1998). Others have used vitrectomy and gas without laser with slow resolution of the RD (Hirakata et al. 2005); however, spontaneous resolution may also occur.
I perform PPV, laser to the RPE at the edge of the optic disc. The retina does not need to be flat during the laser application indeed its elevation helps prevent damage to the overlying nerve fibres. Apply the laser only to the area with elevated retina with minimal blanching of the retina. Insert 30 % perfluoropropane.
Warn the patient that the resolution of the retinal elevation may take 9 months postoperatively.
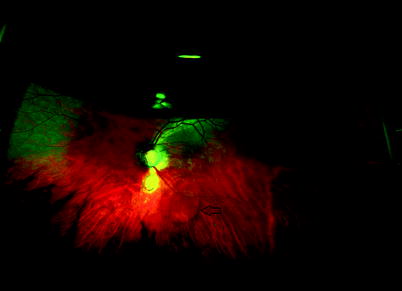
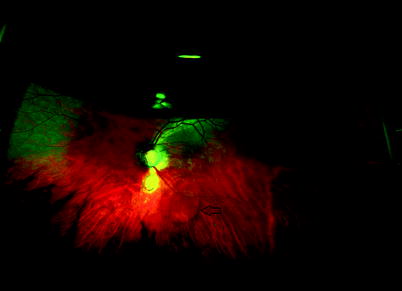
Fig. 17.31
A wide-angle view of an eye with gas insertion for optic pit maculopathy. The patient also has a chorioretinal coloboma. Note the displacement of retinal fluid inferiorly (arrow)
Some patients may be suffering from renal coloboma syndrome with renal hypoplasia and a mutation of the PAX2 gene, and therefore renal investigations may be advisable (Ttie-Bitach et al. 2001).
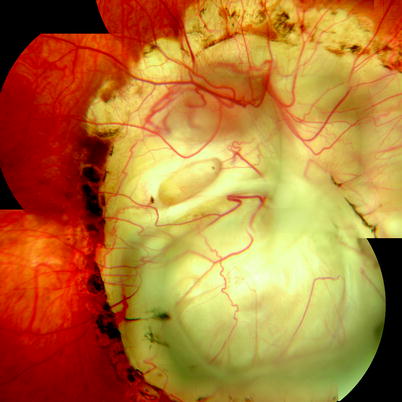
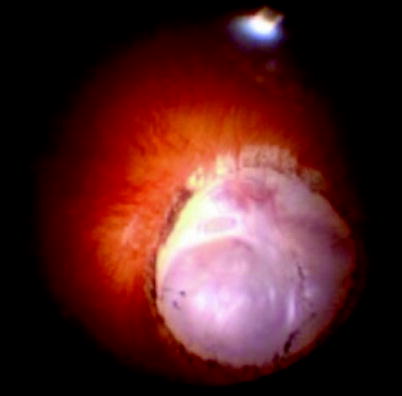
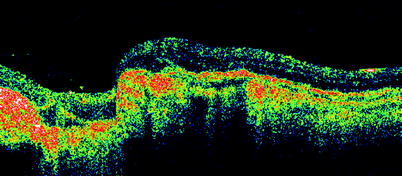

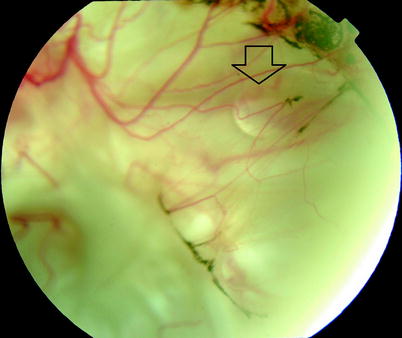
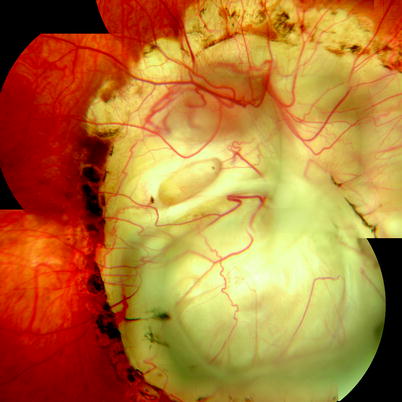
Fig. 17.32
A 14-year-old patient with CHARGE syndrome (coloboma of the eye, heart defects, atresia of the nasal choanae, retardation of growth, genitourinary abnormalities, ear abnormalities and deafness) presented with RRD from the right coloboma which was successfully treated with laser to the edge of the coloboma and 2 months silicone oil tamponade then removal of the oil, retaining 20/120 vision. A postoperative view is shown with laser scars in the right eye see Fig. 17.32 and left eye Fig. 17.33
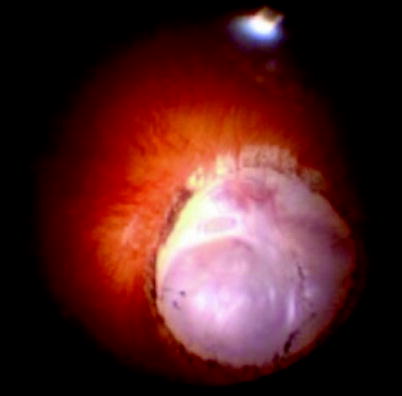
Fig. 17.34
A peroperative view of a coloboma in CHARGE syndrome
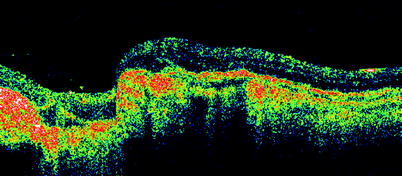
Fig. 17.35
An OCT of the edge of the coloboma in a patient with CHARGE syndrome. Note the sudden posterior displacement of the tissues with some evidence of membranes in the coloboma

Fig. 17.36
Retinal adhesion from laser photocoagulation to prevent spread of SRF can be employed in selected cases. This can only be used successfully in eyes in which there is very gradual fluid accumulation (tiny break or formed attached vitreous) or little momentum in the SRF to lift the adherent edge (shallow SRF or low volume of SRF). It has been used successfully in this patient with CHARGE who has a shallow ‘blister’ of SRF leaking under the retina on the edge of the coloboma, thereby avoiding more invasive surgery in this complex case
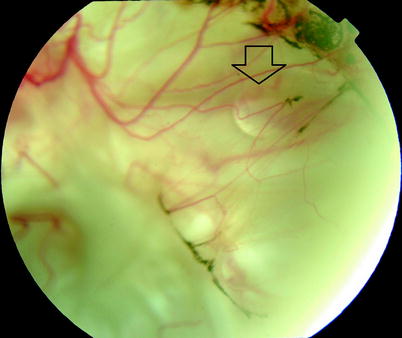
Fig. 17.37
A droplet of oil (arrow) can be seen under the retina in the coloboma, suggesting a communication from the vitreous cavity and the subretinal space postoperatively
17.4.2 Morning Glory Syndrome