Chapter 1 Introduction to Allergy
History of Allergy
The concept of allergy is relatively recent in the history of clinical medicine. Until the late 19th century allergy was not considered to be a medical discipline. In fact, the concept of hypersensitivity reactions to generally innocuous substances present in the environment had not yet been developed. Seasonal catarrh or “hay fever” was seen as toxic reactions to various plant products, and therapies were developed to neutralize these “toxins.”
Despite a strong clinical interest in allergy and an active system of clinical practice, the causes of allergy were not well understood until the 1960s. During that period of time Johannson and Ishizaka independently isolated immunoglobulin E from the serum of allergy patients and demonstrated its primary role in clinical allergy. This development demonstrated the molecular basis of allergy and allowed both a rapid progression of the science related to allergy practice as well as the growth of standardized in vitro serum tests for specific IgE. These developments continued to foster a growth in clinical allergy practice, and led to the rapid influx of clinical and scientific research in the field of allergy-related immunology. These interests continue to the present day.
Prevalence of Allergic Diseases
In general, studies have suggested that allergic diseases, both respiratory and nonrespiratory, are steadily increasing in prevalence. This rise has been seen around the globe, not only in the west but also throughout the developing world. It has been estimated that 25% to 30% of the population in the western world are affected by allergic illnesses on a yearly basis, with a somewhat lower prevalence in the developing world. By a variety of indicators, the prevalence of allergic diseases such as rhinitis and asthma continue to grow steadily.1
Allergic diseases occur throughout the lifespan, but often have their origins in childhood. Infants and young children are often sensitized to foods and other macromolecules absorbed through the gut, and develop a variety of hypersensitization symptoms such as colic and eczema. These sensitivities can be enhanced by maternal food allergies, and these allergies have been demonstrated to be transmitted placentally. Among these atopic children, exposure to aeroallergens over the first few years of life often causes additional sensitization, resulting in the development of upper respiratory allergy and the condition known as allergic rhinitis. Allergic rhinitis also has a very strong genetic predisposition, with up to two-thirds of children with both parents suffering from allergic rhinitis also demonstrating symptoms of this disease. Concurrent with the development of allergic rhinitis is a rise in IgE levels in children. As will be discussed later in this chapter, IgE is the immunoglobulin involved in the immune response, and levels of IgE become significant in allergic children after the age of 2 years. Allergic rhinitis is quite common in childhood, with studies suggesting that up to 40% of children may be diagnosed by their physician with allergic rhinitis by the age of 6 years.
This progression of allergic disease from food-mediated colic and eczema, to allergic rhinitis, and finally to asthma has been referred to as the allergic march, implying that allergic disease will continue to progress in a steady manner from early childhood into adulthood.2 It is unclear at this time whether early aggressive intervention can prevent or blunt this progression of disease. It is clear, however, that this allergic march is common in many children with atopic disease.
Burden of Allergic Diseases
For example, allergic rhinitis has been demonstrated to affect a daytime function in both children and adults.3,4 These studies suggest that over 90% of children and adults have noted disruption in their abilities to work productively in the workplace or in the school when their rhinitis is symptomatic. Nearly one in four of these adults and children have missed work or school due to their symptoms. These findings demonstrate that allergic rhinitis is not only bothersome in terms of its adverse symptoms, it will impact the ability of adults and children to perform the general activities of their daily living, such as work and school attendance. Similar findings have been reported in a number of studies.
In addition, in patients with allergic rhinitis, the presence of the disease impacts on other aspects of function. Children with allergic rhinitis learn less effectively than those without the disease.5 Adults and children with allergic rhinitis have difficulty falling asleep and staying asleep.6 Furthermore, many of the older treatments for allergic rhinitis, particularly the first-generation antihistamines such as diphenhydramine, further adversely affect quality of life and function through their sedating and anticholinergic side effects.7
While the effects of upper airway allergy on function and quality of life can be significant, the adverse effects of asthma are even more dramatic. Asthma is a disease that is often poorly treated, due to a variety of factors including poverty, delay in diagnosis, inappropriate treatment, and patient nonadherence. It affects sleep, learning, daytime function, and has a significant negative impact on quality of life. Asthma deaths continue to number around 180000 annually on a worldwide basis, with delay in diagnosis and inadequate treatment being primary driving factors.8
Comorbidities of Allergic Diseases
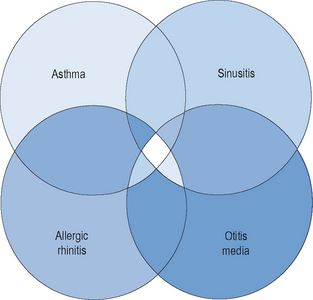
The majority of allergic diseases affect the upper and lower respiratory tracts. Respiratory illnesses that have a very direct allergic pathogenesis include allergic rhinitis and asthma. Other respiratory illnesses such as otitis media and acute and chronic rhinosinusitis have significant elements of allergy, at least in the expression of their symptoms, and perhaps in their pathogenesis as well (Figure 1.1). Among patients with allergic rhinitis, both adults and children, there is a greater prevalence of these other allergic illnesses than in the nonallergic population. In addition, among patients with allergic rhinitis, there is a higher likelihood of the development of rhinosinusitis, asthma, and otitis media than in patients who do not have allergic rhinitis. For that reason, the presence of allergy must be considered in any individual who presents with chronic respiratory symptoms, either upper or lower.
Over the past decade, an awareness of the close interrelationship between upper and lower airway inflammatory diseases has been appreciated. Due to similarities in epithelial cells and membranes, inflammatory mediators, and pathophysiological mechanisms, the entire airway has been conceptualized as a unified system. It has been observed that diseases that affect one portion of this airway system will often affect other respiratory sites as well. This observation has led to a model described as the “unified airway model,” also known as the model of “one airway, one disease.”9,10 Allergic rhinitis and asthma, therefore, are considered diseases along a pathophysiological spectrum, whose mechanisms exert similar influences in discrete portions of a unified airway system. This model has been useful conceptually, in explaining many observations of concurrent inflammation in both the upper and lower airway.
In 2000, the World Health Organization brought together an international panel of experts to examine the association between upper and lower airway inflammatory diseases. This panel issued a consensus document known as the ARIA document (Allergic Rhinitis and its Impact on Asthma). In the ARIA guidelines, the close association between allergic rhinitis and asthma was detailed, with specific recommendations for treatment of these coexisting diseases. The document stated “The upper and lower airways may be considered as a unique entity influenced by a common, evolving inflammatory process, which may be sustained and amplified by interconnected mechanisms.” In addition, it went on to argue that “When considering a diagnosis of rhinitis or asthma, an evaluation of both the upper and lower airways should be made.”11
Basic Immunology
The term “immune” is derived from the Latin word immunitas that refers to the specific exemption that was granted to Roman senators in their state duties. This concept is carried forward into today’s legal system, where witnesses can be given immunity from prosecution for cooperating with a criminal investigation. In health and disease, the immune system is designed to provide this same exemption or protection through preventing or limiting the effects of the disease on the organism. The immune system has a number of properties, which are detailed in Box 1.1.