CHAPTER 27 Management of Aging Skin
Aging skin is one of the primary characteristics of the aging face that must be addressed as a part of comprehensive facial rejuvenation. Proper skin care regimens can be started at an early age in order to decrease the amount of photoaging, dyschromias, and superficial scarring that a person accumulates over time. Even though these preventive measures are becoming more commonplace, there are still many patients who seek treatment of their aging skin in order to “reverse” this process. This chapter focuses mainly on the resurfacing techniques available to treat advanced skin damage. Chemical peels and laser ablative techniques have been proven to produce substantial results in a consistent manner. We will also discuss emerging trends including nonablative laser therapy and fractionated ablative laser therapy. Other topics including dermabrasion and medical skin care regimens will also be addressed. Each of these techniques alone can produce predictable results in selective patients. However, it has been our experience that combined modalities tailored to skin type and location can be most effective.1
Histologic Changes of Aging Skin
The first scholarly report on phenol chemical peels was written by Brown and others.2 Brown described the histologic changes that were induced including laminated collagen in the epidermis, with fibrous strands consistently paralleling the newly formed epidermis. Later, Kligman and colleagues3 studied the skin taken from Baker and Gordon’s facelift patients who had chemical peels  to 20 years earlier. First, they described histologic changes of nonpeeled skin. These aging skin changes were typical of actinic exposure with a loss of orderly differentiation in the epidermis and degeneration of the elastic network, along with some mottled pigmentation and lymphocytic infiltration. There was a decrease in collagen amounts as well as disordered degeneration of the dermal fibers, a flattening of the dermal-epidermal junction, and multiple actinic keratoses with atypia. The number of melanocytes was increased in this actinic skin, but they were unevenly distributed and contained variable amounts of melanin.
to 20 years earlier. First, they described histologic changes of nonpeeled skin. These aging skin changes were typical of actinic exposure with a loss of orderly differentiation in the epidermis and degeneration of the elastic network, along with some mottled pigmentation and lymphocytic infiltration. There was a decrease in collagen amounts as well as disordered degeneration of the dermal fibers, a flattening of the dermal-epidermal junction, and multiple actinic keratoses with atypia. The number of melanocytes was increased in this actinic skin, but they were unevenly distributed and contained variable amounts of melanin.
The skin of patients who had undergone a previous chemical peel showed a new band of dermis 2 to 3 mm thick just beneath the epidermis and lying on top of the old elastotic dermis. The epidermis had returned to orderly cellular differentiation without irregularities or microscopic actinic keratoses. Although there was an abundance of melanocytes present containing some fine, evenly distributed melanin granules, there appeared to be impaired melanin synthesis with a generalized bleaching effect, or hypopigmentation. Lentigines were not seen. Furthermore, the epidermal-dermal matrix was composed of thin, compact, parallel collagen bundles arranged horizontally in contrast to the usual wavy pattern. Elastotic fibers had actually regenerated, forming a network of fibers paralleling the new collagen. Finally, the lymphocytic infiltration was diminished compared with that of untreated skin. Kligman and colleagues3 believed that the dermal reconstruction lasted about 20 years based on their study. They further concluded that chemical peel reduced the development of new neoplasms. The laying down of a band of new connective tissue can adequately account for the effacement of the wrinkles seen clinically. The skin is smoother, fuller, and tighter. Stegman4 and Litton and colleagues5,6 showed the chemical peel solution penetrating deeper in the dermis of actinically damaged skin than nonactinically damaged skin. Hayes and Stambaugh7 demonstrated that during the first 2 to 5 days of a chemical peel there is epidermal necrosis, edema, and homogenization with the lymphocytic infiltration all the way into the reticular dermis.8 At 2 weeks, new collagen formation had begun. Stegman,4 Alt,9 and Brody and Alt10 have illustrated that there is deeper penetration of phenol with occlusion than with nonocclusion. According to Beeson and McCollough,11 this is apparently true but not necessarily desired.
Litton and others6 agreed with Kligman and colleagues3 that the rate of appearance with precancerous and early cancerous lesions of photoaged skin was decreased after a phenol chemical peel.
Brodland and Roenigk12 showed that trichloroacetic acid (TCA) destroys the epidermis and upper dermis and further showed that the new epidermis migrated from the cutaneous adnexa beneath the destroyed tissue. This is similar to phenol peel. Histologically, the atypical clones of keratinocytes are removed and replaced by normal epidermal cells.
Patient Evaluation, Classification, and Selection
The process or technique of chemical peels (and other resurfacing modalities) is relatively easy to learn. However, it takes a great deal of experience with many different types of patients to learn the wide variation in skin types and how these respond to peel solutions.13 It also takes a great deal of experience to predict the way in which each area of the face will respond to light or deep resurfacing in an individual patient, and how one can influence the method of application used. Careful selection of the appropriate patients for resurfacing is the first and most important consideration. According to McCollough and Hillman,14 “The ideal patient is a thin-skinned female with fair complexion and fine rhytids.”
Fitzpatrick15 described types of actinically damaged skin ranging from type I to type VI (Table 27-1). Brody16 stated that Fitzpatrick types I through III patients are suitable for a chemical peel. He describes the ideal patient as a light-complected person of Celtic or Northern European descent with skin types I or II.17
Table 27-1 Fitzpatrick Sun-Reactive Skin Types I to VI
| Type I | Fair-skinned, blue or hazel eyes, blond or red hair |
| Always burns, never tans | |
| Type II | Fair-skinned; blond, red, or brown hair |
| Usually burns, tans less than average | |
| Type III | Fair-skinned, largest group of U.S. citizens |
| Sometimes burns mildly, tans about average | |
| Type IV | Still considered white-skinned |
| Rarely burns, tans more than average and with ease | |
| Type V | Intermediate-colored skin; that is, Asian, Latin, Indian |
| Brown skin | |
| Type VI | Black-skinned persons |
| Never burns |
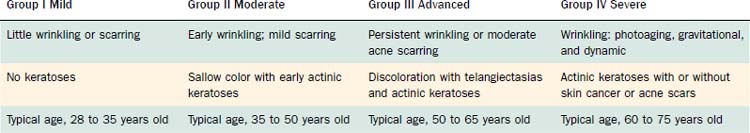
The Glogau classification system18 was created in 1994 and provides an objective assessment of the degree of photoaging, categorizing the patient’s skin damage into mild, moderate, advanced, or severe (groups I through IV) (Table 27-2). Patients in category I are often young with minimal photoaging and are best managed with a superficial peel in conjunction with a good medical skin care program. Patients in category II or III are candidates for medium-depth peels in addition to long-term medical therapy as with retinoids or alpha-hydroxy acids. Category IV photoaging patients are best treated with medium or deep chemical peels, ablative lasers, or dermabrasion, in conjunction with long-term medical skin care regimens.
There are several aesthetic and therapeutic indications for chemical peels and resurfacing (Table 27-3).
Table 27-3 Indications for Facial Resurfacing
| Aesthetic Indications |
| Therapeutic Indications |
Data from McCollough EG, Hillman RA Jr. Symposium on the aging face. Otolaryngol Clin North Am. 1980;13:353; Farber GA, Collins PS, Scott MW. Update on chemical peel. J Dermatol Surg Oncol. 1984;10:559; and Litton C, Sachowicz EH, Trinidad GP. Present day status of the chemical face peel. Aesthetic Plast Surg. 1986;10:1.
Contraindications
There are a few relative contraindications to chemical peels in addition to some absolute contraindications (Table 27-4). In the past, a history of herpes simplex virus was a contraindication to chemical peel.19 With the advent of antiviral drugs, however, acyclovir (Zovirax) or valacyclovir (Valtrex) can be effectively used as preventive or therapeutic intervention. Telangiectasias are relative contraindications in that they become more apparent after chemical peels or laser resurfacing. Confirmed malignant lesions should not be treated with chemical peels unless they are very superficial basal cell carcinomas. Nevoid or nevus lesions may become darker or actually stimulated to grow, and port-wine stains, hemangiomas, and neurofibromatoses are not effectively treated with chemical peels. Contraindications include the presence of hepatorenal disease or cardiac disease (for phenol peels), unless approved by an appropriate specialist. True documented allergies to an agent are obvious contraindications, and dressings should be latex free in sensitive patients. Patients who are unstable psychologically should not be treated with any resurfacing modality, particularly because the postoperative care may require intense patient involvement, education, and understanding.
Table 27-4 Brody’s Relative and Absolute Contraindications to Chemical Peels
| Relative Contraindications |
| Absolute Contraindications |
Chemical Peels
Chemical Peel Agents
Superficial Peels
Several chemical agents fall into the superficial peel category. These agents include low concentrations of glycolic acid; 10% to 20% TCA; Jessner’s solution (resorcinol, 14 g; salicylic acid, 14 g; lactic acid, 14 mL; ethanol, 100 mL); tretinoin; 5-fluorouracil (5-FU); and salicylic acid, a beta-hydroxy acid. The depth of the peel achieved with each of the above agents varies depending on the concentration of agent used, the duration of the application, and the number of times the agent is applied. During application, there may be a mild stinging followed by a level I frosting, defined as the appearance of erythema and streaky whitening on the surface.18 Regular washing with a mild cleanser and the use of routine moisturizers and sunscreens is all that is needed after the procedure. Superficial peels usually cause mild erythema and desquamation, with a healing time varying from 1 to 4 days, depending on the strength of the chemical agent.
Medium-Depth Chemical Peels
Monheit has demonstrated the use of Jessner’s solution before the application of TCA as a synergistic combination.19a Jessner’s solution effectively destroys the epidermal barrier by breaking up individual keratinocytes, allowing deeper and more even penetration of the 35% TCA. This technique is useful for the improvement of mild to moderate photoaging. There is minimal risk of pigmentary or textural complications, and this combination softens fine rhytids and freshens sallow, atrophic skin. Collagen remodeling and thickening occur over a 3- to 4-month period, with continued improvement in rhytid effacement and texture quality of aging skin. Deep furrows, however, are not eliminated with this medium-depth combination alone. The Jessner’s solution plus 35% TCA combination has been as effective as topical 5-FU chemotherapy in removing grossly visible and clinically undetectable actinic keratoses, with less morbidity and the positive effect of antiaging. This combination of agents is also used to blend resurfacing procedures with the surrounding skin. For example, patients who have undergone dermabrasion, CO2 laser resurfacing, or deep chemical peels in an isolated region (e.g., perioral or periorbital) may develop a sharp line of demarcation or hypopigmentation when compared with nontreated skin. In these instances, use of Jessner’s solution plus 35% TCA on the surrounding nontreated skin helps blend the treated area into its surroundings.
Technique: Medium-Depth Chemical Peels
The skin must first be cleansed of all residual oils, debris, and excess stratum corneum before the application of any peels (Fig. 27-1). The patient’s face is vigorously scrubbed with acetone using 2- × 2-cm gauze pads folded on a hemostat. Thorough degreasing is necessary for even penetration of the peeling solution. Uneven or splotchy peels are typically caused by residual oils on the stratum corneum from inadequate degreasing.
After the Jessner’s solution has dried, 35% TCA is evenly applied using cotton pads or swabs. The amount of TCA delivered to the skin surface is dependent on the number of applications, the degree of saturation (volume of solution), the amount of pressure applied to the skin, and contact time with the peel solution. Larger areas, including the forehead, bilateral cheeks, nose, and chin, are treated first with cotton pad applicators. Then, using cotton swabs, the perioral area and eyelids are treated, coming within 1 to 2 mm of the lower eyelid margin. An assistant should always be on standby with sterile eye wash for irrigation in case the surgeon inadvertently spills any peel solution into the eye. The white frost should appear within 30 seconds to 2 minutes after application of the TCA peel (Figs. 27-2 and 27-3). Before retreating an area, however, one should wait at least 3 to 4 minutes to ensure that the frosting has reached its peak before determining asymmetry. Additional applications can then be added with caution, because the depth of peel and potential complications are proportional to the volume of chemical applied.
The white frosting seen after a peel indicates the process of keratocoagulation, the completion of the chemical reaction. A level II or III frosting is a sufficient end point of a medium-depth peel. Level II frosting is defined as a white coat frosting with a background of erythema. Level III frosting is a solid white enamel frosting with no background of erythema, indicative of penetration into the reticular dermis. Such level III peeling should be limited to areas of thicker skin and heavy actinic damage. Sensitive areas such as thin eyelid skin and bony prominences (which have a high propensity for scarring) should be limited to a level II frosting.18
An immediate burning sensation is felt with the application of the TCA peel, but this begins to dissipate with the onset of frosting and is typically resolved by the time of discharge. Cool saline compresses offer symptomatic relief for a peeled area and are used over the entire face after completion of a peel. On completion of the peel, a brawny, dusky erythema progresses over the first 12 hours. Mild to moderate edema soon follows and can be severe over the thin eyelid skin and forehead regions. As the edema begins to resolve, dark crusts appear that peel off during the subsequent 5 to 7 days to reveal a new, erythematous epithelium. The redness soon fades to a pink color that resembles a sunburn and can typically be camouflaged with makeup by the 10th day after the peel. A formal makeover with a makeup artist within the aesthetics department is a valuable experience for the patient once he or she has reepithelialized on day 10. The patient can begin using sunscreens as tolerated. He or she should wait at least 3 months before resuming regular aesthetic skin care services such as superficial chemical peels or microdermabrasion. Cleansing facials can begin as early as 4 to 6 weeks after the peel. Repeat medium-depth chemical peel should not be performed for at least 1 year. Several studies have demonstrated microscopic improvement of collagen thickness progressing over a 6- to 13-month period (Fig. 27-4).

Figure 27-4. A, Pretreatment medium-depth chemical peel. B, Posttreatment medium-depth chemical peel.
Deep Chemical Peels
Resurfacing techniques that penetrate or wound the midreticular dermis are classified as deep chemical peels. Patients with Glogau group III or IV photodamage may require deep chemical peeling. The classic chemical compound is the Baker’s solution that consists of the following20:
Phenol itself is carbolic acid (C6H5OH), an aromatic benzene-ring hydrocarbon formed from coal tar.6,14,21 At concentrations greater than 80%, carbolic acid is a keratocoagulant precipitating the surface protein, thus preventing further penetration of the peel solution. Phenol produces an extremely rapid denaturization and irreversible coagulation.5 Further penetration of the phenol is prevented when the keratin protein binds to the phenol, creating large molecules that cannot penetrate further. McCollough and Hillman14 state that if the concentration of phenol is less than 50%, it becomes keratolytic, interrupting sulfur bridges in the keratin layer, and can then produce deeper penetration and more destruction than desired. Therefore, as one decreases the concentration of phenol, the depth and therefore wounding of tissue becomes more severe.
The croton oil included in the formula is composed of glycerides of several acids and can be very irritating to the skin. Because of its inflammatory characteristics, it induces more collagen formation.6,14 Recent studies have demonstrated that croton oil is the key ingredient, creating the significant depth of wounding.22 Some surgeons vary the depth of Baker’s solution peeling by using one, two, or three drops of croton oil. Soap in the solution acts as a surfactant, reducing surface tension and enhancing the penetration of the waxes and cholesterol esters of phenol. Septisol (hexachlorophene and alcohol) is a partial astringent that helps remove the stratum corneum and plays the role of a surfactant. The addition of distilled water produces the desired concentration of phenol between 50% and 60%. The mixture of ingredients is freshly prepared and must be stirred vigorously before application because of its poor miscibility.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree