Chapter 6 Management of the Patient with Ocular Allergy
Epidemiology/Prevalence/Burden
▪ Acute Allergic Conjunctivitis
Seasonal (SAC) and perennial (PAC) allergic conjunctivitis are the most common forms of allergic conjunctivitis, SAC representing approximately half of the cases of ocular allergy.1 Perennial allergic conjunctivitis is identical to SAC, but with year-round symptoms. In SAC, the allergens are the pollens, and in PAC dust, mite feces, animal dander, and feathers are the common provocative antigens.2
Allergic conjunctivitis may affect individuals of all ages, social strata, and gender. Atopic ocular disorders are common but underdiagnosed. Most epidemiologic studies lack objective testing data to describe the prevalence and natural history of these diseases in an accurate manner, primarily centering on seasonal and perennial allergic conjunctivitis. These vary among geographic regions and are more common in warmer climates. The prevalence of SAC is reported to be as high as 33% in certain populations.3 SAC occurs in a large proportion of people afflicted by seasonal rhinitis. The seasonal influence on the appearance and disappearance of the symptoms is obvious from the history, and a positive family history of atopy is obtained in about 70% of patients with SAC.2
▪ Chronic Allergic Conjunctivitis
Giant Papillary Conjunctivitis
Giant papillary conjunctivitis (GPC) is a well-known complication of chronic contact lens use, but may also be observed in patients after cataract surgery, ocular prosthesis wearing, extruding scleral buckle retinal detachment surgery material, and corneal foreign bodies.4 A retrospective study performed by Donshik and Porazinski5 from 1993 to 1997, reported that 21.27% of contact lens users developed GPC. Most of these patients replaced their lenses at 4 weeks or longer and had previous history of allergy. The authors did not find a relationship between GPC and sex, age, average daily wearing time, contact lens material, or fitting characteristics of the lens. Unfortunately, the epidemiologic data on GPC is limited and outdated. The contact lens industry has made great advances in lens material as well as in cleaning solutions, which should reduce the prevalence of GPC. Strict FDA guidelines regarding lens replacement are now implemented, possibly decreasing complications in contact lens users.
Vernal Keratoconjunctivitis
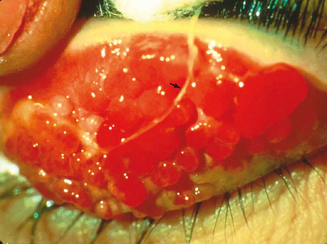
Vernal keratoconjunctivitis (VKC) is a chronic allergic conjunctival inflammatory disorder frequently associated with secondary keratopathy. The characteristic hallmark of VKC is the presence of giant papillae, usually in the upper tarsal conjunctiva, but in some cases in the conjunctiva at the corneoscleral limbus (Figure 6.1). It is a disease predominantly of young men, with pronounced seasonal (spring) influence, probably secondary to vernal allergens, but perennial forms exist as well.2 VKC may be differentiated from SAC in that increased disease activity may also occur in summer and SAC patients never develop the giant papillae so characteristic of VKC. A long-term follow-up study performed by Bonini reports that approximately 23% of patients have a perennial form of VKC and that 60% have additional recurrences during winter.6 He found that almost 16% of patients with longstanding seasonal VKC developed chronic, perennial inflammation after an average of 3 years, implying that persistent disease is most likely to develop in this population.
A personal or family history of atopy is usually uncovered in VKC patients, and in many cases, specific allergens to which the patient is sensitive can be determined by history and by scratch and prick allergen skin testing. One particularly notorious provocative allergen in patients with VKC is the house dust mite and its feces.2
Vernal keratoconjunctivitis has a worldwide distribution, with pronounced regional variations and prevalence. It is most common in the Mediterranean region and Central and South America, and is rare in North America and Northern Europe.2 VKC may represent as much as 3% of serious ophthalmic disease in some regions,7 whereas in Northern Europe and North America, the prevalence is about 1 in 5000 cases of eye disease.8
VKC has been reported to affect patients from 1 month old to more than 70 years of age, but at least 50% of the patients in most reported series are between 5 and 25 years of age. In most patients, the disease resolves spontaneously within 10 years of onset. Regrettably, however, the improperly treated patient may be blind by the time this happens.2
In a study by Dart,9 78% of 120 patients with VKC developed the disorder before the age of 16 years. Dart found that the corneal complications of VKC in this population occurred almost exclusively in patients with palpebral or mixed palpebral and limbal VKC. He found no differences in serum or tear IgE levels among VKC patients with the various forms of the disease; the VKC patients did have higher than normal levels of IgE, and specific IgE to cat dander and to house dust mites was detected. This finding agrees with other studies which suggest that this disorder is not solely IgE-mediated.2 Twenty-seven percent of the study population lost vision because of VKC, and Dart commented, “therapeutic complications are also common, and may lead to blindness.”
Atopic Keratoconjunctivitis
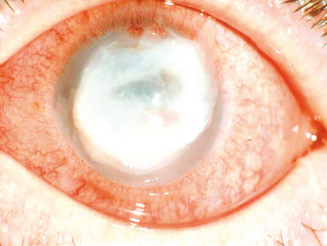
Hogan10 defined atopic keratoconjunctivitis in 1952 as allergic keratoconjunctivitis occurring in association with atopic dermatitis (eczema). It is estimated that between 25% and 40% of patients with atopic dermatitis have some type of ocular complication.11,12 Chronic allergic conjunctivitis with superficial punctate keratitis was the most frequent clinical presentation.12 This represents a substantial number of people who are at risk of bilateral blinding corneal complications from this complex inflammatory disorder. AKC most frequently occurs in men. It typically presents in the late teen years or early twenties, rarely before puberty, and may persist until the fourth or fifth decade of life.1 A recent study shows that childhood-onset adult AKC patients have greater ocular surface epithelial damage due to the effects of prolonged inflammation.13 It is this keratopathy which produces such profound disability for patients with AKC (Figure 6.2).
Relevant Anatomy and Physiology
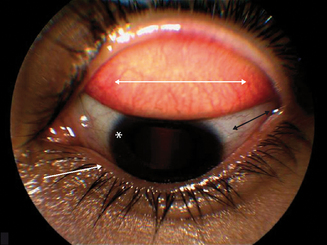
The conjunctiva is a thin, transparent, vascularized mucous membrane that covers the posterior surface of the eyelids, reflects forwards on the eye at the fornix, to cover the anterior sclera. Anatomically, the conjunctiva is composed of a bulbar and a palpebral component. The bulbar conjunctiva is a thin, semitransparent, colorless tissue that covers the sclera up to the corneoscleral junction, the limbus. The palpebral conjunctiva, a thick, opaque, red tissue, is further divided into marginal, tarsal, and orbital zones. The marginal zone exhibits minimal keratinization and is located between the skin and the conjunctiva. The tarsal conjunctiva is a relatively smooth fibrous layer that gives the eyelid its characteristic shape, evident upon eyelid eversion (Figure 6.3).
Pathophysiology
The pathogenesis of ocular allergic diseases involves multiple steps. Allergic conjunctivitis represents a pure type 1 hypersensitivity response.2 Although the pathogenesis of GPC, VKC, and AKC involves more complex immunoinflammatory reaction, a type 1 hypersensitivity response has also been implicated in each of these disorders.14 Histopathologic characterization of inflamed conjunctiva shows similar cellular infiltrate among the atopic ocular disorders, consisting predominantly of eosinophils and lymphocytes.2 Studies illustrate the importance of the relationship between adhesion molecules and chemokines in the recruitment of leukocytes in the ocular allergic inflammatory response. With an advancing knowledge of the mechanisms involved in leukocyte recruitment into ocular inflammatory sites, more definitive treatment strategies are currently under investigation.
▪ Acute Allergic Conjunctivitis
Pathophysiologic features of SAC and PAC are prototypic type 1 anaphylactic hypersensitivity reactions. In sensitized individuals the allergen crosslinks IgE antibodies on the surface of mast cells and basophils, resulting in the degranulation of these cells with release of mediators including histamine and kinins. Patients with SAC and PAC have elevated levels of IgE in their tears and serum and pollen specificity has been demonstrated in both diseases.15
Seasonal allergic conjunctivitis is accompanied by migration of mast cells into the conjunctival epithelium,16 and by an increase in tear levels of the mast cell neutral protease tryptase.17 Challenging sensitized individuals reproduces ocular allergy features of increased tear levels of the inflammatory mediators histamine, all products of mast cell degranulation, and prostaglandin D2 and leukotrienes C4 and D4, newly produced mediators.18 Subsequent studies reveal that mast cells store and secrete a range of multifunctional cytokines including interleukin 4 (IL-4), IL-5, IL-6, IL-8, and tumor necrosis factor alfa (TNF-α).19 The release of these chemokines suggests that the mast cell has the capacity of upregulating local allergic responses, as well as organizing the participation of other inflammatory cells. IL-4 regulates the expression of VCAM-1 (vascular cell adhesion molecule 1) which is involved in the selective recruitment of eosinophils from the microvasculature,20 a critical event in the blinding ocular allergies, VKC and AKC.
As previously noted, mast cells (MC) are critical components of acute allergic disorders. Anderson and colleagues investigated the expression of inflammatory cytokines between the two known subsets of mast cells, MCTC and MCT,21 which are classified on the basis of neutral protease content.22 They found that MCTC had preferential expression of IL-4 and IL-13, suggesting that this subset is capable of regulating IgE, at least locally, through IL-4 “driven” humoral immunity. On the other hand, patients with SAC had low MCT expression of IL-5 and IL-6, consistent with previous reports that show high levels of IL-5 are necessary to activate eosinophils in chronic allergic disease.21
Studies show that there is a correlation between the levels of adhesion molecules and the different types of inflammatory cell infiltrate in allergic eye disease. Adhesion molecules help anchor circulating eosinophils to the endothelium with subsequent extravasation. All types of adhesion molecules (E-selectin, intercellular adhesion molecule (ICAM-1), and VCAM-1) are expressed in increased amounts only in active allergic eye disease, and not, for instance, in out of season SAC.23 There is a positive correlation between ICAM-1 and E-selectin levels and the degree of granulocyte and lymphocyte conjunctival infiltrate, and VCAM-1 expression with eosinophil levels.24 Therefore, the specific pattern of granulocyte and lymphocyte infiltrate is due to the relative concentration rather the selective recruitment of the different adhesion molecules.23 Out of season symptoms in patients with SAC and PAC, which tend to be milder, are associated with an increased number of CD45RO memory cells and EG2-positive cells.25
Human eotaxin-1, otherwise known as CC chemokine ligand 11 (CCL11), and its receptor CCR3, have been shown to be upregulated in tears of individuals with SAC26 and AKC with severe corneal damage,27 and in the mucus of patients with VKC.28 Eotaxin-1 is an important protein in inflammatory conditions because it helps recruit eosinophils to the site of inflammation, leading to their activation,29 and succeeding release of cytokines. Among these is IL-13, whose functions include promoting IgE class switching, regulation of cell-mediated immunity, inhibition of eosinophil apoptosis, and possibly mediation of tissue fibrosis.30 It also targets Th2 lymphocytes and mast cells, promoting the allergen-driven production of IL-4 and IL-5,31 upregulation of adhesion molecules, and persistence of the inflammatory process.
▪ Chronic allergic conjunctivitis
Giant Papillary Conjunctivitis
In 1974, Spring32 reported that 78 of 170 soft contact lens wearers developed an allergic reaction on the upper tarsal conjunctiva, presenting with complaints of contact lens intolerance and excessive mucus production. Allansmith and coworkers33 more definitively described this disorder and called it giant papillary conjunctivitis because of the appearance of papillae in the upper tarsal conjunctiva; these papillae grew larger when the condition remained untreated. Most recently, in 2005, Chang and colleagues found that GPC changes are not limited to the upper tarsal conjunctiva. Patients diagnosed with GPC associated with ocular prosthesis had a honeycomb pattern consistent with giant papillae in both upper and lower tarsal conjunctiva.34
GPC appears to develop as a result of tarsal conjunctival sensitization to environmental allergenic material present on the surface of the contact lens, coupled with the trauma to the upper tarsal conjunctiva associated with the excursion of the eyelid over the soft lens at each blink, an event that occurs about 8000 times each day.2 Irritation secondary to trauma to the tarsal conjunctiva leads to the release of neutrophil chemotactic factor and other inflammatory mediators.35 Scanning electron microscopy studies show that within 8 hours of wear, the contact lens is coated with material composed of mucus, protein, bacteria, cells, cell debris, and air-borne pollutants.36
The chemistry of the contact lens is another important element in the development of GPC, as well as edge design, surface properties, fitting characteristics, and replacement cycle.37 Nevertheless, patients need to be aware that the condition may occur with any type of lens, especially if they are replaced at intervals greater than 3 weeks.
Various inflammatory mediators contribute to the development of GPC. Leukotriene C4 (LTC4), known to be released by eosinophils, is elevated in the tear fluid of these patients. Patients who wear contact lenses have decreased levels of decay-accelerating factor (DAF),38 a complement-activation inhibiting protein, leading to increased inflammation secondary to increased complement upregulation. It is interesting to find higher tear levels of eotaxin in contact lens users,39 previously noted to be increased in SAC, AKC, and VKC. In fact, Maschos found that eotaxin levels were proportional to the severity of GPC, suggesting that this molecule could be involved in the formation of the papilla associated with GPC.
Biopsy of the conjunctival papillae discloses mast cells in the conjunctival epithelium and substantia propria, eosinophils in the same sites, and occasionally basophils in the conjunctival epithelium or substantia propria. Mast cell participation in GPC is substantially greater than would first appear to be the case on the basis of light microscopic observations.2 Ultrastructural studies show many more mast cells than can be observed by light microscopy, with ultrastructural evidence of mast cell degranulation.40 This high content of mast cells correlates with past findings associating GPC with atopy.
The tarsal conjunctiva, overlying the giant papilla, is thickened and irregular, with many indippings to the underlying stroma.1 The epithelium over the atypical portions of the papillae may show localized reduction of the goblet cell population, whereas in the interpapillary crypts, mucus-secreting elements seem to be hyperplastic.41
Vernal Keratoconjunctivitis
The histopathologic and immunopathologic characteristics of the tissues affected with VKC have led some authorities42,43 to conclude that VKC is not a pure type 1 Gell and Coombs hypersensitivity reaction, but rather a combination of both type 1 and type 1V reactions.2 Immunohistochemical studies show that the mononuclear cells are rich in helper (CD4) T cells and that the cytokines produced by the inflammatory cells are, among other things, inducing abnormal expression of class 2 HLA glycoproteins on conjunctival epithelium and stromal cells.42 In these CD4 areas of VKC biopsies, there is an increased level of IL-5, but not of IL-2, confirming Th2 rather than Th1 influence.44 Recent studies also reveal an increased expression of adhesion molecules. These promote the recruitment of inflammatory cells as well as the interaction between lymphocytes, antigen-presenting cells, and epithelial cells.45
The histopathology of the conjunctival papillae discloses not only the cells typically associated with allergic reactions (mast cells and eosinophils), but also large collections of mononuclear cells, fibroblasts, and newly secreted collagen, leading to the characteristic conjunctival findings.2 Leukotrienes may be largely responsible for chemosis, conjunctival injection, and increased mucus secretions seen in VKC. They may induce conjunctival vasodilation, edema, hyperemia, and epithelial gland glycoprotein secretion.46–48
Current research proposes that eosinophil cationic protein (ECP), released by eosinophils, is influential in the pathogenesis of palpebral VKC. Pucci and colleagues49 observed a direct correlation between the number and size of giant tarsal papillae and ECP serum levels. They postulate that serum ECP is a reliable marker of disease activity in patients with palpebral and mixed VKC. On the other hand, patients with bulbar VKC had lower ECP and total IgE serum concentrations, suggesting “IgE sensitization is a predisposing factor for tarsal rather than limbal VKC.”49
Another constituent of eosinophil granules is major basic protein (MBP). At high levels, MBP can be cytotoxic,50 whereas at lower concentrations it contributes to histamine release from mast cells.51 Extracellular deposition of MBP has been observed in VKC, AKC, and GPC,52–54 leading to neutrophil activation and tissue injury through the release of lysosomal enzymes, neutrophil oxidase, and superoxide anion.55
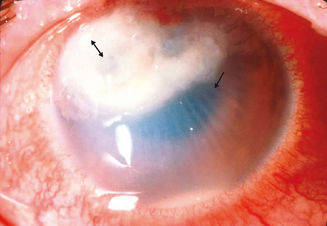
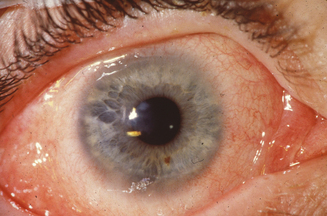
The limbal form of VKC was first described by Arlt56 in 1846, predating the description by von Graefe57 of the palpebral form by 25 years. This form is characterized by the presence of large papillae in the conjunctiva at the corneoscleral limbus, with associated collections of inflammatory cells rich in eosinophils at the apices of the limbal papillae, the so-called Horner–Trantas dots.2 In especially severe forms of limbal VKC, the steady accumulation of inflammatory cells may result in formation of a frank mound on the peripheral cornea (Figure 6.4). This complex immunologic process seems to be coordinated with the help of the chemokine receptor CXCR3, reported to predominate in this type of disorder.58
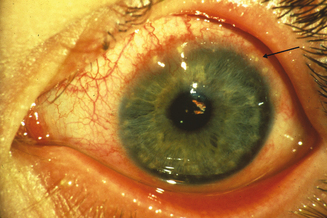
Figure 6.4 Limbal vernal keratoconjunctivitis. Note the white-opaque perilimbal Horner–Trantas dots (arrow).
Conjunctival remodeling in VKC is characterized by epithelial hyperplasia, angiogenesis, and deposition of extracellular matrix components in the substantia propia.59,60 Abu El-Asrar et al61 ascertained significant overexpression of α3– and α6-integrin subunits, epidermal growth factor (EGFR), vascular endothelial growth factor (VEGF), transforming growth factor beta (TGF-β), basic fibroblast growth factor (bFGF), and platelet derived growth factor (PDGF) in VKC lesions. Abnormal keratinocyte deposition has been associated with suprabasal integrin expression.62 TGF-β, bFGF, and PDGF stimulate fibroblast proliferation, while VEGF influences angiogenesis and vascular permeability.63–65 Taken together, it is not surprising to find such profound conjunctival alterations in this disease.
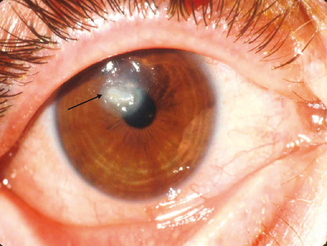
The keratopathy of vernal keratoconjunctivitis typically begins as a diffuse superficial punctate keratitis. If the inflammation continues with an outpouring of inflammatory mediators, especially those from eosinophils, into the tear film and with associated epithelial toxicity and possibly conspiracy from the mechanical effects of the large papillae, a frank epithelial defect appears next.2 These defects have been termed shield ulcers because of their position and morphology (Figure 6.5). They are present in approximately 3–11% of patients with VKC.6 Epithelial defects are trophic, defying the therapeutic strategies that usually are successful in healing corneal abrasions or epithelial defects. The longer such trophic defects persist, the higher is the likelihood of eventual stromal ulceration, secondary microbial infestation, and permanent corneal scarring (Figure 6.6). In chronic advanced cases, the inflammatory material is deposited in the form of opaque white or yellow “plaque.”1
Failure of corneal ulcer or plaque re-epithelialization may be attributed to the overexpression of matrix metalloproteinases (MMPs) by resident corneal cells,66 as well as to deposition of MBP at the ulcers.52 Corneal sensitivity, tear film break-up time (BUT) values, and MUC5AC mRNA expression was significantly lower in atopic patients with corneal ulcers, as reported by Dogru et al.67 It should be noted that MUC5AC is part of the mucinous component of the tear film, promoting tear adhesion to the corneal surface. They believe there is an inverse relationship between MUC5AC expression and the degree of ocular surface inflammation in atopic eyes with allergy.
At a molecular level, corneal damage in VKC may result from various sources. The extracellular matrix is an important component of tissue remodeling. Matrix metalloproteinases (MMPs), mediators of collagen degradation and inflammatory cell migration, and tissue inhibitors of MMPs (TIMP), have to be in equilibrium in order to achieve normal corneal healing. Leonardi68 found increased tear levels and activity of MMP-1 and -9 in patients with VKC, leading to altered homeostasis and tissue damage. In fact, they found a direct relationship between MMP-9 activity and clinical findings, including corneal involvement and giant papillae formation. MMP-1, also known as collagenase, is activated by mast cell chymase.69 Ebihara et al70 observed increased levels of chymase in the tears of VKC patients, further substantiating Leonardi’s findings.
Atopic Keratoconjunctivitis
Atopic keratoconjunctivitis was defined by Hogan10 in 1952 as allergic keratoconjunctivitis occurring in association with atopic dermatitis (eczema). This definition, although imprecise, is in common usage and connotes the patients with the most severe form of atopic ocular disease seen in association with eczema.2 The argument by some physicians that other types of atopic conjunctivitis, such as chronic allergic conjunctivitis or perennial atopic conjunctivitis, also are atopic ocular diseases and therefore can be confused with atopic keratoconjunctivitis is not a constructive one. This is particularly true in view of the fact that in those latter disorders, keratitis or significant keratopathy is not part of the clinical picture. Corneal disease is, however, typical of patients with atopic keratoconjunctivitis.2
Ocular surface disease in patients with atopic dermatitis is characterized by decreased goblet cells and conjunctival squamous metaplasia, which seem to worsen with increased number of flare-ups.67 Reduced goblet cell counts contribute to tear instability by limiting the secretion of mucin, specifically MUC5AC,71 a phenomena present in VKC also.
Atopic individuals have a defect in suppressor T cells responsible for regulating IgE production to antigens, in addition to other genetically governed abnormalities which set the stage for atopic or inappropriate responses to environmental allergens.1 Type 1 hypersensitivity is only one of the mechanisms in the pathogenesis of AKC, in fact it is widely accepted that Th2 cells play an important role as well. Some of the immunopathologic characteristics of AKC specimens are similar to those of cicatricial pemphigoid and ocular rosacea, emphasizing that fibroblast activation, proliferation, and production of cicatrization may result from a variety of chronic conjunctival inflammatory disorders in which T cells, macrophages, and mast cells collaborate.72 Matsuura et al corroborated the systemic predilection towards a type 2 immune response and the associated infiltration of type 2 T cells into the local ocular site, without undermining the presence of type 1 T cells in chronic allergic inflammation.73 Another mechanism by which Th2 cells may predominate in atopic disease is through preferential apoptosis of their counterpart, Th1 cells.74
Recent studies focus on the characterization of Th1 and Th2 cytokines in chronic ocular allergy. Leonardi75 detected IL-4 and interferon gamma (IFN-γ) in tears of individuals with AKC, but found that only IFN-γ levels correlated with disease activity, specifically with corneal involvement. Upregulated IFN-γ levels seemed to go in hand with increased expression of ICAM-1 on conjunctival fibroblasts and the secretion of IL-6 and IL-8.75 In 2005, Okada et al76 contributed to Leonardi’s hypothesis. They noticed that when activated by IL-4 and TNF-α, corneal fibroblasts expressed ICAM-1 and VCAM-1 and increased eotaxin production, all leading to continued eosinophil adhesion to these molecules and persistent allergic keratopathy.
Perforin is a plasma membrane protein that plays an essential role in T-cell cytotoxicity. Ambach and colleagues77 demonstrated that atopic patients have a reduced number of perforin-containing CD8+ cytotoxic lymphocytes, leading us to conclude that this is one of the many mechanisms by which these individuals are likely to develop inflammation.
The histopathologic findings of the conjunctiva of patients with AKC are characterized by mast cell and eosinophil invasion of the epithelium, epithelial pseudotubule formation, and increased goblet cell presence.1 Mast cells and eosinophils along with a chronic mononuclear cell infiltration are also prominent in the substantia propria.72 Conjunctival biopsies reveal high mRNA levels of IL-3, IL-4, and IL-5.78 Patients with VKC or AKC have higher levels of conjunctival IL-4 producing CD4+ T cells than patients with acute allergic conjunctivitis.73
Giant papillary formation is essential in the pathogenesis of AKC, as well as in VKC. Conjunctival histopathologic examination of the excised papillae shows elevated number of goblet cells, inflammatory leukocytes, and fibrotic tissue, along with evidence of angiogenesis.79,80 Asano-Kato81 showed increased production of VEGF by conjunctival fibroblasts when stimulated by Th2 cytokines, TGF-β1, and IL-1β. These findings led to the conclusion that conjunctival fibroblasts may be influential in exacerbating inflammation and tissue remodeling, paving the way towards papillary formation.81
Yamagami and coworkers evaluated the tarsal conjunctival giant papillae which are typically seen in patients with AKC and atopic dermatitis and/or asthma.82 They found that the predominant chemokine receptor genes were CXCR4 and CCR4. Giant papillae showed increased IL-4 and IL-13 levels in association with high CCR4 gene expression. Eotaxin and its receptor, CCR3, were also detected, but at lower levels. These findings are relevant to atopic disease because CC-receptors are important for eosinophil migration.83
Diagnosis
▪ Acute Allergic Conjunctivitis
Physical Examination
Signs of ocular inflammation, even during a time of maximal symptoms, usually are unimpressive. The eye may not be obviously inflamed. Indeed, the conjunctiva may appear totally white and quiet.2 Further inspection by slit lamp biomicroscopy, however, often reveals mild edema of the bulbar conjunctiva and signs of inflammation in both upper and lower tarsal conjunctiva (Figure 6.7). The conjunctivae are usually mildly injected and edematous leading to a “milky” appearance. Increased mucus is frequently observed in the preocular tear film and in the inferior fornix. Fine papillary hypertrophy of the upper tarsal conjunctiva may occur.84 Additionally venous congestion in the skin of the lids can cause the appearance of dark circles around the eyes termed “allergic shiner.” Many individuals also have concurrent nasal symptoms.85 The cornea is characteristically unaffected, an important sign which differentiates acute allergic conjunctivitis from the chronic forms, which usually involve corneal alterations.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree