(1)
Department of Ophthalmology, St. Thomas’ Hospital, London, UK
10.1 Clinical Features
10.1.1 Other Conditions
10.1.2 Secondary Macular Pucker
10.2 Surgery
10.3 Success Rates
10.5 Membrane Recurrence
10.6 Summary
Abstract
Idiopathic epiretinal membrane formation in the macula is also stimulated by posterior vitreous detachment, giving the clinical entities of macular pucker or cellophane maculopathy. It is postulated that the PVD damages the internal limiting membrane stimulating microglial cells proliferation and fibrosis (Messmer et al. 1998; Snead et al. 2004). Myofibroblastic activity may be present (De Juan et al. 1985) and may be commoner in younger patients (Smiddy et al. 1992).
Electronic supplementary material
The online version of this chapter (doi:10.1007/978-3-642-31872-6_10) contains supplementary material, which is available to authorized users.
10.1 Clinical Features
Idiopathic epiretinal membrane formation in the macula is also stimulated by posterior vitreous detachment, giving the clinical entities of macular pucker or cellophane maculopathy. It is postulated that the PVD damages the internal limiting membrane stimulating microglial cells proliferation and fibrosis (Messmer et al. 1998; Snead et al. 2004). Myofibroblastic activity may be present (De Juan et al. 1985) and may be commoner in younger patients (Smiddy et al. 1992).

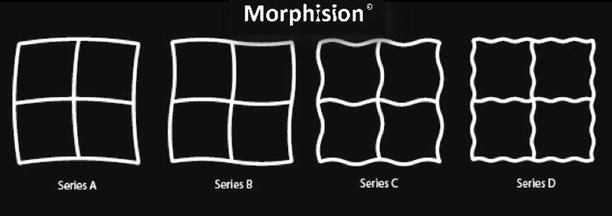
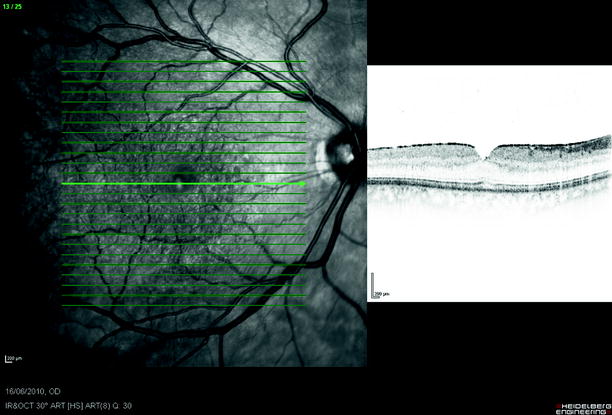

Fig. 10.1
A diffuse membrane can be described as cellophane maculopathy. This is part of the spectrum of epiretinal membrane formation from posterior vitreous detachment in middle-aged and elderly individuals
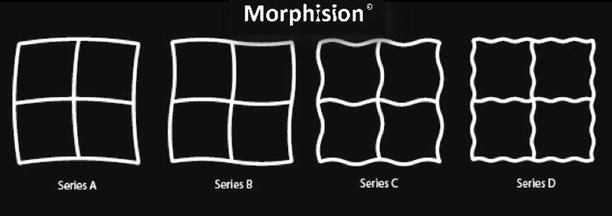
Fig. 10.2
Use the Apple App Morphision, which uses sinusoidal patterns, to measure and monitor distortion in these patients
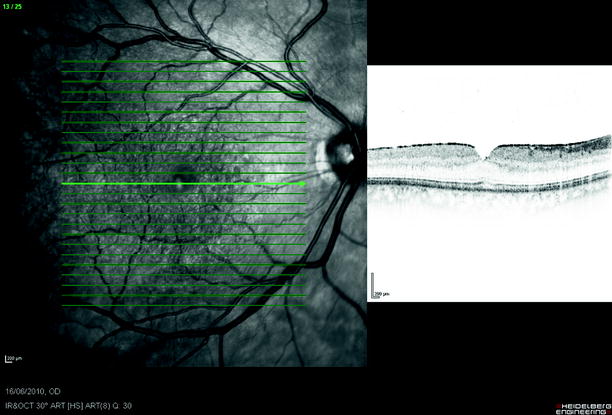
Fig. 10.3
Cellophane maculopathy can be seen coincidentally in many patients without symptoms
The patient notices a reduction of vision accompanied by distortion of images and macropsia (increased image size) as the membrane pulls the retina centrally. The membrane can be seen as a reflective sheet (cellophane) or as a thick, opaque membrane which is drawing the retinal arcades together. A pseudohole in the central membrane can sometimes be detected and distinguished from a hole in the retina (macular hole) by a negative Watzke–Allen test (Allen 1976; Martinez et al. 1994) and by OCT. Vitreomacular traction is present when the vitreous separation is incomplete and an area of attachment of the epiretinal membrane to the posterior hyaloid membrane remains. The membrane is associated with the presence of mild CMO on FFA.
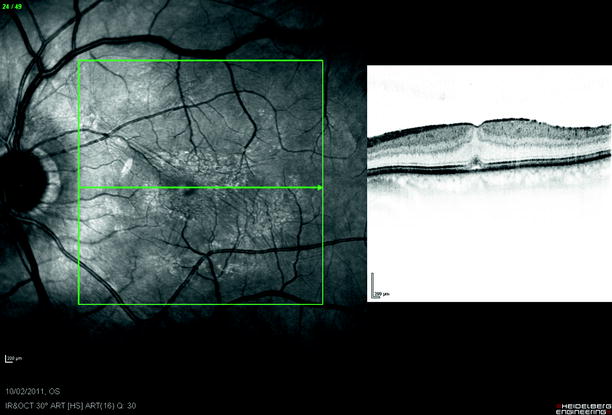
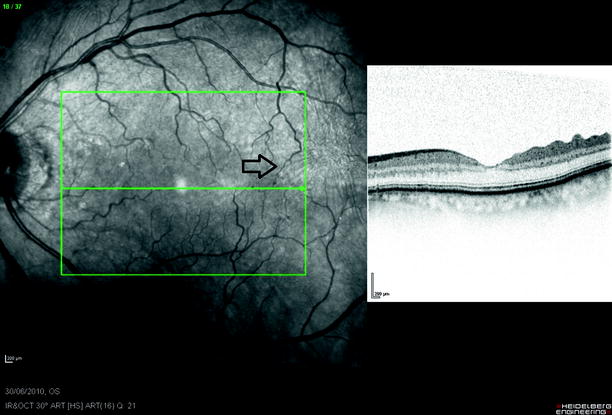
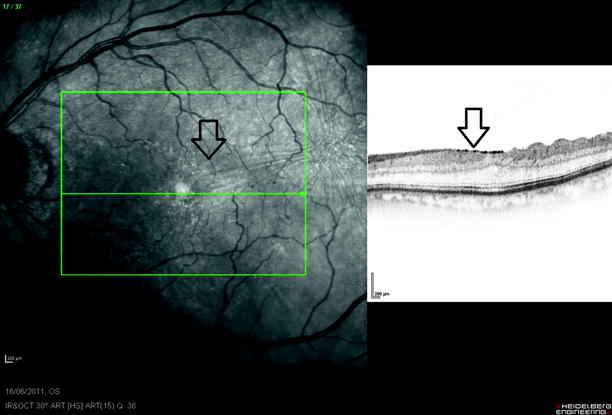
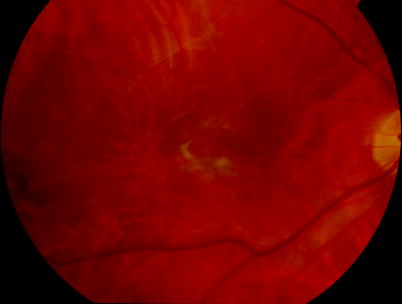
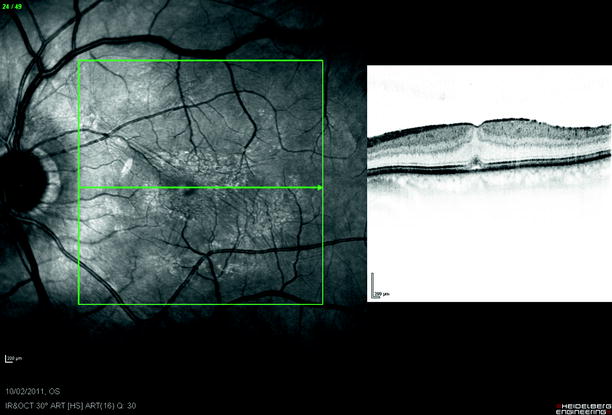
Fig. 10.4
Cellophane starts to distort the fovea and flatten the foveal dip
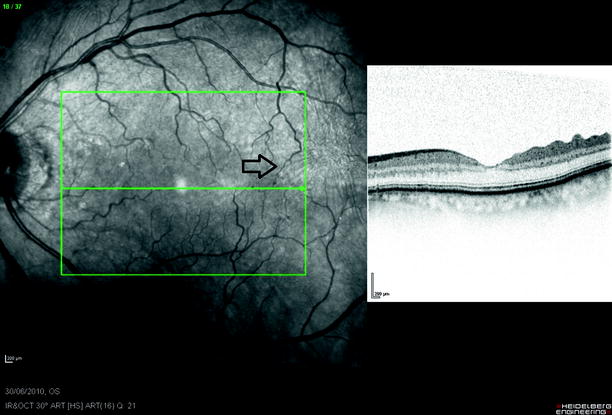
Fig. 10.5
Although most ERM are stable after presentation, some can progress with reduction in vision. This ERM (arrows) has gradually grown across the macula over 1 year
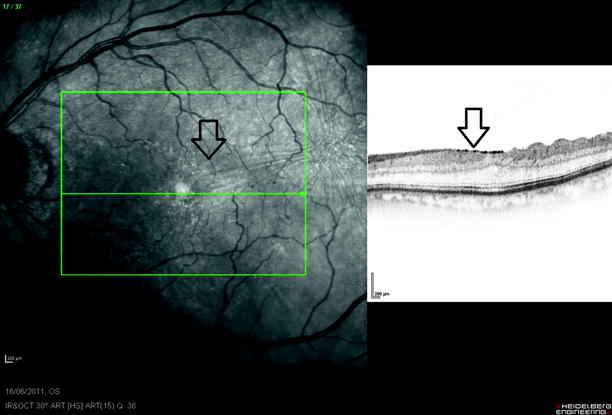
Fig. 10.6
See previous figure
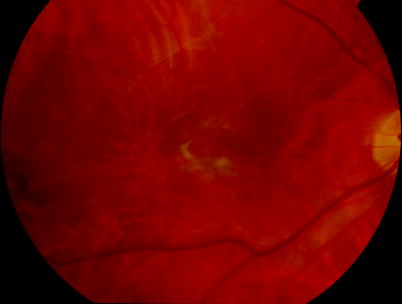
Fig. 10.7
A severe ERM causing pucker of the macula
Young patients often have an attached PHM and more often show spontaneous separation of the ERM because the vitreous separates taking the ERM with it (Desatnik et al. 1999). A PVD is not always seen (Meyer et al. 2004).

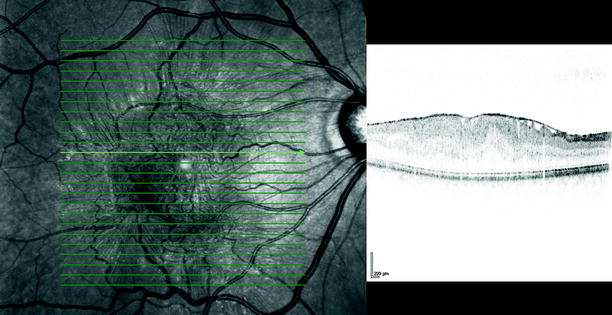
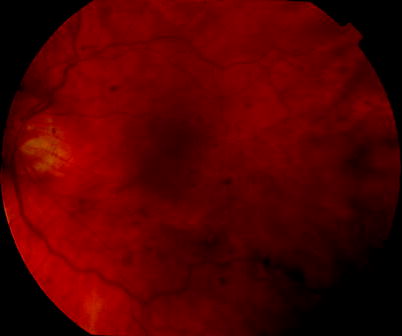
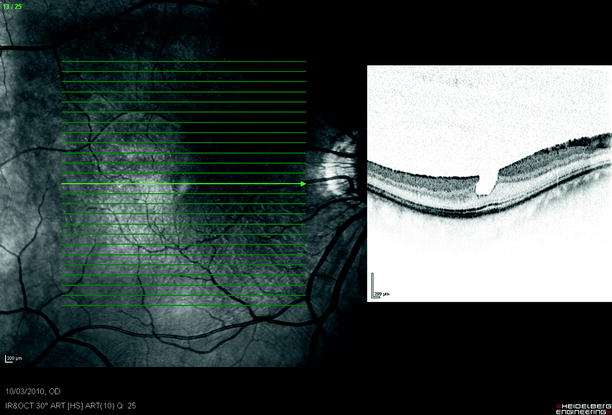
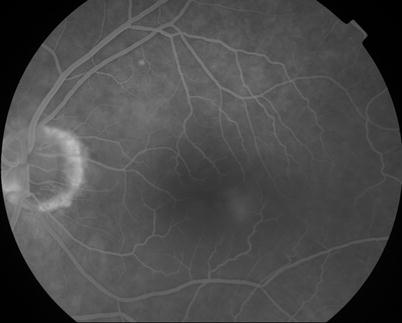
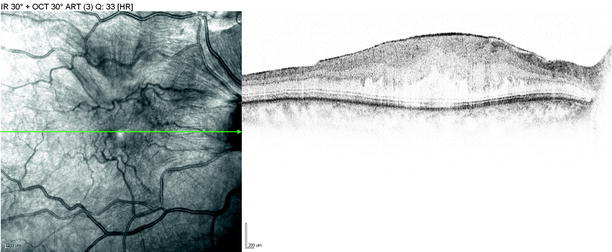
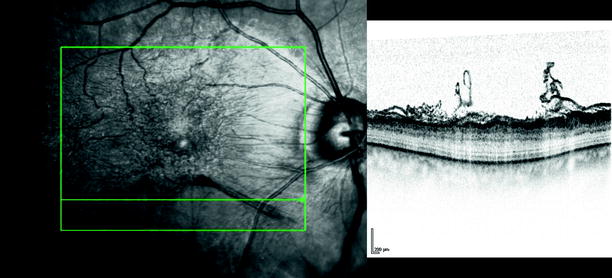

Fig. 10.8
A large epiretinal membrane is pulling the blood vessels centrally towards the fovea, distorting the anatomy of the macula
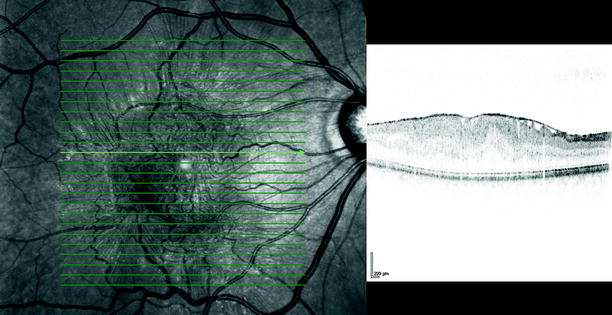
Fig. 10.9
The OCT shows thickening and wrinkling of the retina from an ERM. Pegs of attachment of the ERM to the retinal can be seen
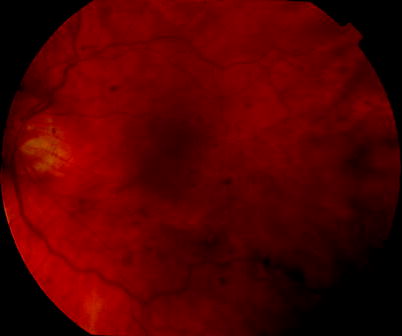
Fig. 10.10
An epiretinal membrane is shown with a pseudohole over the fovea
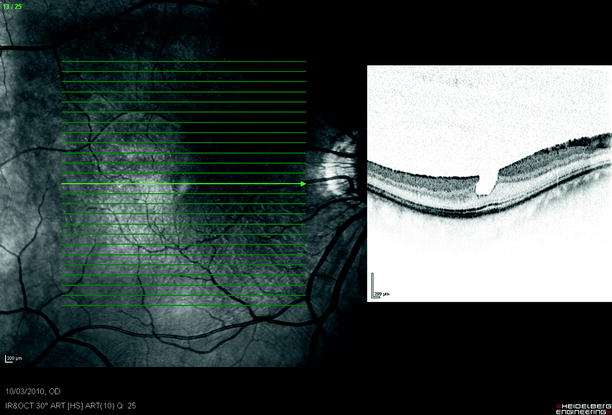
Fig. 10.11
A mild cellophane ERM with pseudohole, vision was 20/20
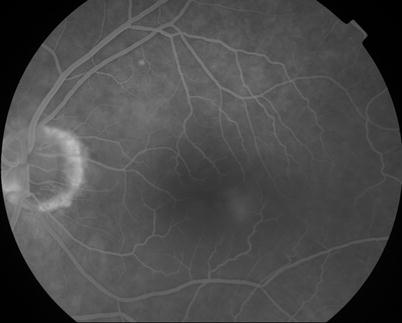
Fig. 10.12
ERM on the macula will produce mild CMO in some cases, seen on FFA
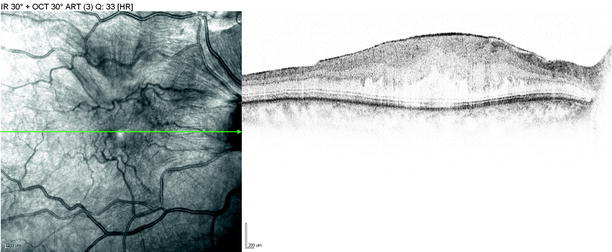
Fig. 10.13
An ERM on HD OCT notice retinal wrinkling on the SLO scan and thickening of the retina on OCT
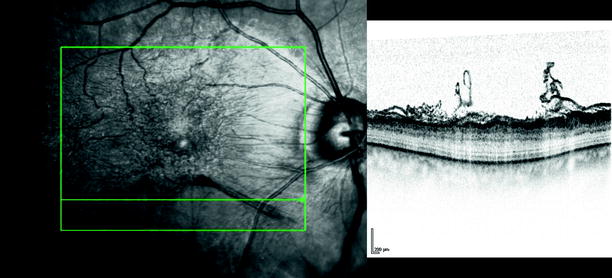
Fig. 10.14
This ERM has a rolled edge which will be easily grasped during surgery. Notice the elastic membrane has rolled at its lifted edge
10.1.1 Other Conditions
Mild vitreous shrinkage with a taut posterior hyaloid membrane that is still attached to the retina may be partly responsible for cystoid macular oedema in diabetic maculopathy or uveitis.


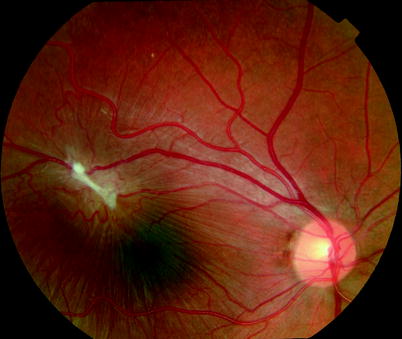
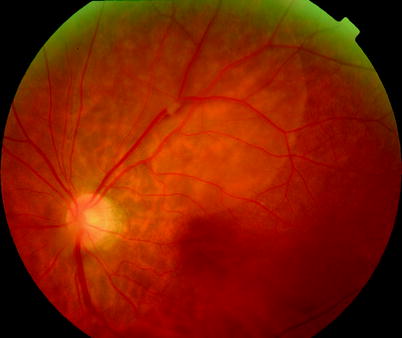

Fig. 10.15
In young patients, spontaneous separation of the ERM is common. With the ERM visible on the PHM of the PVD

Fig. 10.16
See previous figure
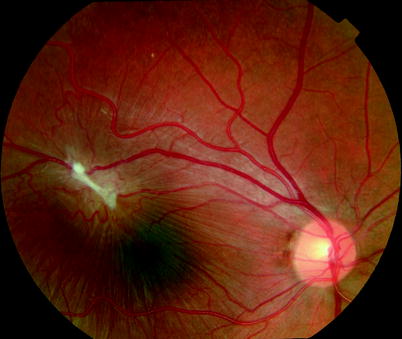
Fig. 10.17
This macular lesion was seen coincidentally with macular striae in a patient of 13 years of age
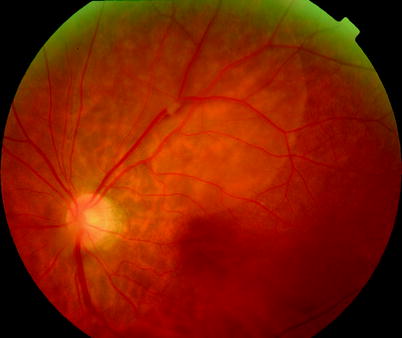
Fig. 10.18
This eye was observed with an area of chronic shallow elevation of the retina from vitreomacular traction without progression. Usually VM traction is associated with ERM of the macula, but no ERM had developed in this eye
10.1.2 Secondary Macular Pucker
Macular pucker can occur after retinal tear or retinal detachment (de Bustros et al. 1988a) seen in approximately 7 % (Lobes 1978) and is more commonly seen in PVR. A 6-month prevalence of 15 % has been described after surgery for PVR by vitrectomy and gas or silicone oil (Cox et al. 1995). Post-mortem studies suggest much higher prevalence, most of which must be subclinical (Wilson and Green 1987). The ERM in RRD can occur relatively rapidly with symptoms deteriorating over weeks (Sheard et al. 2003). In RRD, the ERM is more often associated with pigmented cells, histologically of RPE origin (Cherfan et al. 1988).
In some cases, the ERM is secondary to branch retinal vein occlusion (BRVO) in which case it is worth checking an FFA to assess the perifoveal arcade. If this is not complete, this may indicate a poorer prognosis for vision postoperatively.
ERM can appear secondary to uveitis.
If the hyaloid is incompletely removed at vitrectomy in patients with vitreoschisis such as diabetic retinopathy, ERM may occur.
ERM can occur in patients with peripheral retinal angiomata, for example, von Hippel–Lindau disease or idiopathic acquired angiomata (Laatikainen et al. 1989; Machemer 1990).
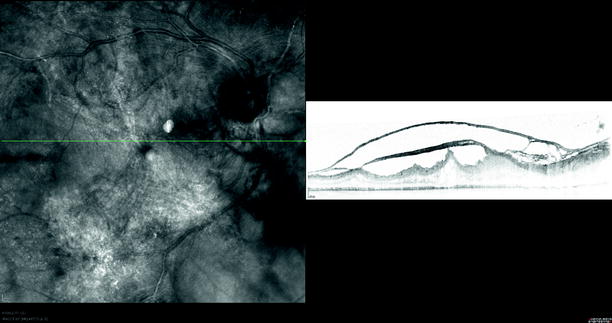
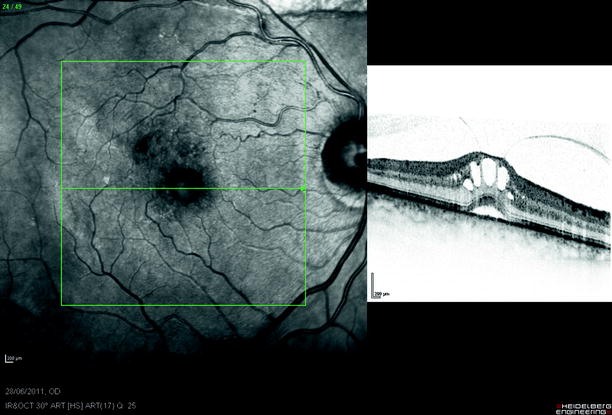
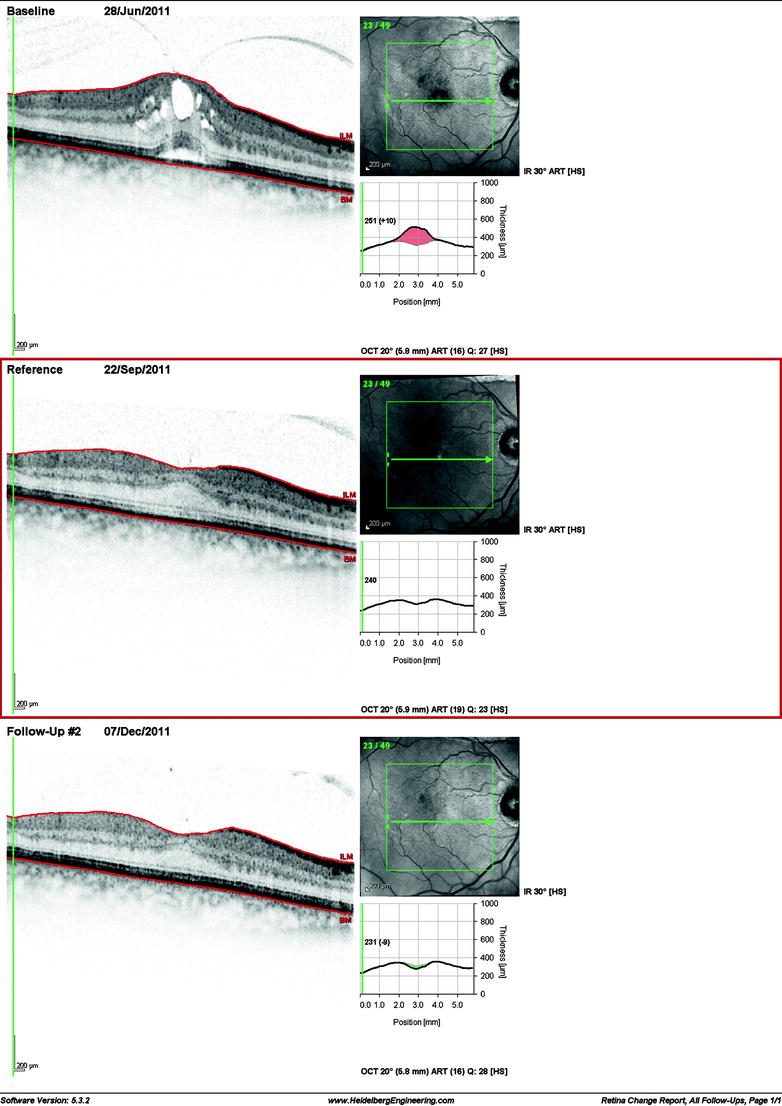
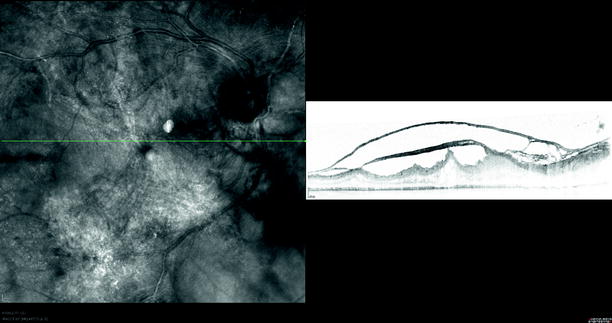
Fig. 10.19
Extensive ERM and traction in an eye which has received plaque radiotherapy for peripheral angiomata
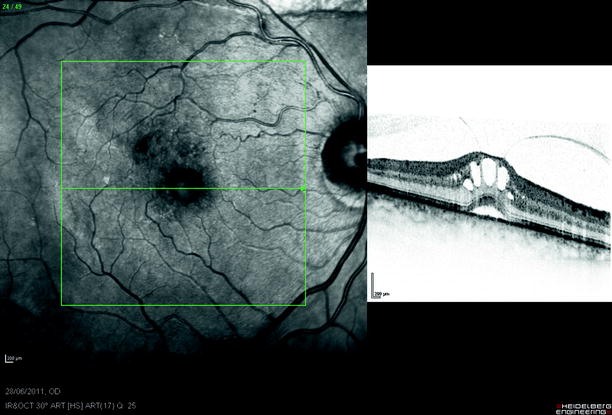
Fig. 10.20
Vitreomacular traction noticed after cataract surgery
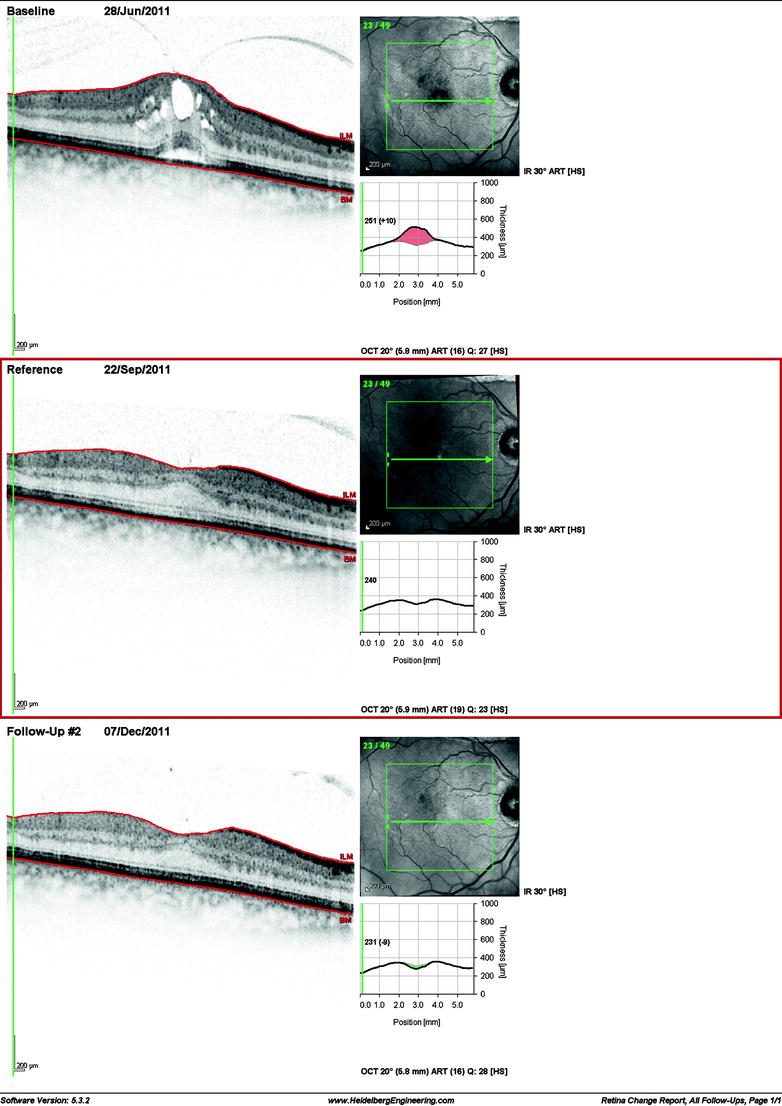
Fig. 10.21
Vitreomacular traction after phacocataract surgery can spontaneously resolve after separation of the vitreous; therefore, it is worth waiting 2 months to see if this will occur before operating
In sickle-cell disease, ERM are seen in 4 % (Carney and Jampol 1987).
Candida endophthalmitis also stimulates ERM in some patients (McDonald et al. 1990).
Combined hamartoma and FEVR may be associated with ERM in young patients (Mason and Kleiner 1997).
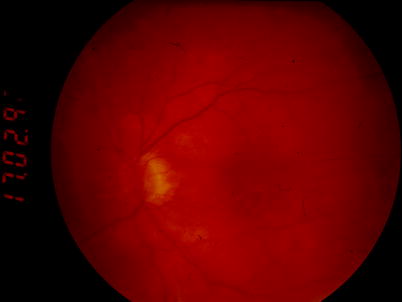

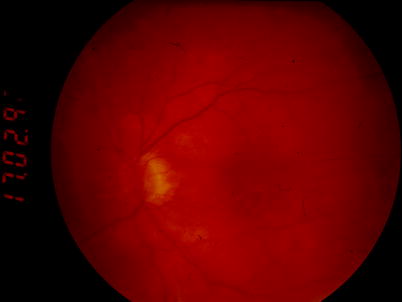
Fig. 10.22
The membrane has been removed from this macula

Fig. 10.23
See previous figure
10.2 Surgery
Table 10.1
Difficulty rating for PPV for macular pucker
Difficulty rating | Easy |
Success rates | Moderate |
Complication rates | Low |
When to use in training | Early |
Additional surgical steps
Stain the ERM with trypan blue.
Peel off the ERM.
Fig. 10.24
ERMs have pegs of attachment to the retina
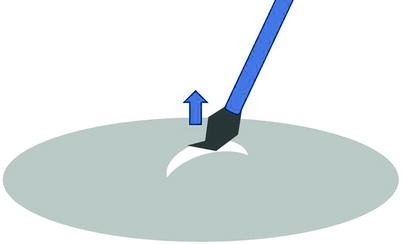
Fig. 10.25
Use a bent MVR blade to lift the ERM to provide an edge. Scraping the ERM as per ILM peel does not create a hole or edge in the ERM because the ERM is elastic and will stretch with the movement of the blade; however, there is usually a virtual space between the ERM and the underlying ILM which can allow passage of a blade to commence lifting. Arrow shows direction of lift
In cellophane maculopathy, vitreomacular traction or macular pucker, pars plana vitrectomy is employed to access epiretinal membranes, allowing their surgical dissection and removal. This is often effective in reducing distortion and improving vision and is one of the easier procedures in vitreoretinal surgery (Michels 1981). In 20-gauge surgery, take a microvitreoretinal (MVR) blade and bend the end to about 45°. Make sure the tip is secure. Some MVRs are made of a material that is brittle and snaps on bending. If so, use an intraocular pick. The 45° angle allows visualisation of the end of the MVR (it is difficult to judge the depth of the end of a straight blade or forceps, and, therefore, the likelihood of injuring the retina is increased).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


