Chapter 10 Management of the Patient with Laryngitis
Introduction
Dysphonia is a problem that afflicts millions of people on an annual basis.1 Its impact on quality of life varies from patient to patient depending upon the underlying laryngeal abnormality and whether the voice difficulties are episodic or chronic. The literature base is replete with research on many different benign and malignant causes of dysphonia. However, the possible role of allergy in the pathogenesis and expression of vocal pathologies has not been extensively investigated, despite the fact that allergic diseases of both the upper and lower respiratory subsystems are among the most prevalent illnesses regularly treated by physicians throughout the world.
Inasmuch as the larynx is an integral component of the unified airway,2,3 it is not unreasonable to suggest that it is as susceptible as other juxtaposed respiratory structures to the development of adverse allergy manifestations. The sparse data base on the potential causal relationship between allergy and vocal pathologies provides a rich opportunity for theoretical discussions and seminal research on this subject. Prospective outcomes of these endeavors may prove valuable to medical and health science practitioners from various subspecialties who frequently evaluate and manage patients with allergies.
Unified Airway
Both Hurwitz2 and Grossman3 discussed the frequent coexistence of upstream and downstream respiratory tract inflammatory conditions, including transient and chronic laryngopharyngeal involvement. More recently, deBenedictis and Bush demonstrated that these allergic manifestations represent a continuum of inflammation throughout this integrated tract of respiratory organs.4 They further suggested that arbitrary separation of the airway into upper and lower subdivisions ignores the inherent anatomic and physiological coupling of this single integrated system.
A considerable amount of research has been conducted in the past couple of decades focusing on the possible causal interrelationships between sinusitis, rhinitis, and lower respiratory tract functional abnormalities.5–10 These investigators have reported that as much as 90% of all patients with asthma also suffer from rhinosinusitis; and that approximately 25% of those with allergic rhinitis experience occasional hyperreactive lower respiratory tract symptoms, such as pulmonary congestion, shortness of breath, spasmodic coughing, and throat clearing due to perceptions of excessive endolaryngeal mucous accumulation. These findings have bolstered support for the model of a unified airway; one common system of organ linkages that is subject to widespread, simultaneous, and reactive (i.e., delayed) allergic manifestations. To date, debate continues within the clinical and scientific communities regarding how these allergy-induced interrelationships are driven. Additionally, the specific role of the phonation subsystem in this inflammatory loop remains unclear, particularly with respect to whether it assumes a largely passive or reactive role, or whether its phylogenetic anatomic position enforces a physiologically more active and integrative role during times of allergic and nonallergic common airway inflammation.11
Phonation Subsystem Anatomy and Physiology
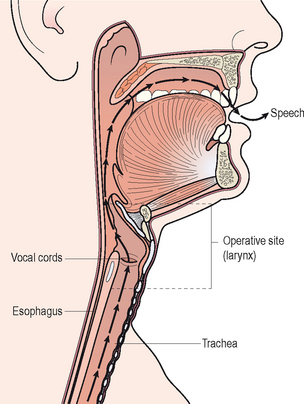
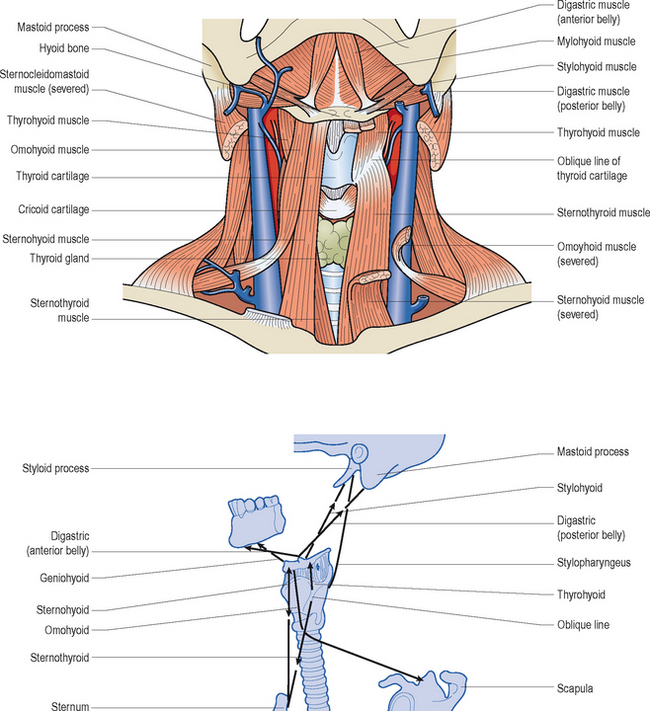
All mammals possess a larynx. Figure 10.1 illustrates that this complex organ is a component of the upper airway and it is suspended in the anterior neck by a sling of extrinsic muscles, ligaments, and specialized joints in the approximate vicinity of the fourth, fifth, and sixth cervical vertebrae. It functions as a biologic valve for: (1) breathing, (2) airway protection during swallowing, (3) coughing to help clear bodily secretions and any foreign particles from the tracheobronchial tree and endolarynx, (4) bowel evacuation, (5) heavy lifting, and (6) childbirth. These functions occur involuntarily or reflexively. The vocal folds within the larynx, in concert with downstream expiratory efforts, can also be voluntarily recruited to vibrate and produce vocalizations known as voice. Over the course of early childhood, humans learn how to coordinate respiratory airflow dynamics, biomechanical vocal fold activities, and upstream articulatory adjustments for the purposes of generating various speech sounds to communicate their thoughts and wishes.
▪ Laryngeal Skeleton
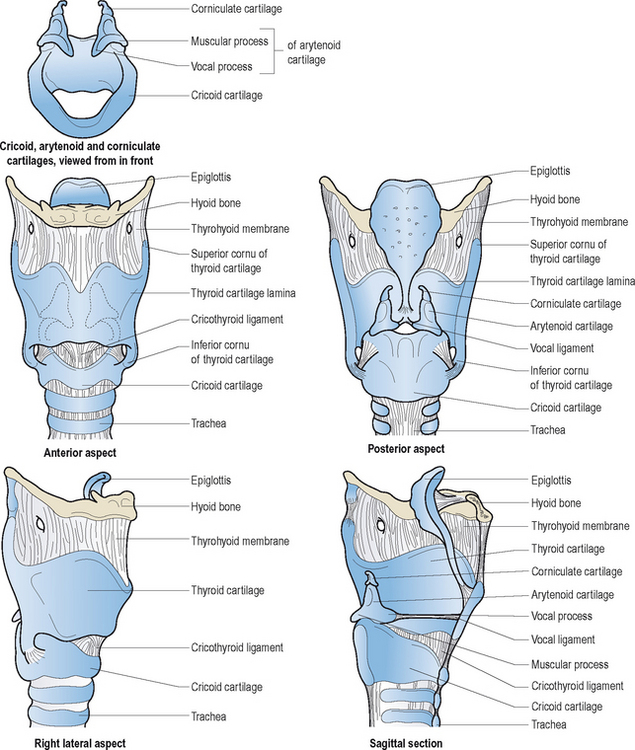
The larynx is composed of three pairs of small cartilages (arytenoid, corniculate, cuneiform) and three large unpaired cartilages (thyroid, cricoid, epiglottis). Figure 10.2 illustrates these structures and their interconnecting membranes and ligaments. The trachea directly links the larynx with the lungs. There are two synovial articulations or laryngeal joints: cricothyroid and cricoarytenoid. Hinge-like action of the former paired joints increases the anteroposterior length of the vocal folds. This adjustment results in increased tension and reduced cross-sectional mass of these structures; most notably influential during pitch variations in speech and song. The primary action of the latter joints is rocking motion of the arytenoids; anteromedial action is of paramount importance for vocal fold adduction, and posterolateral action is essential for vocal fold abduction. There is little evidence in the scientific literature to support classic textbook descriptions of rotary and gliding motions of the arytenoid cartilages during voice production or other valving activities.
▪ Laryngeal Muscles
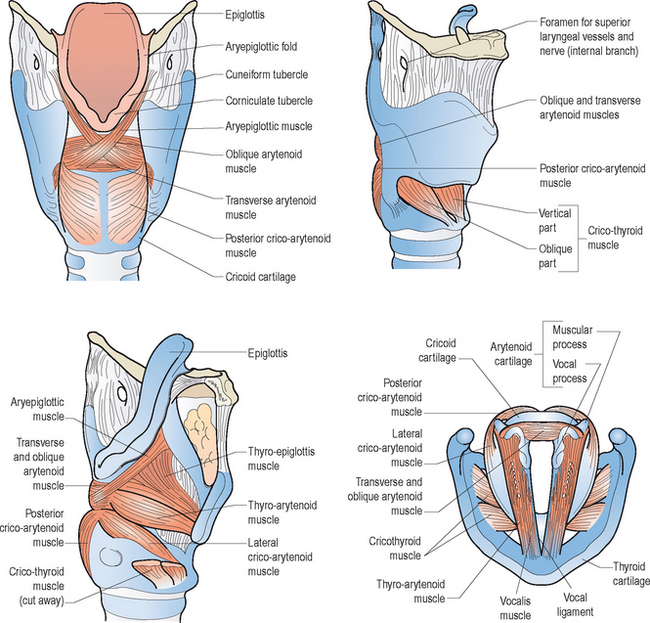
Figures 10.3 and 10.4 illustrate the various intrinsic and extrinsic muscles of the larynx, respectively. Suffice it to say that the true vocal folds arise from or are components of the thyroarytenoid muscle bundles. The intrinsic group of muscles work harmoniously to open, close, tense, and relax the vocal folds during breathing, swallowing, and speaking. Although this entire group probably works in a coordinated and collective manner to achieve these movements; for ease of review, specific functions can be attributed to individual components. That is, contractions of the thyroarytenoid, lateral cricoarytenoid, and interarytenoid muscles generally contribute to vocal fold adduction. As noted earlier, the cricothyroid muscles chiefly lengthen and tense the vocal folds, which decreases their cross-sectional mass. Posterior cricoarytenoid muscle contractions are critical for vocal fold abduction, associated with deep breaths and cessation of vibrations during running speech to accommodate the demands of voiceless consonant production and to terminate voicing at the completion of an utterance.
▪ The Vocal Folds
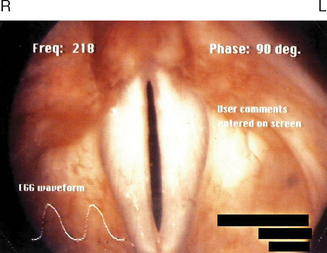
Figure 10.5 demonstrates the normally white and glistening appearances of the true vocal folds within the framework of the thyroid cartilage. The space between the vocal folds is called the glottis, and it varies in its anterior and posterior dimensions during various biological and phonatory behaviors. The vocal folds consist: of (1) an outermost layer of mucosa and stratified, nonkeratinizing squamous epithelium, known as the cover, and (2) deeper layers, which contain the aforementioned thyroarytenoid muscle fibers, as well as high density fibroblasts and elastic and collagenous tissues. Immediately deep to the cover there exists a potential space known as Reinke’s area, which consists mainly of amorphous material with few fibroblasts or elastic tissue. Later in the chapter, we will discuss the biomolecular make-up of the endolarynx and true vocal folds, particularly as it pertains to the presence or absence of mast cells and eosinophils, which normally mediate allergic inflammation in other components of the respiratory subsystem.
Hirano described the cover-body concept of vocal fold vibration.12 His elaborate explanations more than 30 years ago have been instrumental in the development of modern phonosurgical procedures for benign vocal fold pathologies. Because Reinke’s space possesses a gelatinous consistency, it enables fluid vibratory motion of the cover over the vocal fold body (thyroarytenoid muscle fibers) during phonation. Detailed appraisal of such activity can be achieved in the clinical setting using laryngovideostroboscopy. This quasi-slow motion imaging technique reveals traveling waves of mucosa from the inferior to superior surface of the vocal folds. Scarred or fibrotic vocal folds, as a result of invasive benign or malignant pathologies, do not produce normal mucosal waves.
▪ Peripheral Laryngeal Innervation
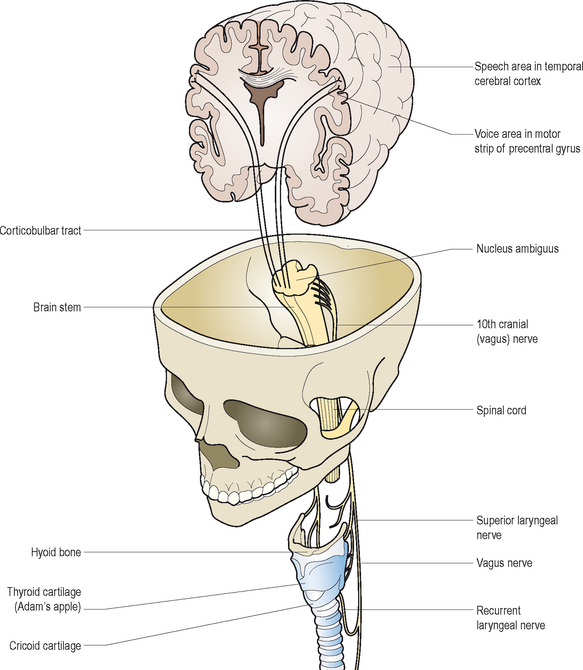
Volitional voice production depends upon a complex loop of neural interactions between the central nervous system, peripheral nervous system, and various respiratory and speech musculature. Kotby et al13 described a six-level hierarchy of laryngeal neuromuscular integration. Of these interrelated segments, the higher levels generally function to activate, inhibit, and modulate output of the lower levels for purposeful voice production. Some of the lower level activities are organized into reflex pathways. Based on a top-down model of control, conceptual programming of speech and voice occurs at the highest level. At the cerebellar level below, movement adjustments are coordinated, and errors are detected and corrected for accurate performance. The pyramidal or upper motor neuron system serves the next level of function as the primary initiator of all muscular contractions through synapses with motor nuclei of all cranial and spinal nerves normally involved in speech production. The extrapyramidal level functions as an ongoing, automatic and subconscious regulator of all sensorimotor outputs and underlying muscle tone, via complex loop circuitry between the central and peripheral nervous system. The vestibular–reticular level helps to activate and regulate motor inputs to and sensory outputs from the cranial and spinal nerves (lower motor neurons) and the muscles responsible for speech and voice production. The lower motor neurons represent the lowest level of this integrated system. They form motor units within the muscle tissues they innervate to stimulate muscle contractions for volitional movement purposes.
The vagus or Xth cranial nerve pair arise from the medulla on the brain stem. They descend into the neck through the jugular foramen, and distribute three primary branches that help control and regulate voice and speech activities: (1) pharyngeal nerve, (2) superior laryngeal nerve, and (3) recurrent laryngeal nerve. The first of these branches provides nerve fibers to the pharynx and most of the soft palate. The second branch contains an internal and external laryngeal nerve component. The former one enters the larynx and divides into two additional branches, both of which contain sensory fibers from the mucous membranes that line the endolarynx above the vocal folds, and from neighboring muscles’ spindles and stretch receptors. The external branch is the chief motor nerve supply of the cricothyroid (pitch changing) muscle and inferior constrictor muscles of the pharynx. The recurrent laryngeal nerve or third primary branch of the vagus nerve, descends past the larynx and then loops back up to provide motor innervation to all of the other intrinsic laryngeal muscles. Whereas the right recurrent nerve loops under the ipsilateral subclavian artery en route to the larynx, the left one descends more inferiorly in the chest, deep to and winding under the arch of the aorta, before it ascends in the tracheoesophageal groove to enter the larynx behind the cricothyroid joint on either side. In addition to its widespread motor inputs, it supplies sensory filaments to the mucous membranes within the lining of the subglottis, immediately below the vocal folds. These fibers transmit afferent output from these tissues as well as stretch receptors in the surrounding musculature.
Mechanoreceptors mediated by the recurrent and superior laryngeal nerves are abundantly located within the mucosal lining, muscles, and joints of the larynx. These sensory elements influence respiratory and vegetative reflexes, and they contribute to what may be termed the intrinsic laryngeal monitoring system, as they relay oscillating discharges to the lower brain stem in response to air pressure fluctuations that occur during voice production. Polysynaptic loops are then formed with the motor neuron pools of the vagus nerve at this level to establish the so-called tonic servo-reflex system of the larynx.14 Figure 10.6 offers a schematic representation of these hierarchical neurologic pathways associated with voice production. For more detailed reviews of the neurologic substrates of phonation, the reader is referred to other sources.15,16
▪ Voice Production
As shown in Figure 10.1, vocal fold vibrations during speech efforts send a traveling wave of acoustic energy upstream through the vocal tract. This pathway, which includes the oral and nasal cavities, acts as a resonating chamber to enhance, absorb, and reflect the sounds generated into distinctive voice qualities. The infraglottal tract consists of the respiratory musculature, lungs, trachea, and immediate subglottis. These structures function as a collective power source for phonation by providing ongoing airflow dynamics required to drive vocal fold vibrations during speech efforts. The vibratory activity itself is largely a passive act. That is to say, at the start of a vibratory cycle the vocal folds are volitionally preset in an adducted position at the midline of the glottis. Assuming the lungs have been supplied with a sufficient amount of inspired air in preparation for speech, pressure increases within the trachea with expiratory effort to generate upstream airflow to induce vocal fold vibrations and voice. When subglottic pressure exceeds the level of resistance created by the adducted vocal folds, a puff of air is emitted into the vocal tract. This momentary break in the glottal seal initiates the vacuumous Bernoulli effect. This aerodynamic phenomenon results from increases in the velocity of air molecules passing through the narrow glottic inlet. As this occurs, air pressure between the vocal folds decreases, which, in turn, induces glottic closure to complete the vibratory cycle (closed–open–closed). This wave is assisted by intrinsic laryngeal myoelastic properties. Sustained phonation depends upon adequate intrinsic laryngeal muscle and elastic glottal closing forces, and sufficient and continuous infraglottal airflow support to initiate and drive vocal fold vibrations.
▪ Parameters of Voice
Quality, loudness, and pitch are the primary parameters of human voice. Quality represents the overall timbre or pleasantness of voice. The rhythm and symmetry of vocal fold vibrations, and the adequacy of glottal closure, significantly influences vocal quality. Irregular motion and glottal incompetence during the closed phases of vibration usually result in escapes of unphonated air, which distorts the voice signal. Hoarse, harsh, raspy, breathy, wet-gurgly, spasmodic, and tremorous, are common terms used to classify vocal quality disorders. The speech diagnostic terms hyponasality and hypernasality are sometimes used within this context of vocal quality disturbances. However, these disorders result from upstream velopharyngeal and nasal cavity disturbances.
Evaluating the Allergic Patient with Voice Complaints
▪ Team Approach
A team approach to the evaluation and treatment of patients with suspected laryngeal allergic sequelae is usually most successful. Members in this effort should minimally include an allergy physician with a background in otolaryngology or immunology, a speech-language pathologist with expertise in the area of vocal pathologies, and a nurse practitioner. The diagnosis of chronic allergic laryngitis should be considered for patients who present with histories of upper respiratory allergies and co-occurring phonation subsystem disturbances, such as globus sensations, excessive laryngeal mucus and reactive throat clearing and coughing behaviors, dry-itchy throat, and voice difficulties. With this clinical population, the history component of the examination usually produces the most indispensable diagnostic data. In this vein, the exploration of antecedent events or triggers of allergy symptoms almost always proves to be of paramount importance to accurate diagnoses, as does the time course or seasonality of such complaints. Whether the patient suffers from any co-occurring diseases, such as asthma, otitis media, sinusitis, and chronic acid reflux, should be evaluated because these conditions can exacerbate the underlying allergy. Prior or current use of medical or complementary therapies to treat these problems should be factored into the differential diagnostic and subsequent management equations.
In the following segment of the chapter commonly employed qualitative and quantitative phonation subsystem evaluation techniques are described in detail. Most of the procedures discussed are not routinely performed by physicians, unless they have undergone training in the area of otolaryngology, or they have worked closely with medical colleagues or speech-language pathologists with such expertise. Notwithstanding this limitation, it is not unfeasible to suggest that virtually all of the techniques below can be easily learned by the inquiring and determined physician, regardless of his or her medical subspecialty background. Those clinicians who prefer to send the dysphonic patient to a laryngologist should, at the very least, achieve a working knowledge of the rationale for and diagnostic benefits of all of these testing procedures. Acquiring this understanding will foster communication with the practitioners to whom the patient is referred, and such information will facilitate comprehensive diagnostic and treatment discussions.
▪ History of the Dysphonia and Initial Examiner Impressions
The origin and course of abnormal voice signs and symptoms are of vital importance to differential diagnosis and management. Initially, the examiner should render a perceptual impression of the overall severity of dysphonia that the patient exhibits during the history-taking process. The types of underlying disturbances in vocal quality, pitch, and loudness should be noted, and each perceived difficulty should be behaviorally defined and rated with respect to degree of impairment. Box 10.1 provides a rating form that may prove helpful for such purposes.
The examiner should employ a logical sequence of questions to evaluate the background of the problem. First, questions regarding how long the dysphonia has existed, and whether it varies in degree from day to day, should be asked. If there is a previous history of dysphonia, ascertain what types of treatments may have been rendered in the past to improve the problem. Second, the examiner should note whether the dysphonia characteristics vary during the interview. Third, whether the patient has determined the possible cause, or can link the voice difficulties to specific times or events, are important factors that must be explored. For example, has there been a recent exacerbation of allergic symptomatology that might account for the voice difficulty, owing to significantly associated coughing or throat clearing behaviors, which may have resulted in vocal fold trauma. Fourth, the patient should be asked whether the difficulty has improved at all since the onset. If so, it would be important to inquire as to what such improvement might be attributed. Fifth, if the patient reports that there are times in the day when the voice is better or worse, these fluctuating abilities should be discussed to try to determine possible causal conditions. Sixth, the astute examiner should always ask whether there have been days since the onset of dysphonia when the voice was completely normal for long periods of time. Seventh, it is essential to rule out significant comorbid medical problems for which the allergic patient may have been treated, and to which the dysphonia may be fully or partially attributed. For example, recent intubation anesthesia, laryngeal trauma, thyroid or neurologic disease, illness, or injury, and severe laryngopharyngeal reflux should be considered as possible causes, either acting alone or in combination with the allergy history. Eighth, determine if the patient abuses the vocal folds; excessive throat clearing, coughing, yelling, smoking, limited water intake and substantial consumption of diuretic beverages, regular use of inhaled corticosteroids, and routine use of decongestant medications are prime examples of behaviors that can provoke vocal fold swellings and generalized signs and symptoms of laryngitis. Ninth, inquire as to whether the patient is suffering from any type of swallowing difficulty. A significant degree of laryngitis can cause odynophagia and glottal incompetence, which can result in aspiration symptoms. Aspiration usually elicits coughing reactions. Coughing can exacerbate existing laryngeal swellings, which increase the swallowing difficulties. This vicious cycle is not uncommon, and it needs to be broken to restore nutritional balance and relieve the patient of potentially deleterious pulmonary side effects. Tenth, if the patient sounds stridorous at rest, during exertion, or both, auscultation of the upper airway with a stethoscope on the larynx to confirm the possible presence of laryngeal airflow difficulty can be diagnostically valuable. Stridor is usually associated with anatomic or physiological glottal obstruction, as may occur with severe vocal fold swellings, large ball-valving glottic or subglottic lesions or stenosis, or bilateral abductor vocal fold paralysis. Stridor may act alone to cause dyspnea, or it may occur in combination with downstream (e.g., asthma; COPD) or upstream (e.g., allergic rhinitis; rhinosinusitis) airway diseases. Table 10.1 provides a synopsis of these steps for easy reference.
TABLE 10.1 Exploring the history of dysphonia
| Examination steps | Objectives |
|---|---|
The initial impressions rendered by the examiner, and answers to the various questions posed to the patient, provide indispensable data ultimately required to formulate a differential diagnosis of the dysphonia and a possible treatment plan for this specific problem. Acute onset dysphonia can usually be tracked to a specific recent event, injury, or illness. Profound yelling at a ballgame, prolonged intubation during a surgical procedure, direct laryngeal trauma in an accident, laryngeal anaphylaxis or non-IgE-mediated allergic laryngitis secondary to substantial antigen exposure, neck or thoracic surgery that normally places the recurrent laryngeal nerve at risk for either stretch neurapraxia or resection injury, repetitive intubation-extubation abrasion of the vocal folds, stroke, Guillain–Barré syndrome, and closed head injury are some of the most common potential etiologies of sudden voice difficulties. Not infrequently, if the resultant laryngeal abnormality causes significant glottal incompetency, the patient may also suffer from aspiration symptoms and a more complicated clinical course. The prognosis for spontaneous recovery of normal voice within a relatively short period of time without phonation subsystem medical intervention largely depends upon the underlying etiology of the acute dysphonia.
▪ Voice Sampling
Contextual speech and voice characteristics will be automatically obtained during the history-taking process. In addition to the collection of these important data, the examiner should request the patient to perform specific tasks. First, instruct the patient to take a deep breath and then prolong the vowel /a/ for as long and steady as possible. This maximum phonation time (MPT) task is usually measured in seconds, and the patient’s mean performance over two trials should be calculated and encircled on the aforementioned rating form (Box 10.1). Normally, adults should be able to generate at least 14 seconds of MPT; children can usually normally sustain voice for at least 10 seconds. Abnormal performance is often attributable to glottal incompetence and consequential air wastage during the phonatory effort. Downstream pulmonary system limitations may also cause reduced MPT, owing to insufficient vital capacity or forced expiratory volume, as may occur in the asthmatic patient. Second, ask the patient to sing up and down a musical scale at his or her most comfortable pitch level. Assess the number of notes that can be sung, as well as the associated voice features throughout the task. Patients with dysphonia often exhibit difficulty raising or lowering pitch from their habitual level, because this activity requires finite vocal fold stretching and relaxing adjustments, respectively. Swellings or lesions involving these structures typically restrict their flexibility and cause pitch production limitations, along with disturbed quality and volume parameters. Third, ask the patient to cough sharply to assess the force of glottal closure during this abrupt vocal fold behavior. Significantly weak or breathy coughing often signifies glottal incompetence, and usually strongly correlates with the dysphonia characteristics. Patients who cannot generate volitionally adequate coughing activity, regardless of the cause, may be at risk for aspiration and pulmonary infection because physiological integrity of the glottal valve is of paramount biologic importance during swallowing and tracheobronchial mucus clearing.
▪ Voice Symptom Questionnaire
Box 10.2 is a questionnaire that can be used to determine the extent to which a patient exhibits and experiences specific signs and symptoms that collectively may be manifestations of allergy and causally related to vocal fold abuses and voice difficulties.