Fig. 16.1
Patterns of tumor growth. Endophytic growth pattern with tumor arising from retina (arrows) and invading the vitreous (a). Notice the formation of vitreous seeds(*), which are small pieces of tumor floating in the vitreous. Exophytic growth pattern with tumor arising from the retina (arrows) and invading the subretinal space (b). Mixed growth pattern is a combination of endophytic and exophytic where the retina is mostly replaced by tumor (c)
16.1.2 Exophytic Growth Pattern
The exophytic tumor grows towards the choroid into the subretinal space, detaching the retina and forming subretinal tumor seeds, which are prone to choroidal invasion (Fig. 16.1b).
16.1.3 Mixed Growth Pattern
The mixed growth pattern is the most common and displays both endophytic and exophytic patterns (Fig. 16.1c).
16.1.4 Diffuse Infiltrative Pattern
Another growth pattern of clinical importance is the diffuse infiltrative type, which typically presents in older children. Diffuse tumors infiltrate the retina without forming an obvious retinal mass, and often invade the anterior segment forming a pseudohypopyon of tumor cells. This pattern has prognostic importance because it can be mistaken clinically for an inflammatory process [2].
16.1.5 Necrotic Retinoblastoma
Finally, an extensively necrotic retinoblastoma can present clinically as an inflammatory process that mimics orbital cellulitis with chemosis and proptosis [1, 5, 6]. Histopathologically, such cases show total tumor necrosis associated with intraocular tissue necrosis. This type carries an increased incidence of poor prognostic factors for metastasis (see below).
16.2 Histopathologic Features
The characteristic histopathologic findings in retinoblastoma include a tumor that replaces the retina with medium-sized cells that have a high nuclear/cytoplasmic ratio, marked apoptotic and mitotic activity, and foci of necrosis with calcification (Fig. 16.2a, b). The areas of necrosis typically surround vessels that are cuffed by a layer of viable cells measuring 90–100 μm in radius (Fig. 16.2c). The active turnover of the tumor often releases DNA from the cells, which forms basophilic deposits around vessels and on basement membranes. Most of the tumor grows as sheets or large foci of undifferentiated cells (Fig. 16.3a) [1–4]; however, sometimes there are areas of tumor differentiation evident as rosettes and fleurettes. The most differentiated tumors exhibit actual photoreceptor differentiation that is evident as bouquet-like aggregates of cells called fleurettes, which lack mitoses or necrosis (Fig. 16.3b). A tumor composed solely of fleurettes is designated a retinocytoma or retinoma – the benign counterpart of retinoblastoma (Chap. 7) [1–3]. Rosettes represent varying degrees of retinal differentiation. Flexner–Wintersteiner rosettes comprise a ring of nuclei surrounding an empty lumen analogous to the subretinal space. The cells are joined by intercellular attachments similar to those found between photoreceptors (Fig. 16.3c). Primitive Homer Wright rosettes are formed by a rim of nuclei with a center filled by tangles of cytoplasmic filaments (Fig. 16.3d). These rosettes also occur in neuroblastomas and other tumors. Both types may contain mitotic figures.
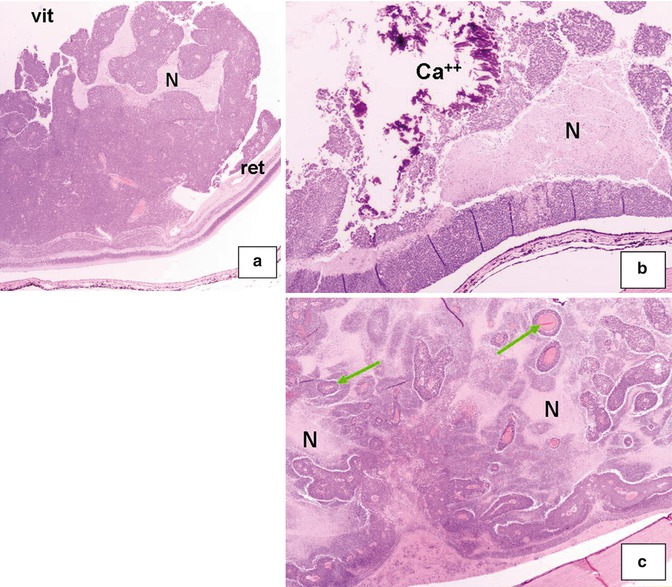
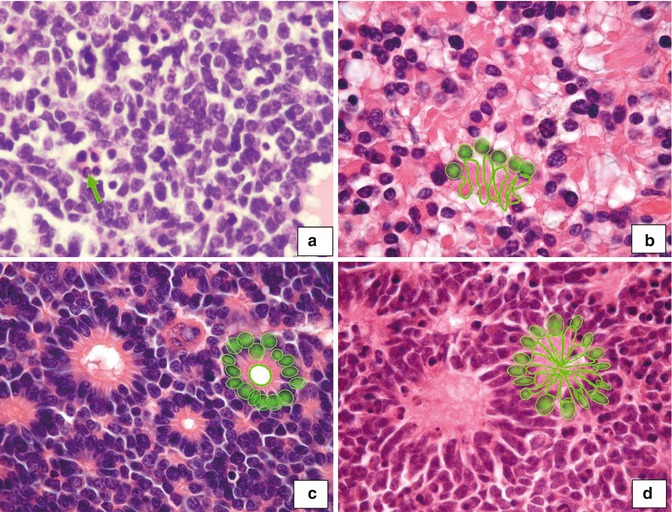
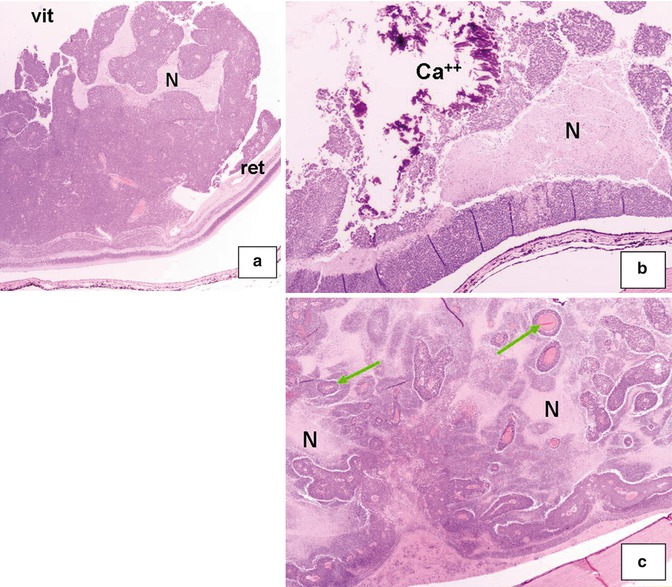
Fig. 16.2
Retinoblastoma is composed of small blue cells and arises from the retina (ret); the tumor cells alternate with geographic areas of necrosis (N) and invade the vitreous (vit) (a) (original magnification ×2). Higher magnification shows necrosis (N) and calcifications (Ca++) (b) (original magnification ×4). Viable tumor cells form cuffs surrounding the vessels (arrows), and they are surrounded by necrosis (N) (c) (original magnification × 4)
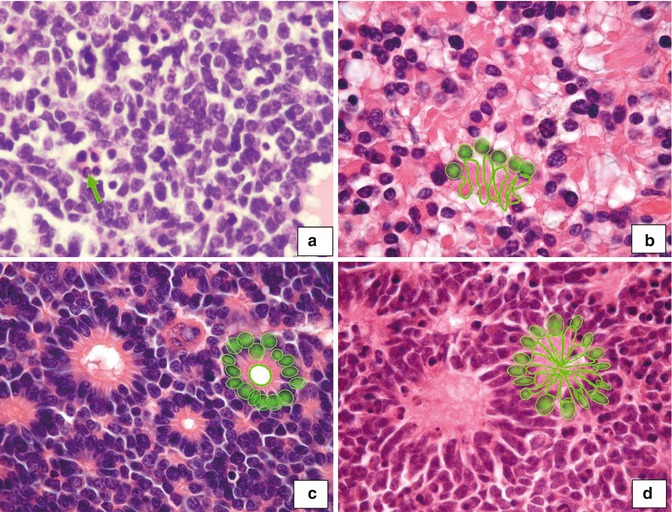
Fig. 16.3
Undifferentiated tumors show sheets of small- and medium-sized cells with scanty cytoplasm and hyperchromatic nuclei (a). Apoptosis is frequently seen (arrow). Fleurettes are composed of cells that closely resemble photoreceptors and are so named because they group in a fashion similar to an arrangement of flowers (b). Flexner–Wintersteiner rosettes are tumor cells forming a round structure with a clear center rimmed by a membrane like the outer limiting membrane in the retina (c). Homer Wright rosettes have a lumen filled by cytoplasmic prolongations of the tumor cells (d) (original magnification ×40)
16.3 Routes of Spread Outside the Eye
If left untreated, retinoblastoma usually fills the eye and completely destroys the internal architecture of the globe. The tumor tends to spread locally by invading the optic nerve and choroid, then hematogenously, and by lymphatics once it reaches the extraocular structures such as the conjunctiva and eyelids.
16.3.1 Optic Nerve Invasion
The most common route of spread is by invasion through the optic nerve (Fig. 16.4). Once in the nerve, tumor spreads directly along it towards the optic chiasm or infiltrates through the pia into the subarachnoid space. After reaching the subarachnoid space, retinoblastoma cells may disperse in the cerebrospinal fluid (CSF) and then invade the brain and the spine. Retinoblastoma cells in the subarachnoid space may reach the optic nerve of the opposite eye through the chiasm, and this can occur without the detectable presence of tumor cells at the surgical margin of the optic nerve [2, 3, 7–11].
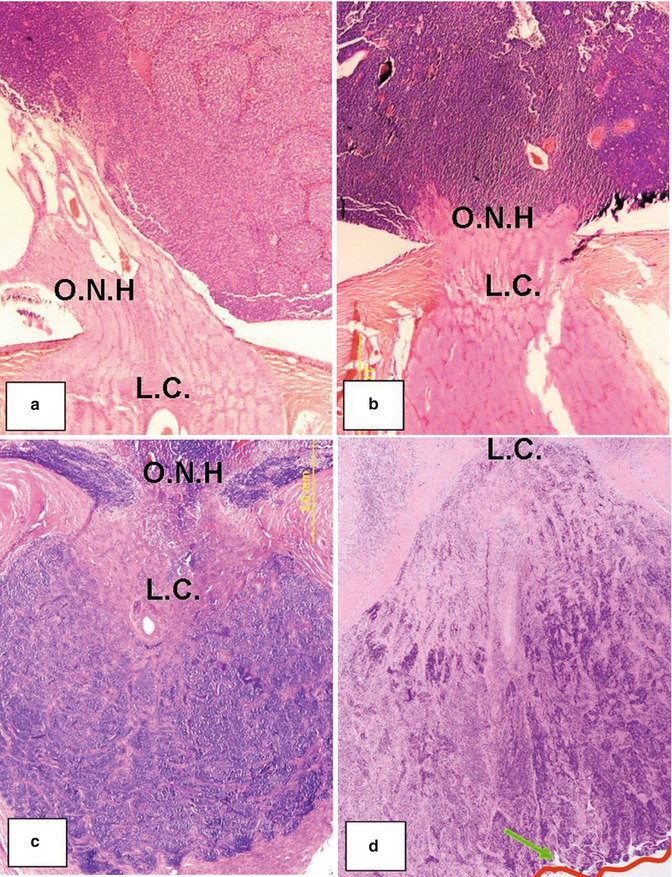
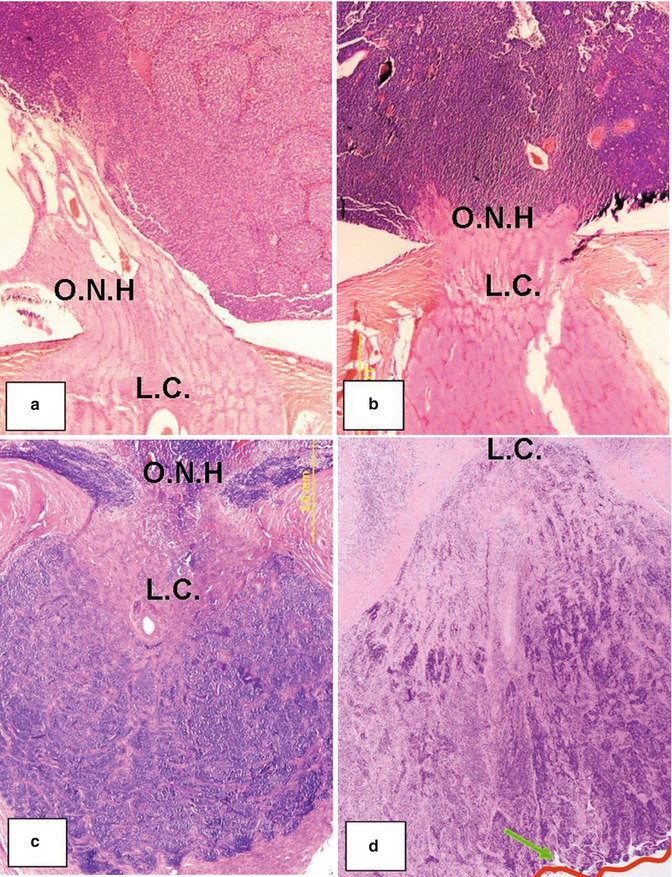
Fig. 16.4
Retinoblastoma invasion at different levels of the optic nerve. Note that the tumor is filling the vitreous cavity and replacing the retina adjacent to the optic nerve head (ONH), but the entire optic nerve is free of tumor (a). Tumor has infiltrated the optic nerve head but does not reach the lamina cribrosa (LC) (b). Tumor has invaded through the lamina cribrosa into the posterior (orbital portion) of the optic nerve but without reaching the margin of resection (c). Tumor massively invades the optic nerve up to the level of the surgical margin (line and arrow) (d) (original magnification ×4)
16.3.2 Choroidal Invasion
The second major route of spread involves massive involvement of the choroid (Fig. 16.5), followed by extension into the orbit via either scleral emissarial canals (channels within the sclera where ciliary vessels, nerves, and vortex veins enter or exit the eye) or by direct invasion through the sclera [1, 2, 9, 11–15]. Extraocular extension generally occurs if intraocular tumors are left untreated (Fig. 16.6a). Extraocular extension dramatically increases the chances of hematogenous and lymphatic spread [2, 3].
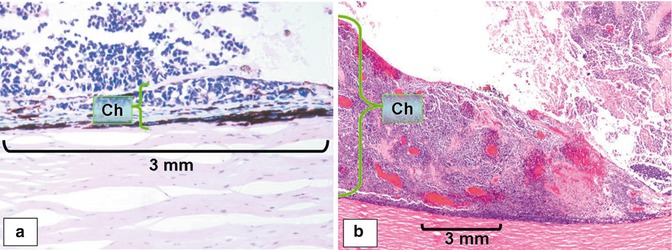
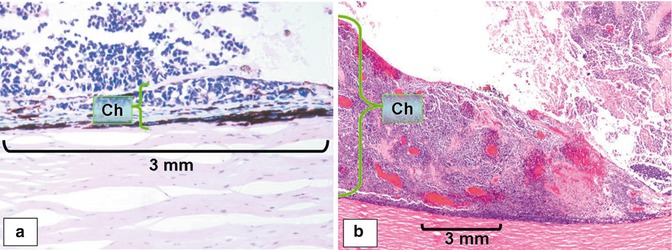
Fig. 16.5
Retinoblastoma invasion of choroid (Ch). Focal invasion of the choroid by tumor that does not expand more than approximately 3 mm in maximum diameter and which is not seen grossly (a) (original magnification × 10). Massive choroidal invasion is seen grossly and expands beyond 3 mm in maximum diameter. Compare the thickness of choroid between focal and massive invasion (b) (original magnification × 4)
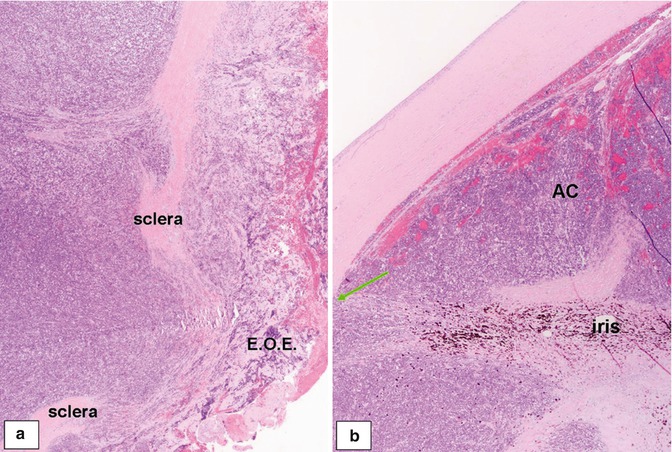
Fig. 16.6
Extraocular extension of retinoblastoma and anterior segment invasion. Extraocular extension (EOE) of tumor through the sclera into the orbital tissue (a) (original magnification ×4). Massive involvement of the anterior chamber (AC) by tumor with effacement of the iris and invasion of the trabeculum and chamber angle structures (arrow) (b) (original magnification ×4)
16.3.3 Hematogenous Dissemination
Metastatic spread can occur by direct infiltration, either through the optic nerve into the brain or through the choroid into the orbital soft tissues and bones. Hematogenous dissemination may induce metastasis even when other types of invasion have not been found. Widespread metastasis presents most frequently in the lung, bone, and brain (Chap. 18) [1, 2, 16].
16.3.4 Lymphatic Dissemination
Metastasis via lymphatic dissemination can occur when tumors spread anteriorly into the conjunctiva and eyelids or extend into extraocular tissues. Lymphatic vessels and lymphoid tissue are absent in the orbit and intraocular tissues. In the ocular region, only the conjunctiva and skin have lymphatic channels. Tumors must first reach these areas to permeate the lymphatic vessels and then spread into regional lymph nodes [1, 2, 16].
Histologically, retinoblastoma metastases appear less differentiated than intraocular tumors. Rosettes are rarely encountered, and fleurettes have never been described. When a focus of a very well-differentiated tumor is found outside the orbit, the differential diagnosis must include primary primitive neuroectodermal tumor (PNET) [1, 2].
16.4 Histopathologic Factors That May Be Useful in Determining Prognosis
Metastatic disease is still associated with a poor prognosis [11–19]. Most clinical findings are not useful in predicting the occurrence of metastasis in children with retinoblastoma, although histopathologic data provide a fair estimate of its risk. Multivariate statistical analysis has suggested the correlation of certain histopathologic findings with metastastic disease (Table 16.1) [17, 19, 20]. The most important prognostic indicators for the development of metastasis are the presence of tumor in the optic nerve posterior to the lamina cribrosa, tumor at the site of surgical transection, and extrascleral extension of tumor into the orbit (Fig. 16.4) [7–12, 20]. Other factors associated with probable risk for metastatic behavior, especially in conjunction with the major factors cited above, are massive choroidal invasion, tumor invasion into the anterior chamber (Fig. 16.6b), large tumor size with vitreous seeding, neovascularization of the iris, and glaucoma (Table 16.2) [12–21].
Table 16.1
Conventional histopathologic poor prognostic factors for metastasis in retinoblastoma
Risk factor | Extent |
|---|---|
Orbital invasion | Present |
Optic nerve invasion | Retrolaminar invasion |
At line of transection | |
Scleral and extrascleral invasion | Present |
Choroidal invasion | Massive |
Anterior segment involvement | Present |
Table 16.2
Probable histopathologic poor prognostic factors for metastasis in retinoblastoma
Risk factor | Extent |
|---|---|
Extensive necrosis of tumor and intraocular tissues | Present |
Tumor angiogenesis | Relative vascular area >3.9 % |
Large tumor with vitreous seeds | Present |
Iris neovascularization | Present |
Glaucoma | Present |
16.4.1 Tumor Invasion into the Optic Nerve
The extent of tumor invasion in the optic nerve correlates with prognosis. In several published series [7–12, 20], superficial invasion of the optic disc was associated with a mortality rate (10 %) similar to that seen when the optic nerve is not involved. The presence of tumor up to the lamina cribrosa is associated with a mortality rate of 29 % (Fig. 16.4a–d). This rises to 42 % when tumor is found posterior to the lamina cribrosa, and the presence of tumor at the transected surgical margin is associated with a mortality of 80 % [7–12, 20, 21]. The importance of obtaining a long segment of optic nerve at the time of enucleation is emphasized by these results.
Specific studies related to the length of the optic nerve stump alone suggest that patients with an optic nerve stump measuring <5 mm in the enucleated eye have a worse prognosis than those having >5 mm stumps. However, other series found no correlation between the length of the optic nerve stump and metastatic events [13].
The location of retinoblastoma in the different portions of the optic nerve has been shown to be important: the closer to the brain the tumor margin, the worse the prognosis for metastasis [7–13]. However, the amount of tumor present and the coexistence of choroidal involvement also appear to have a prognostic value. More precise measurement of the invading tumor into the nerve, together with the location, may be needed. Limitations for exact measurement include the plane of section and the number of sections examined. However, results may become comparable if pathologists adopt a standardized protocol for ocular dissection and tissue submission, sectioning, and examination.
Even though the results may not be exact measurements of the actual amount of tumor present, they may be representative of the biological process in each case.
16.4.2 Tumor Invasion into the Choroid
Conventionally, tumor invasion of the choroid has been described as massive or focal without commonly agreed definitions of the degree of invasion that constitutes each descriptor. Using this imprecise terminology, however, massive – but not focal – invasion of the choroid by tumor increases the possibility for hematogenous spread, either via the choroidal vessels or, more frequently, by extension through the sclera into the orbital tissues (Fig. 16.6a) [6–12].
The prospective clinical trial of the Children’s Oncology Group used an objective definition for massive involvement. Massive invasion is defined as 3 mm or more of invasion in the choroid. The International Retinoblastoma Staging Working Group proposed the 3 mm or more and the tumor reaching the sclera to consider a focus of invasion as massive invasion [22]. Focal invasion is any tumor invasion in the choroid that is less than 3 mm. If there are multiple foci the measurements should be added to have the maximum amount of invasion. The significance of choroidal involvement and its effect on survival outcome remains controversial. In the literature, some degree of choroidal invasion has been reported in 12–62 % of eyes enucleated for retinoblastoma [12, 19, 23–25].
Some studies found that choroidal invasion is an isolated risk factor for disease, with widely ranging mortality rates from 11 to 81 % [12, 19, 25].
16.4.3 Scleral and Extrascleral Extension
The reported occurrence of scleral infiltration (1–8 %) [12, 17, 19], and extrascleral extension (2–13 %) [12, 17, 19], varies widely, even in series reported from developed countries. It is now generally agreed that infiltration and extrascleral extension are the risk factors that are predictive of metastasis [12, 17, 19, 26].
16.4.4 Tumor at Surgical Margins and in the Orbit
The optic nerve is the most important surgical margin for prognosis in eyes with retinoblastoma because of the predilection of this tumor to spread primarily through the optic nerve. If the tumor is present at the cut end of the optic nerve, retinoblastoma tumor cells are left in the orbit (Fig. 16.4a–d). Once the orbital soft tissues are invaded, the tumor spreads directly into the orbital bones, through the sinuses into the nasopharynx, or via the various openings into the cranium. In cases of extraocular extension of tumor before enucleation, the soft tissues of the orbit represent additional surgical margins [1, 2]. Currently, most ophthalmic oncologists would administer pre-enucleation chemotherapy if extraocular extension is suspected, in order to decrease the tumor burden and to target the extraocular extension. In these cases, evaluation of orbital soft tissue margins to access the presence of residual tumor is of prognostic importance (Chap. 17).
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


