Inferior Oblique Muscle Surgery
Cynthia L. Beauchamp
David R. Stager
Paul R. Mitchell
Marshall M. Parks, M.D., once described the inferior oblique as the last bastion of motility disorders to be conquered. He and Leonard Apt, M.D., have inspired our interest in surgery of this muscle and its nerve. When describing his technique for locating the nerve to the inferior oblique, Dr. Parks stated that it could be located easily following disinsertion and anterior traction on the insertion of the muscle by “strumming” the inferior oblique nerve as it approached the inferior oblique near the temporal border of the inferior rectus. His description has led many to be curious about the nature of this nerve and has led to a great deal of research on the nerve and muscle over the last two decades.
The history of inferior oblique muscle surgery has been reviewed in detail by Dyer,1 Parks,2 and Weakley and Stager.9 Various inferior oblique strengthening procedures have been described,4,5,6,7,8 but they are no longer useful or recommended. Therapy for inferior oblique underaction includes techniques that involve the antagonist superior oblique muscle or the contralateral yoke muscle,9,10 and they are not discussed here.
This chapter discusses surgery on the inferior oblique muscles for primary inferior oblique overaction, secondary inferior oblique overaction associated with palsy of the ipsilateral superior oblique or contralateral superior rectus, A and V patterns, and dissociated vertical deviations. More detailed and thorough descriptions of the etiology, diagnosis, and management of these conditions are provided in other chapters.
ANATOMY
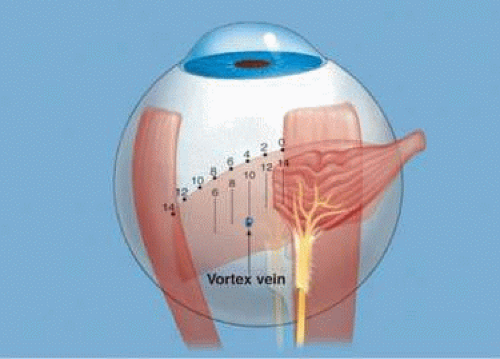
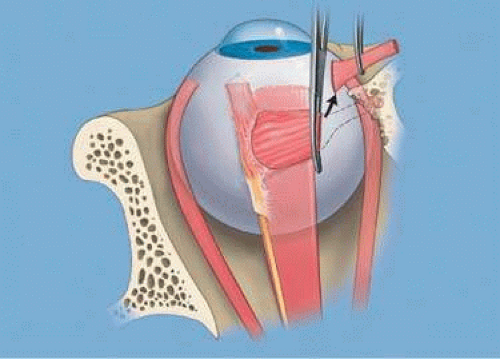
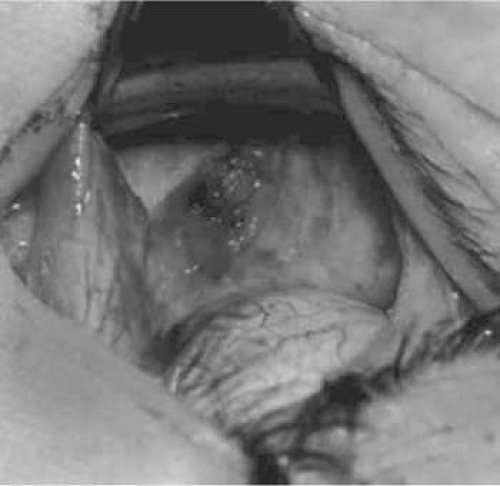
In discussing surgery to the inferior oblique, one needs to first address the anatomy of the inferior oblique and the nerve to the inferior oblique (Fig. 87-1). The inferior oblique muscle measures 37 mm in length. It originates just posterior to the nasal aspect of the inferior orbital rim where the muscle is narrow, measuring about 5 mm in its anterior posterior diameter. The nasal aspect measures about 13 mm in length. About 3 mm nasal to the inferior rectus, the muscle expands in its anterior posterior diameter to become about 10 mm wide. The mid portion of the muscle crosses the underside of the inferior rectus muscle for the next 10 mm. The temporal portion of the inferior oblique measures about 14 mm in length and inserts on the sclera near the lower border of the lateral rectus muscle in the inferior temporal quadrant of the globe. The nerve to the inferior oblique, a branch of the inferior division of the third cranial nerve, enters the muscle approximately 2 mm temporal to the lateral border of the inferior rectus at its posterior border.
Some variability in the muscle may exist. De Angelis et al11 performed a cadaver study of 100 eyes. Multiple insertions were found in 17% of inferior oblique muscles examined; duplications of the inferior oblique muscle belly located at 10 to 12 mm from the insertion were found in 8%. The mean muscle width among these eight specimens was larger than normal muscles.
It is important to be aware of the surrounding layers of the inferior oblique. Nasally, the muscle is surrounded by a rather significant capsule and is located outside the intermuscular septum. Outside the capsule is the fat pad. In the midportion, the inferior oblique is surrounded by both its capsule, a thickened portion of Lockwood ligament, and Demers ligament on its superior surface. On the inferior surface, it is covered by the Tenon capsule. Temporally, the muscle is surrounded by a thin muscle capsule, the intermuscular septum, and the Tenon capsule. External to that is the orbital fat pad.
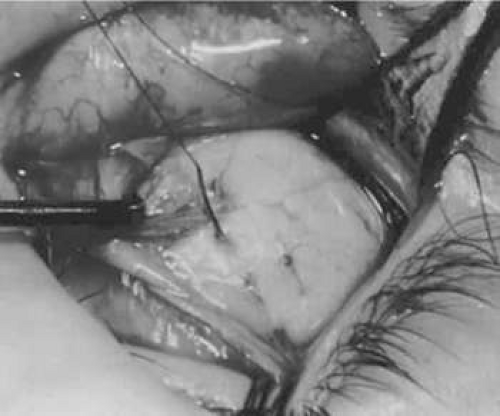
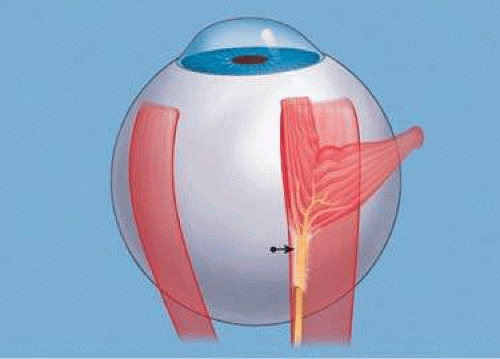
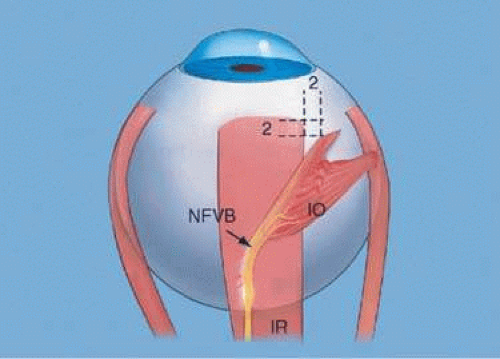
Much study has been done on the nerve to the inferior oblique12 (Fig. 87-2). It lies in a straight line to the apex of the orbit just temporal to the lateral border of the inferior rectus. The stiffness of the nerve is derived from the capsule of the nerve. It is composed of collagen fibers that are aligned parallel to the axis of the nerve, giving the muscle the stiffness of which Dr. Parks originally spoke. Tension studies show that it is five times as stiff as the superior oblique tendon. This provides an ancillary origin for the posterior temporal fibers of the inferior oblique muscle when the insertion is transposed anteriorly.12
EXPOSURE TECHNIQUE
All inferior oblique surgery requires the same initial steps to the point of isolation of the inferior oblique muscle (Figs. 87-3–87-13). At that time, any one of several procedures can be performed (Figs. 87-12–87-41). These procedures are described individually. The figures are presented from the view of the surgeon seated at the head of the patient.
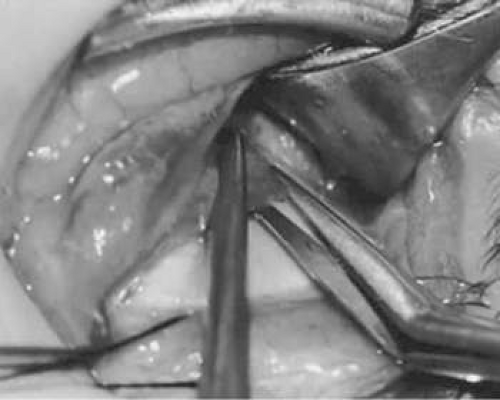
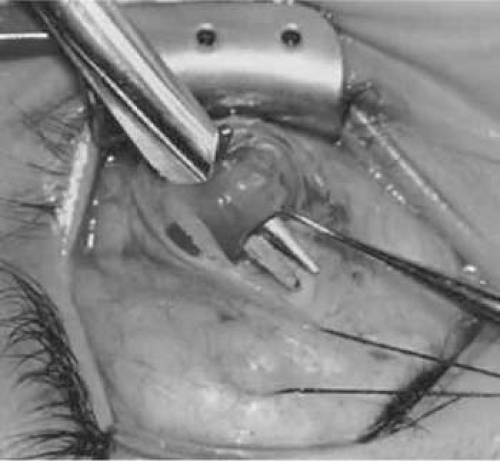 Figure 87-8. A Westcott scissor is used gently to open a space beneath the elevated inferior oblique muscle and allow placement of a Green muscle hook. |
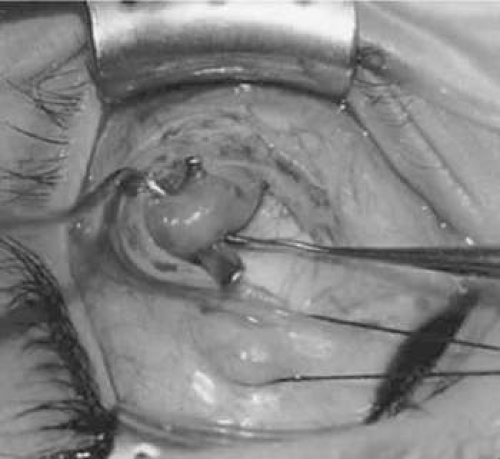 Figure 87-9. The Green muscle hook is placed beneath the belly of the inferior oblique muscle, and the eye is retracted nasally. |
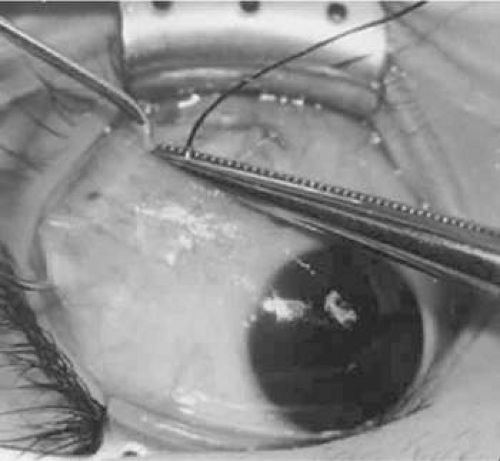
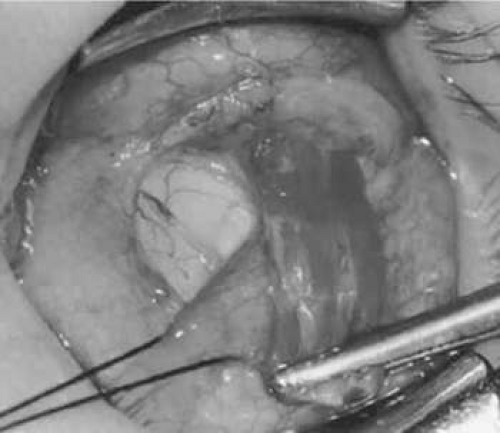
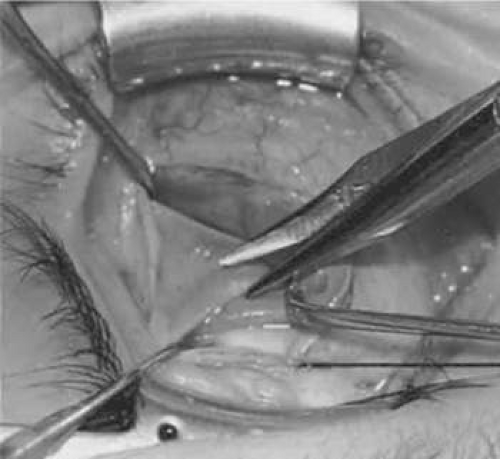 Figure 87-10. A Westcott scissor is used to dissect the intermuscular septum and expose the insertion of the inferior oblique muscle. |
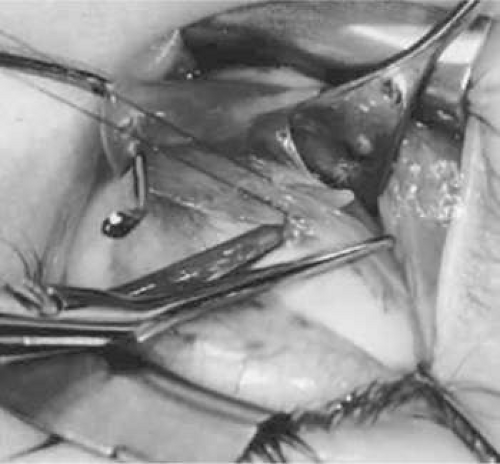 Figure 87-12. An Aebli scissor is placed at the inferior oblique muscle insertion and it is tenotomized from the globe. In this photo, a suture has been preplaced. We prefer the use of the Beauchamp clamp near the insertion allowing the suture to be placed once the muscle has been tenotomized from the globe. The placement of a vascular clamp along the insertion is seen in Figures 87-25 and 87-26. |
 Figure 87-13. The oblique is sectioned from the globe with the 6-0 Vicryl suture attached to the insertion. |
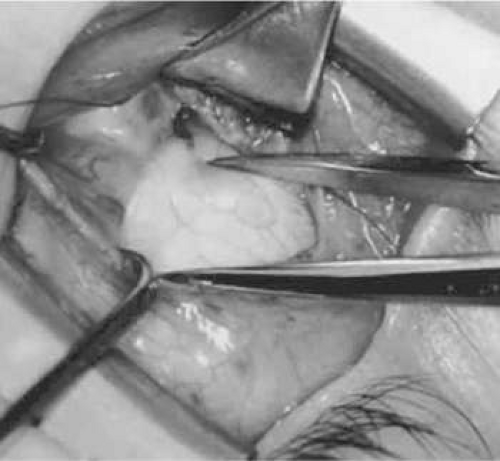 Figure 87-14. The inferior temporal vortex vein, 8 mm posterior to the temporal insertion of the inferior rectus muscle, is held on a Green muscle hook. |
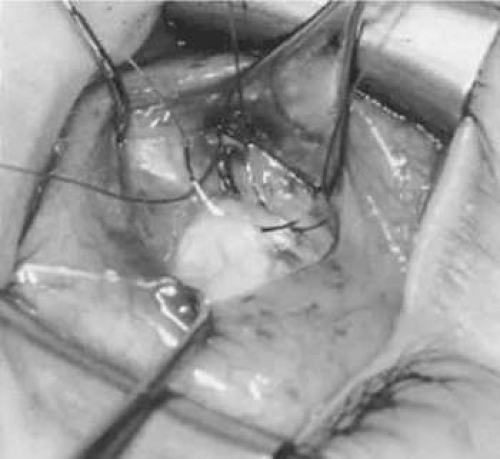 Figure 87-15. Two sutures straddle the inferior temporal vortex vein insertion for a 10-mm recession procedure. |
 Figure 87-16. Knots are tied to show the placement. The inferior oblique muscle is held on a Stevens muscle hook. |
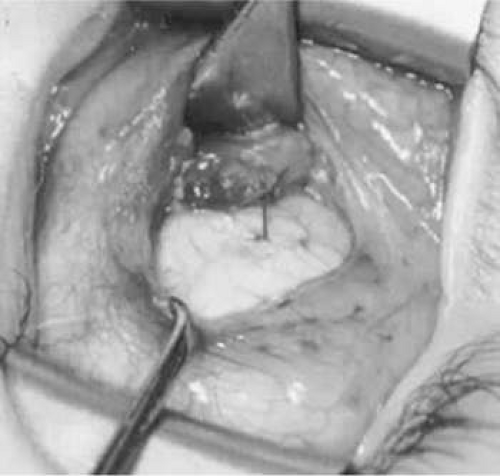 Figure 87-17. A 10-mm inferior oblique muscle recession is placed over the inferior temporal vortex vein. |
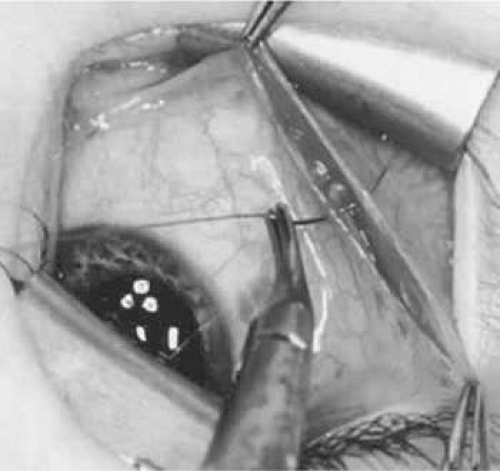 Figure 87-18. Optional closure of the incision with a 6-0 Vicryl suture. The incision may be allowed to heal without a suture. |
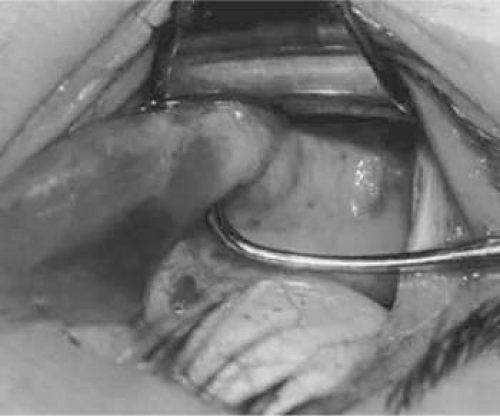
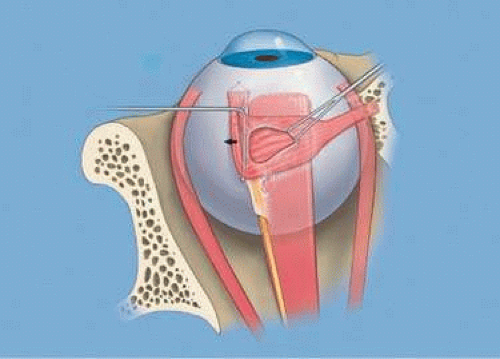 Figure 87-21. A double hook is placed inside the opening of the capsule to expose the inferior oblique muscle belly. |
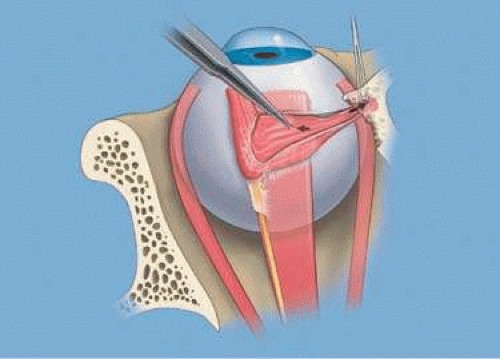 Figure 87-22. The inferior oblique muscle is grasped with Bishop-Harman forceps as the double hook is drawn nasally to expose the nasal portion of the muscle. |
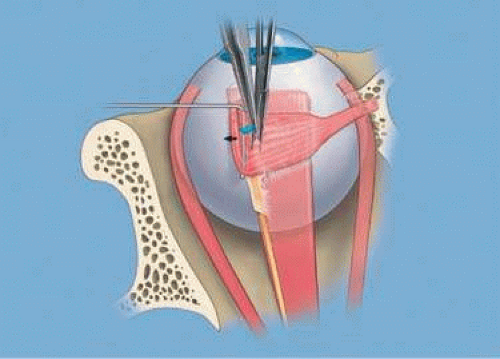
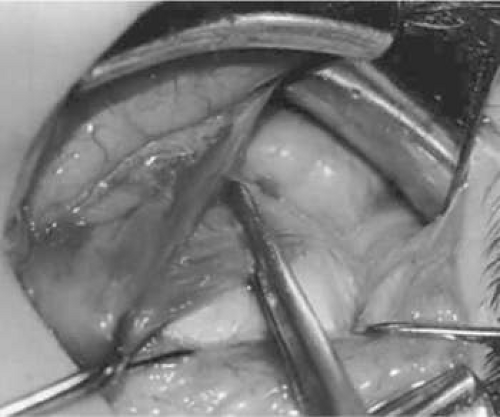 Figure 87-25. The following photographs depict a denervation and extirpation procedure (Figs. 87-25–87-36). A hemostat is placed adjacent to the insertion of the right inferior oblique muscle. |
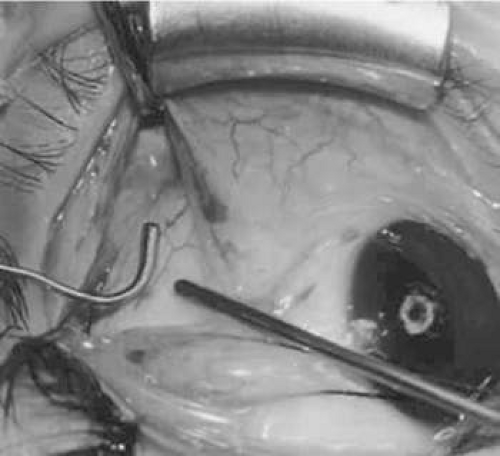
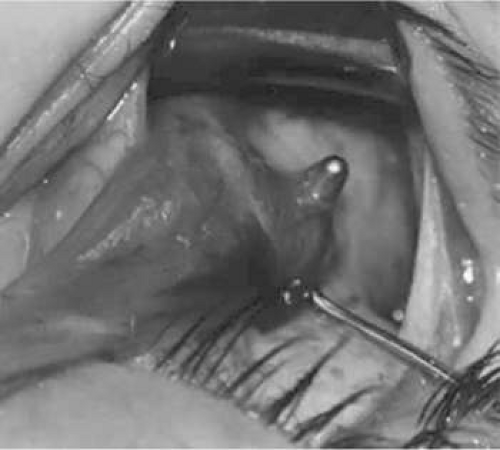 Figure 87-29. The hook is advanced farther for identification of the neurovascular bundle on the inferior oblique muscle. |
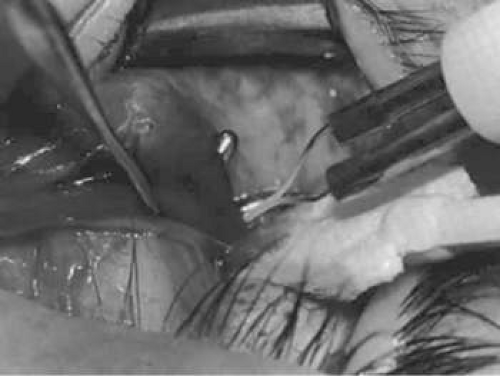 Figure 87-30. Cautery is applied to sever the neurovascular bundle, and a sponge is used to protect the sclera and lids from cautery. |
 Figure 87-32. The inferior oblique muscle is drawn farther into the operative field, and a 3-0 Vicryl suture ligature is applied about the belly of the muscle. |
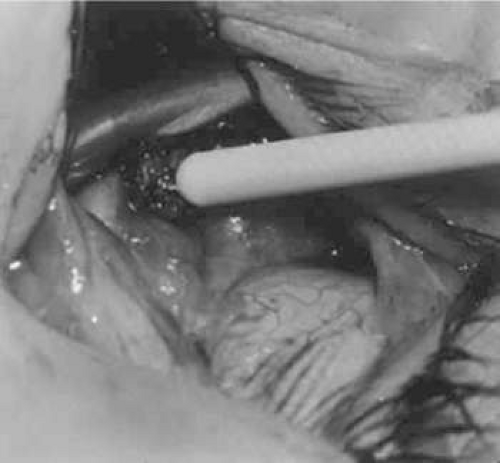 Figure 87-34. The stump of muscle is placed through the Tenon capsule opening. The surgeon must apply sufficient cautery to prevent postoperative bleeding. |
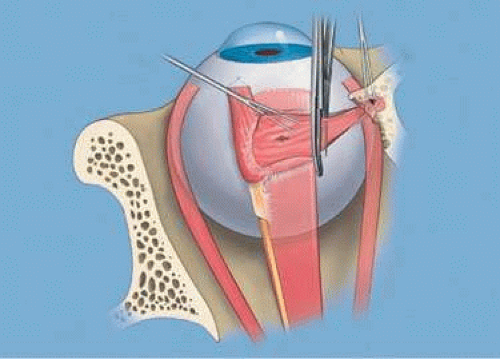
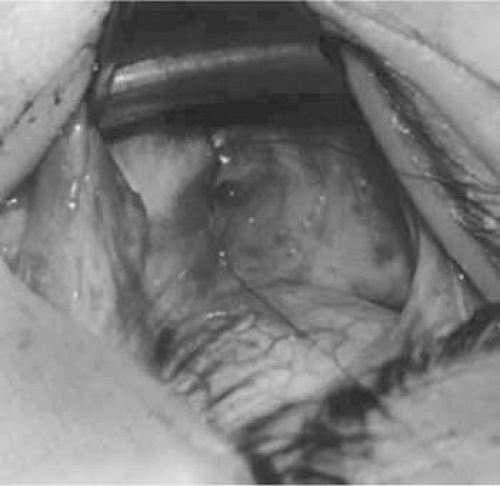 Figure 87-36. The Tenon capsule opening is closed with 6-0 or 7-0 Vicryl suture to place the inferior oblique muscle entirely outside Tenon capsule. |
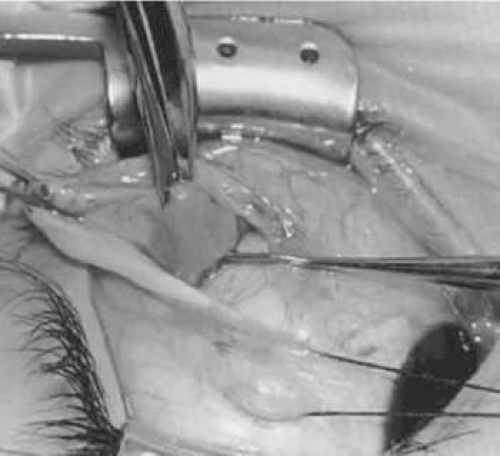
 Figure 87-37. The following photographs depict an anterior transposition procedure (Figs. 87-37–87-39). A 6-0 Vicryl suture is placed in the inferior oblique muscle in preparation for anterior transposition. A Green muscle hook is placed beneath the inferior rectus muscle. |
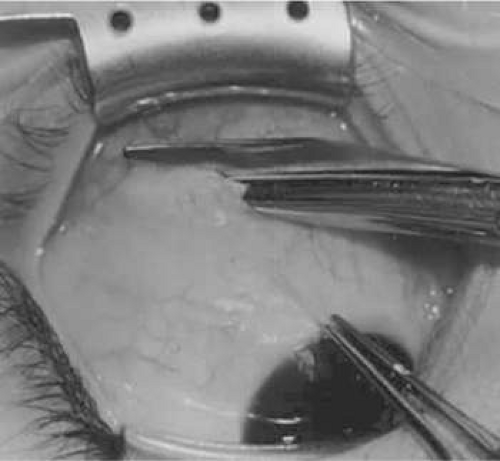
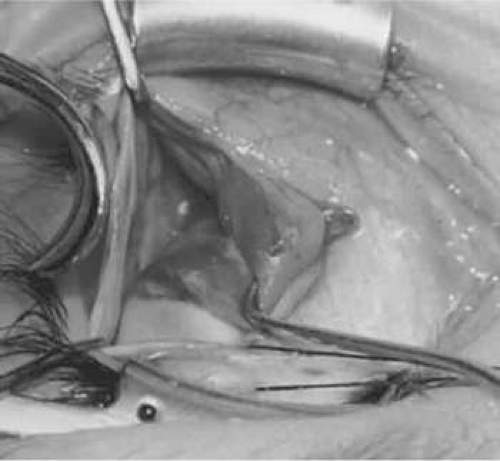
The inferior oblique is exposed through an inferior temporal cul-de-sac incision down to bare sclera (Fig. 87-3). The lateral rectus is isolated on a muscle hook and the eye is rotated nasally and superiorly (Fig. 87-4). The lateral portion of the incision is retracted inferior temporally with a double hook. A Bishop-Harman forceps grasps the anterior part of the inferior oblique temporally and pulls it forward. A Von Graefe hook is then passed posteriorly along the sclera, which is retracted nasally, as the muscle is pulled laterally and anteriorly. The posterior border of the inferior oblique can then be identified where the white intermuscular septum contrasts with the red inferior oblique muscle (Fig. 87-5). The hook is rotated under the inferior oblique with the point temporally and this then is pulled forward, taking care to isolate all the fibers of the muscle (Fig. 87-6). Excessive intermuscular septum and Tenon capsule must be separated and lifted off, and then an incision is made in the tissue to expose the tip of the hook. A second hook is placed through that opening and the two hooks are separated. The posterior portion of the intermuscular septum and Tenon capsule are retracted temporally with a Jameson hook while the muscle is retracted nasally. The second hook under the inferior oblique is repositioned under the lower border of the lateral rectus posteriorly, near the inferior oblique insertion. The tissue between the muscle and the fibrous tissue is cut with scissors (Figs. 87-7–87-10). Care must be taken to ensure there is no evidence of inferior oblique muscle that has been missed. If that does occur, one needs to go back and repeat the procedure to be certain that the entire inferior oblique is properly identified and isolated on the hook. The inferior oblique is thus exposed and ready for a myotomy, myectomy, disinsertion, recession, or extirpation (Fig. 87-11). A Beauchamp clamp, which has the advantage of holding the muscle without crushing the tissue, is then placed near the insertion of the inferior oblique and the muscle is then disinserted close to the sclera13 (Figs. 87-12 and 87-13).
SURGICAL PROCEDURES
Currently, tightening the inferior oblique surgically has not received any significant acceptance as a surgical option although some work had been done combining resection with anterior transposition with promising results.14,15 In the future, this may change as newer options become available to chemically tighten the muscle fibers. Chemically weakening the inferior oblique muscle fibers with botulinum toxin (Botox) has not become an acceptable alternative, perhaps due to the thinness and close proximity to the sclera, which has made this more hazardous. However, early studies have suggested promising results. Garnham et al16 retrospectively reviewed 20 patients who received botulinum injections in either the inferior oblique or inferior rectus for superior oblique palsy. They found the greatest benefit to patients with residual deviations following previous surgery, particularly when the inferior rectus was injected. Eighty-three percent of the patients receiving botulinum as a primary therapy required further surgery. In a prospective case series, Bagheri and Eshaghi17 injected botulinum toxin into the inferior oblique in 18 eyes with acute superior oblique palsies. At 6 months, they found a reduction in hyperdeviation, cyclodeviation, head tilt, and inferior oblique overaction. They concluded that botulinum toxin is a viable option for acute superior oblique palsies as patients await recovery.
In the future, other substances may also become available to inject into the muscle under direct vision to weaken the action. In a prospective study of 20 patients, Nemet18 found success with injecting acetylcholine following myectomy to prevent reattachment and recurrence.
Currently, surgical procedures that are performed on the inferior oblique muscles include recession, temporal myotomy, myectomy, nasal myectomy, disinsertion, denervation, denervation and extirpation, and anterior transposition.19 The decision on surgical options will depend to a great extent on the activity of its antagonist, the superior oblique muscle and its tendon. The effect of the superior oblique on the globe may vary from a mild underaction to a severe underaction, or perhaps even an absence or transposition of the superior oblique tendon to an ineffective location. Weakness may be permanent or temporary due to involvement of the fourth cranial nerve. Therefore, it is important in making a decision to weaken the inferior oblique that one has a complete history of the permanent nature of this imbalance between the opposing superior and inferior oblique muscle complex.
Recession
In comparing the various weakening procedures, Parks2,20 concluded that the recession procedure was superior (Figs. 87-14–87-18). The major advantage of the recession is that it allows the weakening procedure to be titrated according to the severity of the overaction (Fig. 87-19). For 1+ or 2+ overaction, the inferior oblique muscle is recessed 10 mm for 3+ overaction, 12 mm; and 4+ overaction, 14 mm, which is the maximum recession. A double-armed 6-0 synthetic suture, such as polyglactin (Vicryl [J-562], Ethicon, Somerville, NJ) with a half-circle spatula needle (S-28, Ethicon, Somerville, NJ), is placed within the insertion of the inferior oblique with a locked bite at the anterior and posterior border after the muscle is tenotomized, as described previously. The muscle is recessed 10 mm by placing the anterior suture 6 mm posteriorly to the lateral border of the inferior rectus muscle insertion and 4 mm temporal to the lateral border of the inferior rectus (approximately at the vortex vein) (Figs. 87-15 and 87-17). Recessions of 12 and 14 mm are placed in relationship as depicted by the figure, farther along the course of the inferior oblique muscle (Fig. 87-19). Metten et al21 studied the dose-response curve for recession and confirmed a dose-response relationship, with large vertical deviations with small excyclodeviation benefitting from increased anteropositioning. The study of Apt and Call22 on the pathway of the temporal portion of the inferior oblique has shown differences in what constitutes a 6- to 14-mm recession along the path of the muscle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree