 Lacrimal Gland Primary Epithelial Tumors
Lacrimal Gland Primary Epithelial TumorsIntroduction: Lacrimal Gland Lesions
A variety of neoplasms and related lesions can arise in the lacrimal gland (1,2,3,4,5,6,7,8,9,10,11,12,13). Lacrimal gland lesions have many similarities to those that occur in the major salivary glands. Lesions of the lacrimal gland can be broadly divided into epithelial and nonepithelial lesions. Nonepithelial lesions such as the lymphoid tumors, inflammations, and other neoplasms that affect the lacrimal gland are covered in other chapters. This chapter covers primary benign and malignant lesions derived from the epithelial structures of the lacrimal gland.
It is important to recall that the lacrimal gland is the only tissue in the orbit that normally contains epithelium and any primary epithelial tumor in the orbit has most likely originated in the lacrimal gland. However, metastatic epithelial neoplasms can reach the orbit by hematogenous spread from distant organs and secondary epithelial neoplasms can invade the orbit from adjacent structures, such as eyelid, conjunctiva, intraocular tissues, paranasal sinuses, and nasopharynx. On rare occasions, congenital ectopic lacrimal gland tissue in the orbit can give rise to cysts and neoplasms (12,13).
True primary epithelial lesions of the lacrimal gland can be divided further into benign and malignant categories. Benign epithelial lesions include ductal epithelial cyst (dacryops) and pleomorphic adenoma (benign mixed tumor). The latter is the only important primary benign epithelial neoplasm of the lacrimal gland. There are several malignant epithelial neoplasms of the lacrimal gland, the most important of which is adenoid cystic carcinoma (ACC). Other less common malignancies include pleomorphic adenocarcinoma (malignant mixed tumor), primary adenocarcinoma, mucoepidermoid carcinoma, primary squamous cell carcinoma, sebaceous carcinoma, acinic cell adenocarcinoma, ductal carcinoma, lymphoepithelial carcinoma, myoepithelial carcinoma, and cystadenocarcinoma. Most of these uncommon neoplasms were discussed in a recent comprehensive review of the subject (5).
Primary epithelial malignancies of the lacrimal gland (PEMLG) occur mostly in middle-aged adults; they are less common in the very young and the elderly. However, the important ACC seems to have a biphasic age distribution with some occurring in children in the first or second decade and another group occurring in young to middle-aged adults. There is no known predilection for race or gender.
Estimates regarding the incidence of lacrimal gland lesions vary from series to series depending on the source of the material and specifically which lesions were included in the survey. Rather than confusing the reader with those numbers, we attempted to make close estimates based on a comprehensive literature review. The following represents a fairly accurate and easy-to-recall average incidence of various lesions (5).
About 10% of orbital space-occupying lesions occur in the lacrimal gland.
About 20% of solid lacrimal gland masses are of epithelial origin and 80% are of nonepithelial origin.
About 55% of reported epithelial tumors are benign and 45% are malignant.
Of primary epithelial malignancies of the lacrimal gland, about 60% are ACC, 20% are pleomorphic adenocarcinoma, 10% are primary (de novo) adenocarcinoma, 5% are mucoepidermoid carcinoma, and 5% are miscellaneous malignant epithelial neoplasms.
In the authors’ recent clinical series of 1,264 consecutive patients with orbital tumors from the Wills Eye Hospital Oncology Service, there were 114 (9%) lacrimal gland lesions. When dacryops (a cystic lesion) and other nonepithelial tumors were excluded, there were 30 solid primary epithelial tumors, of which 11 were pleomorphic adenoma and 19 were PEMLG. The 19 PEMLGs included 14 ACC (74%), 4 pleomorphic adenocarcinomas (21%), and 1 mucoepidermoid carcinoma (5%). That series, like most other studies, is biased in the sense that more difficult cases or malignant cases are likely to be referred to the Oncology Service. For example, several patients with ACC were referred for further management after incisional biopsy elsewhere disclosed the diagnosis. A completely excised pleomorphic adenoma would be less likely to prompt a referral to the Oncology Service.
Clinically, mass lesions in the lacrimal gland have consistent, but somewhat variable, features. Sizable solid lesions in the lacrimal gland fossa typically cause proptosis and inferior and nasal displacement of the globe. Benign epithelial tumors and lymphomas generally are painless, whereas malignant epithelial tumors and inflammations are more likely to cause pain. With imaging studies, benign tumors are more likely to show normal adjacent bone or smooth fossa formation. In general, malignant epithelial tumors are more likely to exhibit bone destruction as they progress. Clinical symptoms and signs and radiographic features are discussed in greater detail in the following sections.
Concerning prognosis, pleomorphic adenoma carries an excellent prognosis if the tumor can be completely removed within its capsule. Incomplete removal can lead to recurrence and eventual malignant transformation. Primary malignant epithelial tumors of the lacrimal gland are generally much more aggressive neoplasms with a relatively high incidence of local recurrence and distant metastasis despite aggressive treatment, often including orbital exenteration, irradiation, or chemotherapy. However, there is considerable variation in the degree of malignancy among the various malignant epithelial tumors (5).
General References
1. Shields JA, ed. Diagnosis and Management of Orbital Tumors. Philadelphia: WB Saunders; 1989:128-132.
2. Jakobiec FA, Bilyk JR, Font RL. Orbit. Lacrimal gland tumors. In: Spencer WH, ed. Ophthalmic Pathology. 4th ed. Philadelphia: WB Saunders; 1996:2485-2525.
3. Rootman J. Neoplasia. Epithelial tumors of the lacrimal gland. In: Rootman J, ed. Diseases of the Orbit. Philadelphia: JB Lippincott; 1988:345-361.
4. Henderson JW. Tumors of orbital bone. In: Henderson JW. Orbital Tumors. 3rd ed. New York: Raven; 1994:161-164.
5. Shields, JA, Shields CL, Epstein J, et al. Primary epithelial malignancies of the lacrimal gland. The 2003 Ramon L. Font Lecture. Ophthalmic Plast Reconstr Surg 2004;20:10-21.
6. Shields JA, Bakewell B, Augsburger JA, et al. Classification and incidence of space-occupying lesions of the orbit. A survey of 645 biopsies. Arch Ophthalmol 1984;102:1606-1611.
7. Shields JA, Bakewell B, Augsburger DG, et al. Space-occupying orbital masses in children. A review of 250 consecutive biopsies. Ophthalmology 1986;93:379-384.
8. Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: the 2002 Montgomery Lecture, part 1. Ophthalmology 2004;111:997-1008.
9. Reese AB. Expanding lesions of the orbit (Bowman Lecture). Trans Ophthalmol Soc UK 1971;91:85-104.
10. Shields CL, Shields JA, Eagle RC, et al. Clinicopathologic review of 142 cases of lacrimal gland lesions. Ophthalmology 1989;96:431-435.
11. Demirci H, Shields CL, Shields JA, et al. Orbital tumors in the older adult population. Ophthalmology 2002;109:243-248.
12. Rush A, Leone CR Jr. Ectopic lacrimal gland cyst of the orbit. Am J Ophthalmol 1981;92:198-201.
13. Green WR, Zimmerman LE. Ectopic lacrimal gland tissue. Report of eight cases with orbital involvement. Arch Ophthalmol 1967;78:318-327.
Lacrimal Gland Ductal Epithelial Cyst (Dacryops)
General Considerations
Ductal epithelial cyst, often called dacryops, is an inclusion cyst secondary to occlusion of one or more of the ducts that drain tears from the lacrimal gland into the conjunctival fornix (1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17). In a review of 645 orbital biopsies, it accounted for 5 cases (,1%) (2). In the review of 142 lacrimal gland biopsies, it accounted for 6% of cases (3). In the authors’ series of 1,264 consecutive space-occupying orbital lesions, dacryops accounted for 17% of epithelial lesions of the lacrimal gland and 2% of all orbital space-occupying lesions. The frequency is probably higher; most lesions are relatively small and many do not come to clinical recognition and surgical excision. Only 4 of the 19 cases required surgical excision. In rare instances, an epithelial cyst can arise from ectopic lacrimal gland tissue in the orbit (9,10).
Clinical Features
Ductal epithelial cyst usually arises from the palpebral lobe of the lacrimal gland in adults and presents as a unilateral or bilateral, painless, nontender, fluctuant mass in the forniceal conjunctiva superotemporally (6). It can occur spontaneously or it can follow dacryoadenitis. The lesion is often slowly progressive, but it can remain stable for long periods of time. It can intermittently discharge tears and then gradually re-form. There has been a report of a mucoepidermoid carcinoma of the lacrimal gland arising from a chronic dacryops (16). The differential diagnosis includes many of the other conjunctival and orbital cysts discussed elsewhere in these atlases.
Diagnostic Approaches
Ductal epithelial cyst can usually be visualized clinically and the diagnosis is not usually difficult. Imaging studies demonstrate a cystic mass corresponding to the anterior part of the lacrimal gland. These studies can help to delineate the posterior extent of the lesion and rule out a solid tumor with an anterior cystic component. In contrast to dermoid cyst and malignant lacrimal gland tumor, the adjacent bone is normal. Some solid epithelial tumors of the lacrimal gland can induce a secondary ductal cyst that can lead to diagnostic confusion (7).
Pathology
Histopathologically, ductal epithelial cyst has a clear lumen and an epithelial lining that consists of one or two layers of somewhat flattened epithelium, similar to a lacrimal gland duct. The inner layer of epithelium is cuboidal and the outer layer is composed of myoepithelial cells. A few mucin-secreting goblet cells are often present. The pathogenesis may be related to inflammation and scar tissue that obstructs the duct, followed by hypersecretion and ductal ectasia (15).
Management
As implied, smaller, asymptomatic lesions can be observed and large ones can be resected locally by a superotemporal conjunctival forniceal approach, taking care not to disrupt the ducts that drain the palpebral lobe if possible. Marsupialization of the cyst is another surgical option, particularly in patients who have decreased tear production. To avoid standard surgery, some authors have described success using blue-green argon laser to collapse the cyst (14).
Selected References
1. Shields JA. Epithelial tumors of the lacrimal gland. Dacryops. In: Shields JA, ed. Diagnosis and Management of Orbital Tumors. Philadelphia: WB Saunders; 1989:260-262.
2. Shields JA, Bakewell B, Augsburger DG, et al. Classification and incidence of space-occupying lesions of the orbit. A survey of 645 biopsies. Arch Ophthalmol 102:1606-1611.
3. Shields CL, Shields JA, Eagle RC, et al. Clinicopathologic review of 142 cases of lacrimal gland lesions. Ophthalmology 1989;96:431-435.
4. Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: the 2002 Montgomery Lecture, part 1. Ophthalmology 2004;111:997-1008.
5. Bullock JD, Fleishman JA, Rosset JS. Lacrimal ductal cysts. Ophthalmology 1986;93:1355-1360.
6. Smith S, Rootman J. Lacrimal ductal cysts. Presentation and management. Surv Ophthalmol 1986;30:245-250.
7. Christie DB, Woog JJ, Lahav M. Combined dacryops with underlying benign mixed cell tumor of the lacrimal gland. Am J Ophthalmol 1995;11:97-99.
8. Bartley GB. Orbital lobe lacrimal ductal cysts. Surg Neurol 1995;43:521.
9. von Domarus H. A lacrimal gland cyst in the orbit. J Craniomaxillofac Surg 1987;15:106-109.
10. Sen DK, Thomas A. Simple dacryops. Am J Ophthalmol 1967;63:161.
11. Bradey N, Hayward JM. Case report: bilateral lacrimal gland enlargement: an unusual manifestation of dacryops. Clin Radiol 1991;43:280-281.
12. Rush A, Leone CR Jr. Ectopic lacrimal gland cyst of the orbit. Am J Ophthalmol 1981;92:198-201.
13. Green WR, Zimmerman LE. Ectopic lacrimal gland tissue. Report of eight cases with orbital involvement. Arch Ophthalmol 1967;78:318-327.
14. Pantaleoni FB, Spagnolo S, Martini A, et al. Argon laser photocoagulation in the treatment of the palpebral lobe cysts of the lacrimal gland (dacryops). Ophthalmic Surg Lasers 1997;28:690-692.
15. Jakobiec FA, Bilyk JR, Font RL. Orbit. In: Spencer WH, ed. Ophthalmic Pathology. 4th ed. Philadelphia: WB Saunders; 1996:2516-2518.
16. Levin LA, Popham J, To K, et al. Mucoepidermoid carcinoma of the lacrimal gland. Report of a case with oncocytic features arising in a patient with chronic dacryops. Ophthalmology 1991;98:1551-1555.
17. Brownstein S, Belin MW, Krohel GB, et al. Orbital dacryops. Ophthalmology 1984;91:1424-1428.
Lacrimal Gland Ductal Epithelial Cyst (Dacryops)
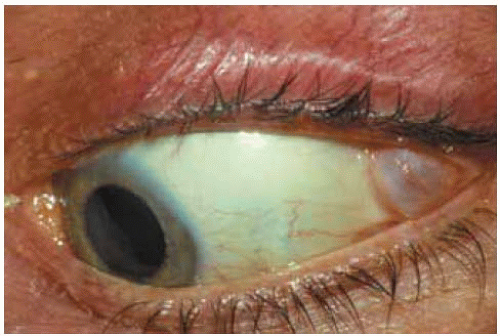
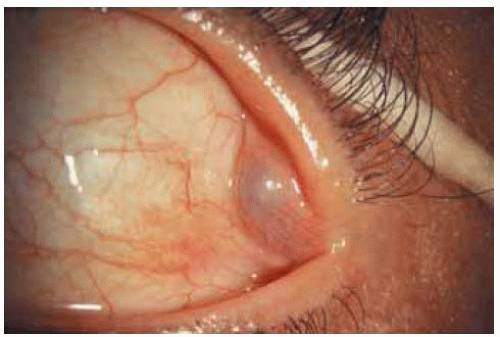
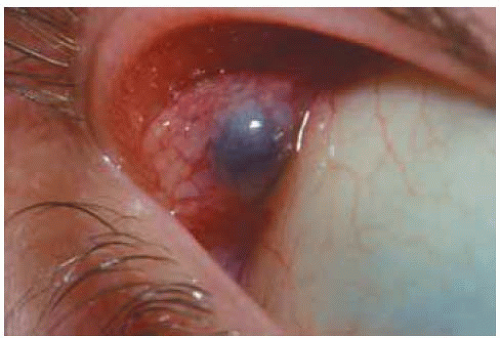
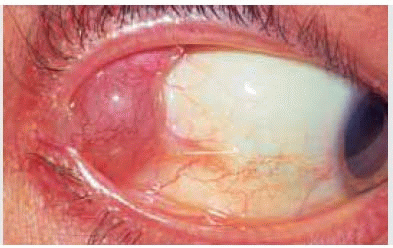
In most instances a dacryops is small, asymptomatic, does not prompt a medical consultation, and is detected on routine ocular examination. Occasionally, a dacryops can cause irritation or foreign body sensation and may require symptomatic treatment or surgical removal. Examples of relatively small, asymptomatic dacryops are depicted.
Lacrimal Gland Ductal Epithelial Cyst (Dacryops)
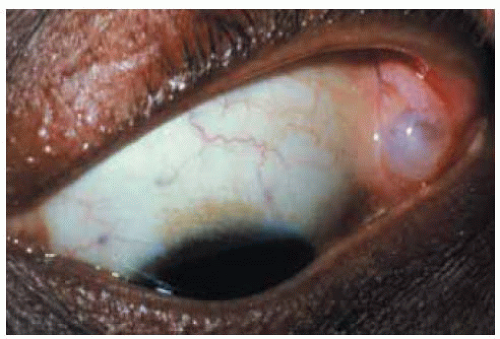
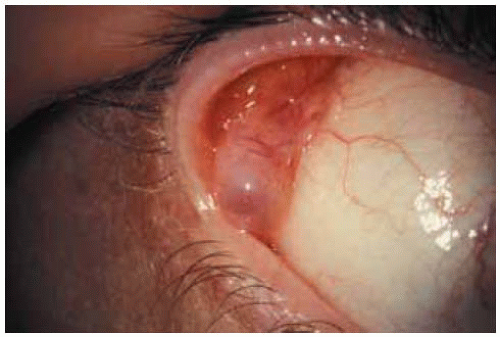
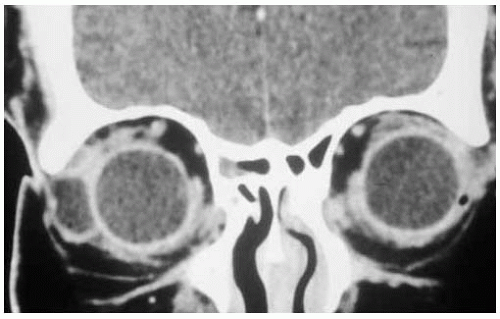
In some instances, dacryops can be larger and cause bothersome symptoms. A case that was studied by computed tomography (CT) and managed by surgical excision is shown.
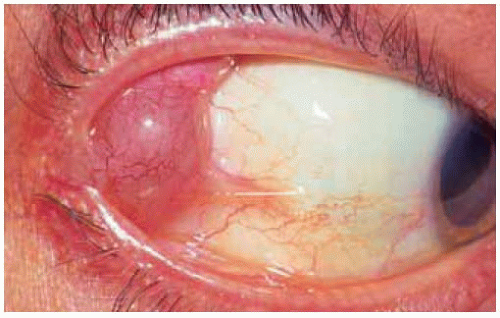 Figure 37.7. Dacryops superotemporally in a 55-year-old man. The lesion was producing persistent discomfort. |
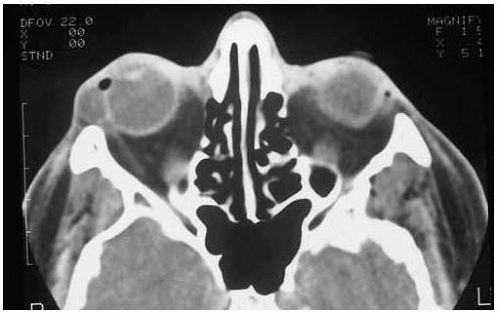 Figure 37.8. Axial computed tomography of patient shown in Figure 37.7, demonstrating cystic lesion near anterior orbital rim. |
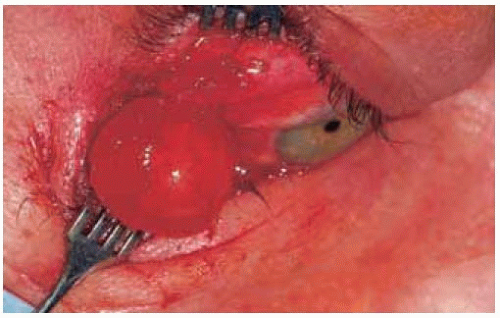 Figure 37.10. Appearance of intact lesion at time of surgical removal by a superotemporal conjunctival approach. |
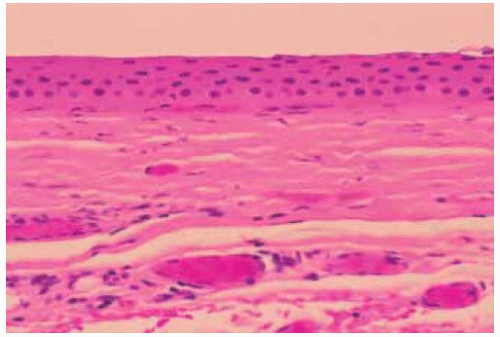 Figure 37.11. Histopathology showing flattened epithelium and fibrous tissue wall of the cyst. (Hematoxylin-eosin 25.) |
Lacrimal Gland Pleomorphic Adenoma (Benign Mixed Tumor)
General Considerations
Tumors of the lacrimal gland are quite similar histopathologically to tumors that arise in the major salivary glands and other minor salivary glands.
Pleomorphic adenoma (benign mixed tumor) is the most important benign epithelial tumor of the lacrimal gland (1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25). In the authors’ earlier series of orbital biopsies, it accounted for 2% of 645 specimens (2). In the more recent clinical series, the 11 pleomorphic adenomas accounted for 10% of all lacrimal gland lesions and for only 1% of all orbital lesions (3). Among 142 lacrimal gland biopsies, it accounted for 12% of cases (4). It usually arises from the orbital lobe of the lacrimal gland, although it has rarely developed in the palpebral lobe or from ectopic lacrimal gland tissue in the orbit (3,6). It is generally a disease of young to middle-aged adults (mean age, 39 years), but it also occurs in children (14,15,21).
Clinical Features
Pleomorphic adenoma of the lacrimal gland generally presents as a unilateral progressive nonpainful mass in the anterior aspect of the orbit superotemporally. As the lesion enlarges, it produces proptosis and downward and nasal displacement of the globe. The relative absence of pain is important in differentiating a pleomorphic adenoma from many malignant lacrimal gland tumors, which characteristically produce more pain (1,6,23).
Diagnostic Approaches
Imaging studies disclose a round to ovoid circumscribed mass in the lacrimal gland fossa with a smooth to slightly irregular surface. There may be fossa formation in the adjacent bone, but frank bone destruction, as seen with some malignant tumors, is usually not evident. Computed tomography is the best method to assess bone involvement (7). The anterior portion of the mass seems to stop at or posterior to the orbital rim, suggesting that the lesion affects the orbital lobe but spares the palpebral lobe of the lacrimal gland. There may be an adjacent bony fossa, but true bone erosion is very rare (20). Like malignant epithelial tumors, pleomorphic adenoma shows low to isointense signal on T1-weighted and hyperintense signal on T2-weighted images (24,25).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree