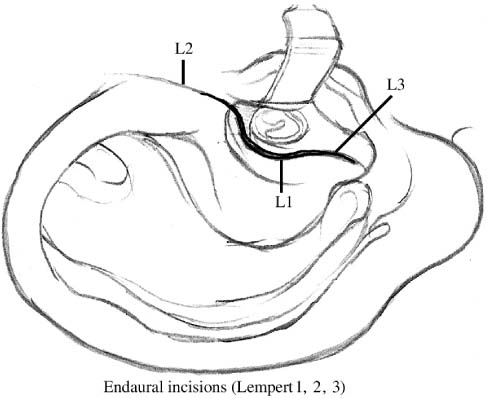
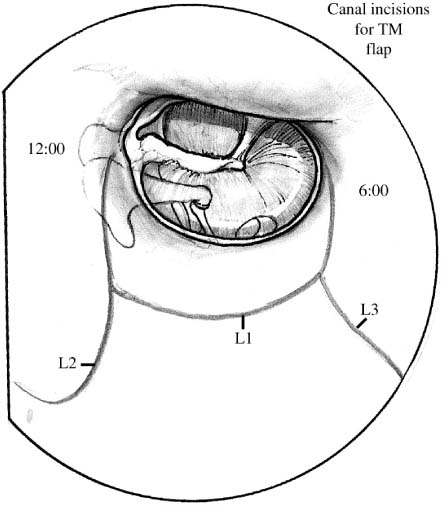
Chapter 10 From about 1965 to 1985, many otologists, notably Sheehy and Patterson,1 Jansen,2 and Smyth,3 recommended either the closed-cavity, intact-wall tympanomastoidectomy or a combined approach, accomplishing each approach usually in two or three stages. First the pathologic conditions were eradicated, then 8 to 12 months later the hearing apparatus was reconstructed via tympanoplasty; sometimes a separate exploratory procedure later searched for residual cholesteatoma. At the First International Conference on Cholesteatoma (held in Alabama in 1977), McCabe and colleagues4 noted rising enthusiasm for two-stage techniques using intact-canal-wall mastoidectomy. Farrior5 and Papar-ella and Kim6 recommended occasional selection of an intact-canal-wall tympanomastoidectomy, depending on existing anatomic and pathologic findings in each patient. By 1982, when the Second International Conference on Cholesteatoma was held in Tel Aviv, discussion had reverted to the high rate of recurrent or residual cholesteatoma found with intact-wall procedures,7 requiring revision of the surgery in 38.1%, compared with 9.4% for open procedures. Recommendations swung back to open-cavity techniques. Brown,8 comparing 1142 consecutive cases of cholesteatoma treated surgically with open and with closed techniques, concluded that closed methods produced better hearing results but higher rates of recurrence. In Paparella and Kim’s6 study, most patients with chronic otitis media and mastoiditis had sclerotic and hypocellular mastoids. On the basis of this observation, Paparella and Jung9 developed a surgical technique called the intact-bridge tympanomastoidectomy (IBM) procedure. This procedure produced excellent long-term results by preserving desirable elements of both open-cavity (intact canal-wall) and closed-cavity (canal-wall-down) techniques, allowing eradication of diseased tissue, better reconstruction of the middle ear and ossicles, enhanced tympanoplastic methods, and enhanced obliteration of the mastoid (when indicated), all within a single stage. From then on, Paparella and Sajjadi have performed more than 1200 IBM procedures with excellent results. It remains the treatment of choice for chronic otitis media and mastoiditis where there is a canal wall or bridge.10 The IBM is indicated for patients with chronic otitis media and mastoiditis, intractable cholesteatoma, cholesterol granuloma, or granulation tissue in the mastoid, middle ear, or attic, either as a first operation or, if there has been prior surgery, to revise where the earlier procedure has left an intact posterior canal wall or bridge. Because most patients with chronic otitis media and mastoiditis do have small, sclerotic, hypocellular mastoids, they are ideal candidates for the IBM.11 In the rare patient with a well-pneumatized mastoid, excellent results can be obtained by adding some techniques from combined-approach tympanoplasty to the intact-canal-wall tympanomastoidectomy. For the most difficult cases of severely contracted, sclerotic mastoids, however, an intact-canal-wall tympanoplasty may be unnecessarily hazardous even in the hands of experts and it does not offer much alleviation of open-cavity postoperative problems. The IBM techniques result in a very small cavity. In a well-pneumatized mastoid, a postauricular incision is used to expose mastoid and middle ear; sometimes, if the meatus is small, a limited endaural incision is added. In the more frequent sclerotic or diploic mastoid, however, Lempert endaural incisions I, II, and III are begun 5 to 7 mm from the tympanic annulus in the bony ear canal (Fig. 10–1). Then incisions are made at the 6 o’clock and 12 o’clock positions with a sickle knife, and a No. 1 knife at the tympanic annulus, to connect with the Lempert I and delineate a tympanomeatal flap (Fig. 10–2). The flap is separated from the mastoid flap at the Lempert I incision, using a duck-billed knife/elevator, and is elevated down to the annulus, but the middle ear is not yet entered. A Lempert elevator is used to further elevate the Lempert I incision with the mastoid flap, and the mastoid flap is put inside a self-retaining retractor with a Penrose drain between retractor and flap to protect the integrity of the flap (Fig. 10–3). Then from the Lempert II incision, with self-retaining retractors, we harvest temporalis muscular fascia, put it into a fascial press for 10 minutes, and then open the press and allow it to air-dry. Most patients with chronic otitis media have small external ear canals that bulge into the anterior and often also the posterior canal. Generous canaloplasty, tailored to each patient, is usually required. Using self-retaining retractors, skin of the anterior canal is elevated in a laterally based flap, and skin of the posterior canal in a medially based flap. A high-speed cutting drill under suction/irrigation is used to enlarge the circumference of the posterior canal, removing the spine of Henle and all overhangs to achieve a straight, direct, unobstructed approach to the tympanic annulus (Fig. 10–4). If there is prominent bulging into the anterior canal that obscures the view of the drumhead, an incision is made in the anterior canal with a No. 2 knife lateral to the tympanic annulus in a semicircle from the 6 o’clock to 12 o’clock positions. The skin of the anterior canal is very carefully elevated using a duck-billed knife/elevator; then just past the bone cartilage junction a thin skin flap is carefully raised with a larger, round, duller periosteal elevator (Fig. 10–5), being careful not to amputate the flap. A high-speed cutting drill with suction/irrigation is then used to make two grooves in the anterior canal wall, inferiorly and superiorly, and then connect them with drilling. This allows full visualization of the anterior drumhead by removing the bulge in the canal. Apparent distance to the temporomandibular joint may be deceptive, so care must be taken not to enter the joint or, if its endosteum is entered, to cease drilling. FIGURE 10–1 Lempert incisions. FIGURE 10–2 Canal incisions and tympanomeatal (TM) flap. In most of these patients, intractable cholesteatoma or granulation tissue in a sclerotic mastoid indicates that the surgeon should proceed directly to mastoidectomy, but in a few patients the status of the mastoid is unclear. For these patients, mastoidotomy, either through the posterior wall of the ear canal through a small opening or under Macewen’s triangle if preoperative radiographs show adequate pneumatization, can help safely identify the extent of the pathologic tissue. In extremely sclerotic mastoids, mastoidotomy is not indicated.
INTACT-BRIDGE MASTOIDECTOMY: A VERSATILE ONE-STAGE OPERATIVE TECHNIQUE
SURGICAL TECHNIQUE
INCISION
CANALOPLASTY
OPTIONAL MASTOIDOTOMY
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree