Recent improvements in serum Tg assays, the availability of recombinant thyrotropin, widespread use of neck ultrasonography, and positron emission tomography (PET)/CT have caused a shift of paradigm in the detection of recurrent disease in well differentiated thyroid cancer. High-resolution neck ultrasonography has taken on a central role, whereas 131 I whole body scanning has become less important. PET/CT has emerged as a powerful tool in the assessment of patients who have recurrent tumor not demonstrable with other imaging modalities. The author reviews the tools available for the detection and localization of recurrent thyroid cancer with respect to their advantages and limitations in various clinical scenarios.
More than 20,000 new thyroid cancers are diagnosed in the United States every year, with approximately 1000 cancer-related deaths . Papillary thyroid carcinoma and its follicular variant account for 80% to 90% of all primary thyroid cancers . Follicular and Hurthle cell cancers comprise 5% to 10%, medullary thyroid cancer 5%, and anaplastic cancer less than 1% of all thyroid malignancies. Several variables can collectively determine the risk for dying from papillary thyroid cancer . These variables include age (>45), distant metastases, completeness of resection, invasion of contiguous structures (trachea, strap muscles, nerves, esophagus), and size of tumor (>4 cm) . Papillary thyroid carcinoma, in general, has an excellent prognosis. Eighty percent to 85% of papillary thyroid cancers can be classified as low risk, associated with a 20-year cause-specific mortality of less than 1% with proper treatment . High-risk thyroid cancer, on the other hand, is a deadly disease. The recurrence rate of thyroid cancer is as high as 30% in some series. However, recurrent disease can be treated effectively. The preferred treatment of local-regional recurrence is surgical excision, often combined with radioactive iodine ablation. Therefore, it is critically important to establish the presence of recurrent disease and its location. About 85% of patients who have recurrence have cervical nodal metastasis, 32% have local recurrence in the thyroid bed, and 12% have distant metastasis. The overall recurrence rate is higher for follicular cancer than for papillary. The rate of distant metastasis is also higher for the follicular carcinoma. Traditionally, the primary modality for detection of disease recurrence was 131 iodine (I) scanning. The ability to measure thyroglobulin (Tg) accurately has brought about a major paradigm shift in the management of thyroid cancer, with greater reliance on serum thyroglobulin and neck ultrasonography (US), and less emphasis on routine diagnostic whole-body radioactive iodine scanning for detection of recurrent disease.
The author reviews the tools available for the detection and localization of recurrent thyroid cancer with respect to their advantages and limitations in various clinical scenarios.
Thyroglobulin
After total thyroidectomy, no Tg should be detectable in the serum. The presence of Tg indicates residual thyroid tissue or recurrence . Tg production by residual thyroid tissue is usually suppressed with thyroid suppression but malignant cells can produce Tg autonomously. The magnitude of Tg levels may be related to tumor mass, degree of differentiation, and location of metastasis . Low levels of Tg, 1 ng/mL or less, provide a sensitive test, whereas higher cut-off levels result in a greater specificity at the expense of decreasing sensitivity in detection of recurrent cancer . Thyroid suppression and withdrawal of suppression influence the serum Tg levels. Measurements after withdrawal of thyroid suppression afford greater sensitivity but lesser specificity. Thyrotropin stimulates Tg production. Recombinant human thyrotropin stimulation can be used to increase test sensitivity, instead of thyroid suppression withdrawal . Most patients who have thyroid cancer in whom the serum Tg level after primary treatment is undetectable have a low risk for recurrence, from less than 0.5% to 1.6% over a period of 5 to 12 years of follow-up . Tg surveillance as the sole screening test for recurrent thyroid cancer may suffice in a subset of patients who have low risk and no evidence of recurrence on prior 131 I scan, although in unselected populations, a combination of Tg with an imaging modality is necessary to increase accuracy. Once the presence of recurrence is established, the location of recurrence must be defined for treatment planning.
131 I whole body scan
Until recently, 131 I whole body scan (WBS) had been at the center of recurrent thyroid cancer detection . Naturally, it detects iodine-avid cancers and is ineffective in undifferentiated tumors. Typically, an oral dose of 1 to 5 mCi of 131 I is administered and followed 2 to 4 days after by whole body scanning. Double-headed gamma cameras equipped with high-energy collimators yield superior images. One distinct advantage of WBS over other imaging modalities is its ability to identify distant metastatic disease. The amount of residual normal thyroid tissue affects the sensitivity of the test. Better results are achieved with little or no residual thyroid. Similar to Tg, 131 I WBS becomes more sensitive after thyroid suppression withdrawal and thyrotropin stimulation. Also, higher doses of iodine increase sensitivity. The reported diagnostic performance of 131 I WBS varies widely among studies and select patient groups. The differences among the patient risk groups and prior therapies involved make interpretation of many studies difficult. Most studies with a large group of unselected patients report a sensitivity of 50% to 60% for 131 I WBS in detecting recurrent thyroid cancer, whereas the specificity is more than 90% . 131 I WBS in conjunction with serial Tg measurements provides a robust tool in thyroid cancer follow-up. Poor visibility of anatomic landmarks is an inherent disadvantage of 131 I. Although an approximate localization of recurrent thyroid cancer is achieved, this approximation is often insufficient for the difficult reoperation in the neck. Before surgical intervention, a more precise localization with anatomic imaging modalities is needed, which makes the value of 131 I questionable. Because most recurrences occur in the neck nodal chains or thyroid bed, which can be evaluated effectively with US, Tg coupled with serial US examinations recently emerged as the preferred method for follow-up of differentiated thyroid cancer.
Many patients who have thyroid cancer are treated soon after surgery with radioiodine ablation for potential residual and metastatic disease, which allows an opportunity for imaging. Four to 6 weeks after the administration of a therapeutic dose of 131 I, WBS is performed, which provides a baseline documentation of the extent of disease.
Other radiolabeled compounds, such as 123 I, 201 thallium, and 99m technetium tetrofosmin, can be used instead of 131 I . Noniodine agents do not require thyroid suppression withdrawal or thyrotropin stimulation and may be preferable in patients who have substantial amounts of residual thyroid tissue, although their performance is usually not better than 131 I.
131 I whole body scan
Until recently, 131 I whole body scan (WBS) had been at the center of recurrent thyroid cancer detection . Naturally, it detects iodine-avid cancers and is ineffective in undifferentiated tumors. Typically, an oral dose of 1 to 5 mCi of 131 I is administered and followed 2 to 4 days after by whole body scanning. Double-headed gamma cameras equipped with high-energy collimators yield superior images. One distinct advantage of WBS over other imaging modalities is its ability to identify distant metastatic disease. The amount of residual normal thyroid tissue affects the sensitivity of the test. Better results are achieved with little or no residual thyroid. Similar to Tg, 131 I WBS becomes more sensitive after thyroid suppression withdrawal and thyrotropin stimulation. Also, higher doses of iodine increase sensitivity. The reported diagnostic performance of 131 I WBS varies widely among studies and select patient groups. The differences among the patient risk groups and prior therapies involved make interpretation of many studies difficult. Most studies with a large group of unselected patients report a sensitivity of 50% to 60% for 131 I WBS in detecting recurrent thyroid cancer, whereas the specificity is more than 90% . 131 I WBS in conjunction with serial Tg measurements provides a robust tool in thyroid cancer follow-up. Poor visibility of anatomic landmarks is an inherent disadvantage of 131 I. Although an approximate localization of recurrent thyroid cancer is achieved, this approximation is often insufficient for the difficult reoperation in the neck. Before surgical intervention, a more precise localization with anatomic imaging modalities is needed, which makes the value of 131 I questionable. Because most recurrences occur in the neck nodal chains or thyroid bed, which can be evaluated effectively with US, Tg coupled with serial US examinations recently emerged as the preferred method for follow-up of differentiated thyroid cancer.
Many patients who have thyroid cancer are treated soon after surgery with radioiodine ablation for potential residual and metastatic disease, which allows an opportunity for imaging. Four to 6 weeks after the administration of a therapeutic dose of 131 I, WBS is performed, which provides a baseline documentation of the extent of disease.
Other radiolabeled compounds, such as 123 I, 201 thallium, and 99m technetium tetrofosmin, can be used instead of 131 I . Noniodine agents do not require thyroid suppression withdrawal or thyrotropin stimulation and may be preferable in patients who have substantial amounts of residual thyroid tissue, although their performance is usually not better than 131 I.
Ultrasonography
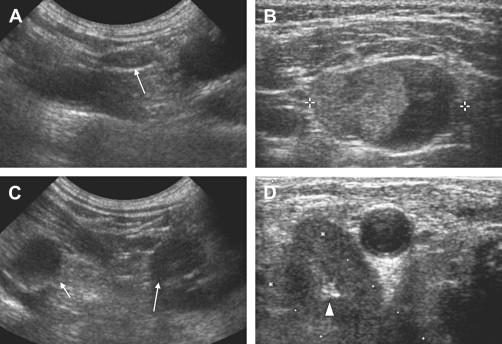
US does not use ionizing radiation and has no known side effects. It is less costly and more available than other imaging modalities. High-frequency transducers yield high-resolution images of the superficial neck structures, allowing detection of clinically nonpalpable disease. Imaging of a certain structure in multiple planes is easy and provides a better appreciation of the morphology. US does not rely on iodine uptake and it can identify recurrent tumor when Tg is falsely negative . Differentiation of normal or reactively enlarged lymph nodes from metastatic ones may be challenging, however. The size of a lymph node is an important indicator of its character; the malignant nodes are larger than benign ones in general, but small nodal metastases from thyroid cancer are frequent enough to render size alone an ineffective criterion in differentiating benign nodes from malignant ones. The shape of a node is a useful feature in nodal characterization. Ovoid (flat) nodes are usually benign, whereas round nodes are usually malignant ( Fig. 1 ). The shape of a node can be described by the ratio of its longitudinal to transverse dimensions. A ratio of less than 2 suggests malignancy. Identification of the hyperechoic nodal hilum is a good sign of a benign node, but about one half of benign nodes do not show this finding. Hyperechoic nodes are usually benign, whereas malignant nodes are usually hypoechoic. The presence of microcalcification or cyst suggests a malignant character. Although the accuracy of these findings may be limited when considered alone, a combination of these features helps predict malignant nodes. Postoperative granulation, parathyroid, and thymic tissue may mimic metastatic nodes. One of the greatest advantages of US is its ability to guide fine needle aspiration biopsy (FNAB), which is more than 95% accurate when performed by experienced radiologists . Using these features, suspicious nodes can be identified and biopsied under US guidance. This strategy, combined with Tg surveillance, yields superior results, compared with other screening methods.
The biggest drawback of US is its limited anatomic coverage. The paravertebral, retrotracheal, and retropharyngeal regions and nodal chains close to the skull base are inadequately imaged with US. The fact that most recurrences occur in the lower nodal chains and thyroid bed, which are easily accessible, however, makes US a very efficient and practical tool.
CT
CT uses ionizing radiation, requires intravenous iodinated contrast administration, which might interfere with other tests, and is more costly than US. However, CT provides a much more comprehensive coverage of the neck compared with US. Traditionally, images are displayed in the transverse plane, which is also the plane in which measurements are made of the lymph nodes. Although newer multidetector units allow easy multiplanar reconstruction of images, no formal study has been done of the benign and pathologic nodes that takes into account the third dimension of the node. However, the size and shape criteria used in US should be directly transferable to CT. Areas of heterogeneous enhancement and central areas of low attenuation within a neck node are reliable signs of metastasis. Retropharyngeal nodal basin is a rare but known site of metastasis from thyroid cancer and can be much more reliably imaged with CT. Metastatic nodes close to the skull base (high level II) are also more reliably identified with CT compared with US. In addition, CT evaluation of extranodal extension of disease with involvement of the paravertebral and prevertebral structures and trachea is superior. CT evaluation of the chest, abdomen, and pelvis for detection and localization of distant metastasis is also feasible. In particular, lung metastases from thyroid cancer are often small and have a miliary pattern, making CT an excellent choice because of its superior spatial resolution, compared with positron emission tomography (PET) and 131 I WBS ( Fig. 2 ). Thus, CT is valuable when recurrence is suspected on the basis of increased Tg and disease cannot be localized with US or 131 I WBS. Also, in cases of established recurrence, CT is indispensable in planning the surgery owing to its superior ability to assess the local and regional extent of disease.




