12 The presence of hemorrhage in the posterior segment may cause significant visual disturbance and may signify a serious ocular or systemic abnormality. For this reason, accurate diagnosis and appropriate care for the patient with hemorrhage of the posterior segment require a thorough medical history, review of systems, and careful and complete examination of both eyes. The clinical entities discussed in this chapter are common and important conditions most likely to be encountered in daily practice. The guidelines provided are intended as a framework for clinical evaluation and therapeutic considerations to be thought out carefully in the context of the individual patient. Blood in the vitreous cavity may be as mild as a suspension of pigmented cells or as severe as to cause complete obscuration of any fundus detail. The source of the blood can be (1) subretinal vessels (e.g., from choroidal neovascularization in age-related macular degeneration or from a choroidal tumor); (2) an avulsed, native retinal blood vessel (e.g., caused by a retinal break or direct trauma); or (3) fragile, proliferative preretinal new vessels. Vitreous hemorrhage most often stems from bleeding from an area of preretinal or intraretinal neovascularization (Table 12–1). This neovascularization is most commonly seen as a sequela of diabetic retinopathy or retinal occlusive disease (see later discussion) but may occur as part of the body’s compensatory response to any condition that produces retinal ischemia. Careful funduscopy often reveals the source of the bleeding, but in cases of dense vitreous hemorrhage, B-scan ultrasonography is valuable for visualizing the posterior segment. Ultrasound examination may disclose a retinal break, retinal detachment, or retinal or choroidal mass, or an elevated area of neovascularization. Treatment and timing of treatment are determined by the underlying condition causing the vitreous hemorrhage as well as by the patient’s level of functioning and systemic health. Terson syndrome is the term used to describe the specific association of intracranial and vitreous hemorrhages1 and has been found to occur in 3 to 8% of patients with subarachnoid hemorrhage.2–4 Some type of intraocular hemorrhage (subretinal, intraretinal, preretinal, or vitreous) may be seen in up to 20% of patients with subarachnoid or subdural hemorrhage.2,5 The exact pathogenesis of Terson syndrome is still unknown. It is thought that intracranial hemorrhage leads to increased intracranial pressure, which is transmitted along the subdural space of the optic nerve. This acute rise in intraocular pressure in turn causes compression of the central retinal vein and blockage of retinal venous outflow, which leads to rupture of retinal capillaries.6 Typically, multiple blot-shaped retinal hemorrhages are seen in the peripapillary and macular regions. Larger areas of hemorrhage beneath the internal limiting membrane or posterior hyaloid face, sometimes assuming an elevated or dome-shaped appearance, also may occur. Vitreous hemorrhage may be dense enough to obscure visualization of the posterior pole. The presence of intraocular hemorrhages may have prognostic as well as diagnostic value. In one retrospective study of 320 patients with subarachnoid hemorrhage, those with associated intraocular hemorrhage had a significantly higher mortality rate (53.6%) than those without intraocular hemorrhage (19.7%).5 Although mortality rates have diminished substantially in the 25 years since publication of that study, it remains likely that intraocular hemorrhage correlates with the severity of injury. In a recent prospective series of 100 patients with subarachnoid hemorrhage, patients with intraocular hemorrhage were much more likely to have experienced coma than those without ocular involvement (89% versus 46%).2
Hemorrhage
Vitreous Hemorrhage
What Are the Sources of Vitreous Hemorrhage?
Terson Syndrome
| Systemic diseases |
| Diabetic mellitus |
| Hemoglobinopathies |
| Sarcoidosis |
| Ocular ischemic syndrome |
| Hyperviscosity syndromes |
| Incontinentia pigmenti |
| Systemic lupus erythematosus |
| Antiphospholipid antibody syndrome |
| Retinal vascular diseases |
| Venous occlusion |
| Arterial occlusion |
| Radiation retinopathy |
| HIV retinopathy |
| Retinopathy of prematurity |
| Intraocular inflammation |
| Uveitis |
| Pars planitis |
| Eales disease |
| Behçet disease |
| Bird-shot chorioretinopathy |
| Acute retinal necrosis |
| Toxoplasmosis |
| Neoplasms |
| Choroidal melanoma |
| Choroidal hemangioma |
| Inherited retinal conditions |
| Familial exudative vitreoretinopathy |
| Retinitis pigmentosa |
| X-linked juvenile retinoschisis |
HIV, human immunodeficiency virus.
HOW IS TERSON SYNDROME MANAGED?
In most cases, these hemorrhages clear spontaneously, albeit slowly. Vitreous hemorrhage usually clears within 1 year but may remain for as long as 6 years.7,8 Schultz and colleagues reported final visual acuity of 20/50 or better in 12 of 16 patients managed with observation alone.8 The main complication following spontaneous clearing is epiretinal membrane formation, but cataract, macular pigmentary changes, retinal detachment, and proliferative vitreoretinopathy also have been reported.9–11
Vitrectomy has been successful in removing vitreous hemorrhage and accelerating visual recovery in patients with Terson syndrome, even in patients with initially dense hemorrhages.2,12 Kuhn and colleagues reported on their results of vitrectomy performed as early as 1 month, and as late as 30 months following diagnosis of Terson syndrome. Vision was 20/30 or better in 21 of 26 eyes (81%) of adult patients. None of the seven eyes of five children, however, achieved vision of better than 20/60.2 Whereas this worse result in children (four of whom were under 1 year of age) may have been a result of associated brain injury, earlier intervention should be considered in children for the prevention of deprivational amblyopia.
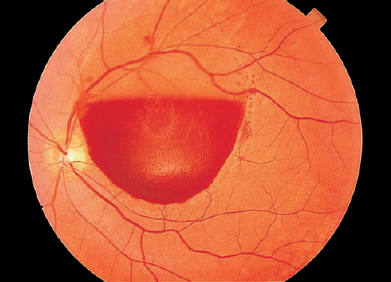
FIGURE 12–1. Valsalva retinopathy. A boat-shaped retinal hemorrhage is present, presumably located under the internal limiting membrane of the retina. (Courtesy of William Tasman, M.D.)
Valsalva Retinopathy
Activities such as lifting, straining, coughing, vomiting, childbirth, or similar exertion cause a sudden rise in intraabdominal or intrathoracic pressure (Valsalva maneuver). The concomitant acute elevation in ocular venous pressure may precipitate rupture of superficial retinal capillaries (termed Valsalva retinopathy).
The typical ophthalmoscopic finding is of one or more well-circumscribed, round or dumbbell-shaped hemorrhages beneath the posterior hyaloid or internal limiting membrane (ILM) within the macula of one eye (Fig. 12–1). Overlying striae, representing wrinkling of the ILM, also may be seen. Sudden and dramatic loss of vision is often caused by hemorrhagic detachment of the ILM, vitreous hemorrhage, or hemorrhage in the fovea.1,13
HOW IS VALSALVA RETINOPATHY MANAGED?
The hemorrhages of Valsalva retinopathy typically resolve spontaneously over several weeks, with accompanying return of vision. In rare cases in which vision or physical function is impaired as a result of macular subhyaloid hemorrhage, blood may be drained into the vitreous by neodymium:yttrium-aluminum-garnet (Nd:YAG) laser disruption of the posterior hyaloid face.14 The chance of complications of the procedure, particularly macular hole and retinal detachment, must be considered seriously, however, if such a procedure is contemplated.14
Retinal Hemorrhage
What are the features that aid in the diagnosis of retinal hemorrhage? In the evaluation of retinal hemorrhage, various clinical features will aid in the formulation of a differential diagnosis (Fig. 12–2):
- Topographical location (macular, posterior pole, anterior)
- Intraretinal location (superficial, deep, or mixed) (Fig. 12–3)
- Spatial distribution (sectorial or diffuse, unilateral or bilateral)
- Number (few or multiple)
- Shape and appearance (flame-shaped, dot/blot, white-centered, circumscribed, or irregular)
- Appearance of vasculature (venous tortuosity or dilatation, arteriolar attenuation, sheathing, aneurysmal changes)
- Associated ocular signs (anterior chamber reaction, vitreitis, papillitis, nerve fiber layer infarcts)
Diabetic Retinopathy
Diabetic retinopathy remains one of the leading causes of blindness in the United States. Large-scale epidemiologic studies have elucidated the natural history, prevalence, and progression of retinopathy and other ocular complications of diabetes, and randomized clinical trials have outlined recommendations for therapy (Fig. 12–4). Regular examination and timely treatment remain essential to preservation of vision for patients with diabetes.
What Are the Important Points Regarding the Epidemiology and Pathogenesis of Diabetic Retinopathy?
Microangiopathy is the fundamental abnormality in diabetic retinopathy. Disturbances in capillary function lead to retinal nonperfusion, which in turn leads to retinal ischemia. Elaboration of vasoproliferative factors (among them vascular endothelial growth factor, or VEGF)15 induces proliferation of new blood vessels on the retina and optic nerve (proliferative diabetic retinopathy, or PDR), with subsequent contraction of these fibrovascular proliferations.16
The risk of developing retinopathy is directly related to the duration of disease and the extent of hyperglycemia.17,18 In patients with the onset of type 1 insulin-dependent diabetes mellitus before the age of 30 years, few will show any change within 5 years of diagnosis. After 20 years, however, nearly all will have some retinopathy, and roughly half will have proliferative disease.19 Among patients who are older than 30 at diagnosis, 67% will have some retinopathy after 10 years, and 10% will have proliferative change.20 The risk of retinopathy in these patients is correlated with the requirement for insulin.
What Are the Clinical Features of Diabetic Retinopathy?
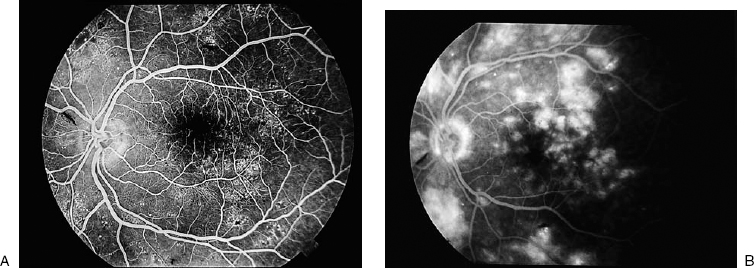
The initial ophthalmoscopic findings (nonproliferative, or background, retinopathy) are microaneurysms, which appear as minute red dots in the inner and middle retinal layers. Accompanying dot and blot hemorrhages (located in the outer plexiform and inner nuclear layers of the retina) may be indistinguishable from microaneurysms. Patent microaneurysms may be identified by fluorescein angiography because they leak fluorescein dye (Fig. 12–5). An increase in the number of microaneurysms may be an early sign of progression of diabetic retinopathy.21 Klein and colleagues reported that patients with an increased ratio of microaneurysms at 4-year follow-up compared with baseline (greater than 3:1) were at three times greater risk for development of PDR by 10-year follow-up than patients with smaller change.22
The vascular permeability that accompanies microaneurysmal change allows leakage of fluid into the intercellular spaces of the retina. Clinically, this leakage appears as thickening of the retina and is appreciated biomicroscopically as decreased translucency of the retina and blurring of the normal background choroidal pattern. Lipid exudation may accumulate in the areas of leakage, often forming a ring around the leaking microaneurysms.23 When such intraretinal edema occurs in the macula, vision is often affected. Macular edema is an important manifestation of nonproliferative diabetic retinopathy (NPDR) and is the leading cause of legal blindness among diabetic patients.
With worsening diabetes, the inner retina becomes more ischemic, with increases in hemorrhages, nerve fiber layer infarcts, and areas of capillary nonperfusion. Venous beading (focal dilatations likely representing areas of poor circulation) develops, along with intraretinal microvascular abnormalities (IRMAs, which are flat, dilated capillary channels that may serve as collateral circulation). IRMAs often resemble surface retinal neovascularization; angiographically, however, IRMAs retain fluorescein dye, whereas neovascularization leaks dye profusely. Advanced NPDR was defined by investigators in the Early Treatment Diabetic Retinopathy Study (ETDRS) as intraretinal hemorrhages in four quadrants, venous beading in two or more quadrants, or IRMA in one or more quadrants (the so-called 4:2:1 rule). The presence of one or more of these clinical signs was highly predictive of progression to PDR within 1 year.24
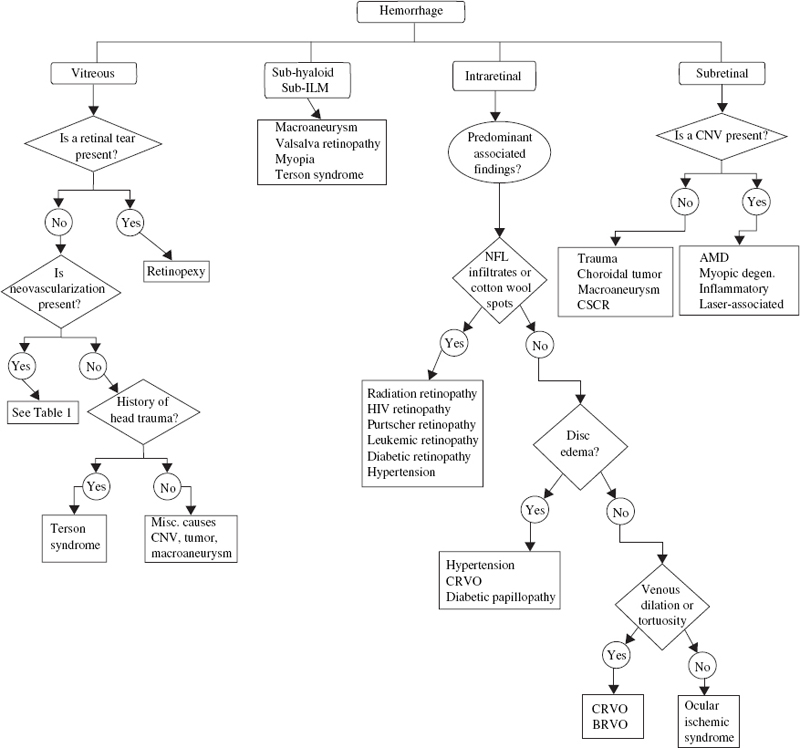
FIGURE 12–2. Diagnostic evaluation of hemorrhage of the posterior segment. ILM, internal limiting membrane; CNV, choroidal neovascularization; AMD, age-related macular degeneration; CSCR, central serous chorioretinopathy; CRVO/BRVO, central/branch retinal vein occlusion; NFL, nerve fiber layer.
According to the ETDRS, nearly 50% of patients with very advanced NPDR (with two or more signs of the 4:2:1 rule present) developed PDR after one year.24 Proliferative blood vessels tend to arise in the posterior pole in areas of severe retinal ischemia. When they arise at or within one disc diameter (1 DD) of the optic nerve, they are referred to as neovascularization of the disc (NVD). When they arise more than 1DD away from the disc, they are termed neovascularization elsewhere (NVE).24 These vessels grow more easily along a “scaffold” of connective tissue, such as the posterior hyaloid face, and may be pulled into the vitreous cavity. The new vessels gradually become surrounded with fibrovascular tissue. Vitreous contraction, coupled with intrinsic contraction from fibrovascular proliferation, transmits tension along the fragile new blood vessels, resulting in vitreous hemorrhage.16 Tension along the retina may result in tractional retinal detachment.
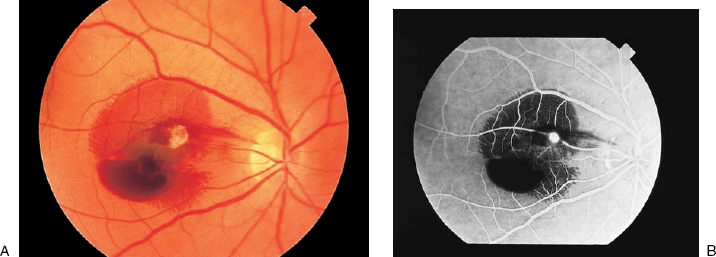
FIGURE 12–3. (A). Retinal arterial macroaneurysm with subretinal hemorrhage in the superior macular and a boat-shaped subhyaloid hemorrhage in the inferior macula. (B). Fluorescein angiogram at 23 seconds after injection. The macroaneurysm appears as a hyperfluorescent focus along a retinal artery. Retinal vessels are visible overlying the subretinal blood but are obscured inferiorly by the subhyaloid blood.
Vitreous hemorrhage often occurs during sleep, possibly as a result of rapid eye movement, and is seldom induced by exercise.25 If erythrocytes enter the vitreous cavity and become invested within the gel, they may take months to years to clear spontaneously. Superficial hemorrhages beneath the ILM may be seen as round, oval, or “boat-shaped” patches of bright red blood that obscure vessel detail. Tight sub-ILM hemorrhages may progress rapidly to tractional retinal detachment.
What Are the Relevant Issues Regarding Medical Management of Diabetic Retinopathy?
The most effective method for preventing diabetic retinopathy remains regular funduscopic examination and tight control of blood glucose. In a study of 1441 patients with type 1 diabetes mellitus in the Diabetes Control and Complication Trial (DCCT), those treated with “intensive” glycemic control (frequent monitoring to achieve a mean hemoglobin A1C of 7.2) suffered significantly less progression in retinopathy and nephropathy than those treated “conventionally” (hemoglobin A1C of 9.1).26,27 These effects have remained after 10 years of follow-up.28 Patients with good glycemic control and shorter duration of disease at baseline had the best prognosis. Whereas up to 13% of patients showed initial worsening of their retinopathy after 12 months of intensive therapy, recovery was achieved soon thereafter and the ultimate reduction in long-term risk remained significant.29
Reduction in blood pressure with the angiotensin-converting enzyme inhibitor lisinopril, even in normotensive patients with type 1 diabetes, slows progression of retinopathy.30 Captopril and atenolol (a beta-receptor antagonist) appear to work equally well.31 According to the ETDRS, treatment with aspirin did not affect the progression of retinopathy, visual loss, or risk of vitreous hemorrhage, but it did reduce morbidity and death from cardiovascular disease by 17%.32,33 Because diabetic patients with high levels of cholesterol and lipids have higher risks of both PDR and macular edema from retinal exudation,23 treatment of hyperlipidemia may be advisable. Clinical trials of drugs targeting angiogenic factors (i.e., VEGF, growth hormone) are also under way.34,35
When and in What Way Is Intervention with Laser Photocoagulation Appropriate for Diabetic Retinopathy?
Following its introduction in the late 1950s, laser energy was used to coagulate areas of blood vessels on the surface of the retina36 and was found to have a beneficial effect on retinal neovascularization and macular edema. Data from the Diabetic Retinopathy Study (DRS), a multicenter trial of 1742 patients, identified characteristics associated with a particularly high risk of visual loss (defined as 5/200). These so-called high-risk characteristics are NVD greater than one third disc area, any NVD with vitreous hemorrhage, and one half disc area of NVE associated with vitreous or preretinal hemorrhage.37 The goal of panretinal photocoagulation (PRP) is to arrest retinal neovascularization and prevent visual loss. Treatment with xenon-arc or argon-laser PRP reduced the risk of severe visual loss by 50%.37 The current standard of PRP uses 1200 to 2000 spots of argon green or blue green laser burns, 500 μm in width, of intensity sufficient to lightly whiten the overlying retina.
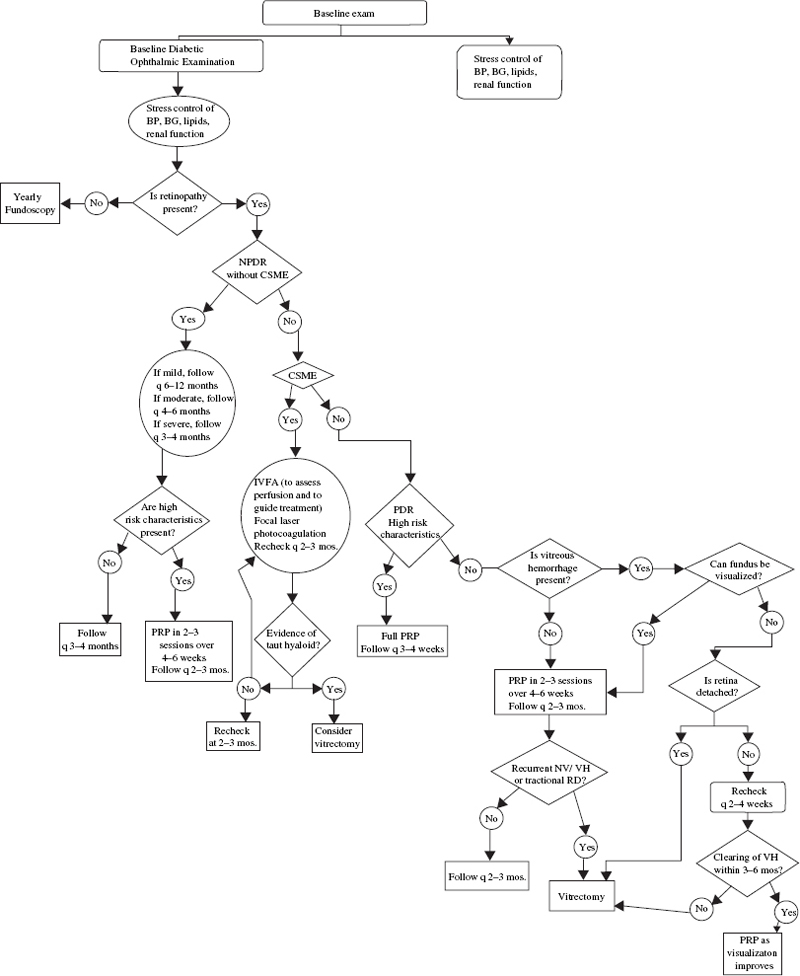
The ETDRS established that focal macular laser photocoagulation is effective in slowing progression of visual decline in patients with clinically significant macular edema (CSME). CSME was defined as retinal thickening involving the macula, hard exudates within 500 μm of the fovea if associated with retinal thickening, or an area of macular edema greater than one disc area but within 1 DD of the fovea. The goal of treatment is to treat all leaking microaneurysms 500 μm or greater from the center of the macula.38,39 Alternatively, grid treatment to areas of diffuse capillary nonperfusion may be applied. Patients with macular edema with the best visual prognosis following focal treatment have circinate retinopathy of recent duration and good macular perfusion. Poorer prognosis is associated with foveal lipid exudation, diffuse edema, widespread nonperfusion, and systemic hypertension.40
Under What Conditions Should Vitrectomy Be Considered for Diabetic Retinopathy?
The main indications for surgical treatment of diabetic retinopathy include vitreous hemorrhage, retinal detachment, and intractable macular edema resulting from a taut posterior hyaloid face.41,42 In the Diabetic Retinopathy Vitrectomy Study (DRVS), the efficacy of immediate vitrectomy, deferred vitrectomy, and observation in diabetic patients were analyzed in a randomized, prospective fashion.41,43–45 On the basis of the DRVS reports, the following recommendations may be made:
- The decision for vitrectomy must be weighed seriously, as 25% of patients who underwent immediate vitrectomy had a final visual acuity of no light perception.
- Patients with moderate to advanced PDR and useful vision (defined as 10/200 or better) are more likely to benefit from early vitrectomy. This advantage was most clear-cut for patients with type I diabetes.
- Patients with PDR and vitreous hemorrhage reducing vision to 5/200 or worse are more likely to regain vision (20/40 or better) with immediate vitrectomy (25% versus 15%). This advantage was again more pronounced for Type I diabetics (36% versus 12%).
In a recent study of patients with persistent macular edema unresponsive to laser photocoagulation, vitrectomy with stripping of the premacular posterior hyaloid face improved vision by at least two lines in half of the patients.42 Vitrectomy remains a valuable therapeutic modality for preservation of vision in patients with end-stage diabetic retinopathy. Furthermore, clinical utility analysis has shown early vitrectomy in appropriate situations both to improve quality of life and to be highly cost-effective.46
Retinal Occlusive Disease
Occlusions of the retinal venous and arterial circulations are a significant cause of visual morbidity and may be associated with serious or even life-threatening systemic conditions (Fig. 12–6). Because such patients often present with abrupt visual changes, recognition of retinal occlusive disorders by the ophthalmologist and referral for appropriate medical evaluation are essential.
Central Retinal Vein Occlusion
The typical appearance of central retinal vein occlusion (CRVO) includes intraretinal hemorrhages in all four quadrants, optic disc edema, and dilation and tortuosity of the retinal venous system. Hemorrhages are clustered in the posterior pole and often are accompanied by nerve-fiber layer infarctions (“cotton-wool spots”) and macular edema.47,48 The occlusion is thought to arise from thrombus formation at the lamina cribrosa.49
What Are the Important Clinical and Epidemiologic Aspects of Central Retinal Vein Occlusion?
Central retinal vein occlusion can affect patients from 9 months to 92 years of age, but it occurs most often in patients 60 years or older; fewer than one sixth are under 45 years of age. Men are affected more commonly than women.50–52
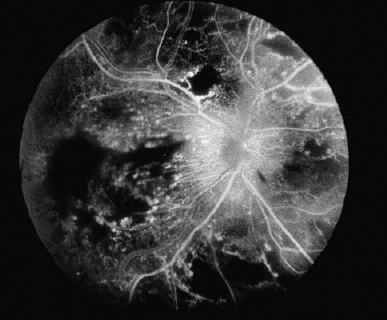
On the basis of clinical and fluorescein angiographic features, two forms of CRVO have been identified.47 This distinction is important because of the significant difference in visual prognosis, management, and patient counseling. The more severe, “ischemic” form (also termed complete, nonperfused, or hemorrhagic retinopathy) is characterized by poorer vision at presentation, copious intraretinal hemorrhages and nerve-fiber layer infarcts, electroretinographic abnormalities, and extensive capillary nonperfusion (more than 10 disc areas of capillary nonperfusion by fluorescein angiography) (Fig. 12–7). The milder, “nonischemic” form (also termed incomplete, perfused, or venous stasis retinopathy) generally presents with better vision and less widespread ischemia (Fig. 12–8). Patients with nonischemic CRVO have better visual prognosis and are less likely to develop intraocular neovascularization and neovascular glaucoma, a dreaded complication of retinal occlusive disease.50,53,54
Several case–control studies have identified a profile of risk factors, especially in older patients, similar to that seen in cardiovascular disease. CRVO is associated with systemic arterial hypertension, electrocardiographic abnormalities, diabetes mellitus, peptic ulcer disease, and thyroid disease.51,55,56 Because there is often a history of glaucoma or ocular hypertension, both eyes should be examined carefully.51,57
What Is the Prognosis, and What Are the Management Options for Central Retinal Vein Occlusion?
Neovascular glaucoma has been recognized as a complication of CRVO for nearly a century. Numerous researchers have concluded that the risk of neovascularization is directly related to the extent of retinal ischemia.53,54,58 Neovascularization is thought to be induced by increased levels of angiogenic factors (among them, VEGF) in the vitreous cavity and anterior chamber of eyes that have suffered ischemic injury.15
The Central Vein Occlusion Study (CVOS) was a prospective, multicenter clinical trial with several aims: (1) to describe the natural history of CRVO and to identify risk factors for development of intraocular neovascularization and vision loss; (2) to evaluate the efficacy and timing of PRP for the prevention of anterior segment neovascularization in cases of ischemic CRVO; and (3) to evaluate the efficacy of macular grid photocoagulation for visual improvement in patients with chronic macular edema.
In the CVOS, initial vision was a strong predictor of final vision as well as risk of neovascularization. Sixty-five percent of patients with initial vision of 20/40 or better maintained vision in that range, whereas patients with presenting vision of 20/200 or worse had only a 20% chance of visual improvement. Neovascularization of the iris (NVI) or of the iridocorneal angle (NVA) developed in 10% of eyes initially classified as “perfused” or nonischemic (fewer than 10 disc areas of capillary nonperfusion). By contrast, NVA/NVI developed in 35% of nonperfused (“ischemic”) eyes within 3 months. Fewer than 5% of patients with initial vision of 20/40 or better developed neovascularization.47,50
On the basis of the CVOS findings, several recommendations can be made:47,50,59,60
- The extent of retinal ischemia (capillary nonperfusion demonstrated by fluorescein angiography) and the patient’s risk for developing neovascularization should be established; patients in whom fluorescein angiography is impossible should be treated as if they were ischemic.
- All patients with ischemic CRVO and those at high risk for conversion to ischemic status should be followed up monthly for 6 months with undilated slit-lamp biomicroscopy, gonioscopy, and dilated funduscopy.
- Patients with initial visual acuity of 20/40 or better are less likely to develop neovascularization and may be followed up every 1 to 2 months for the first 6 months and at longer intervals thereafter if stable.
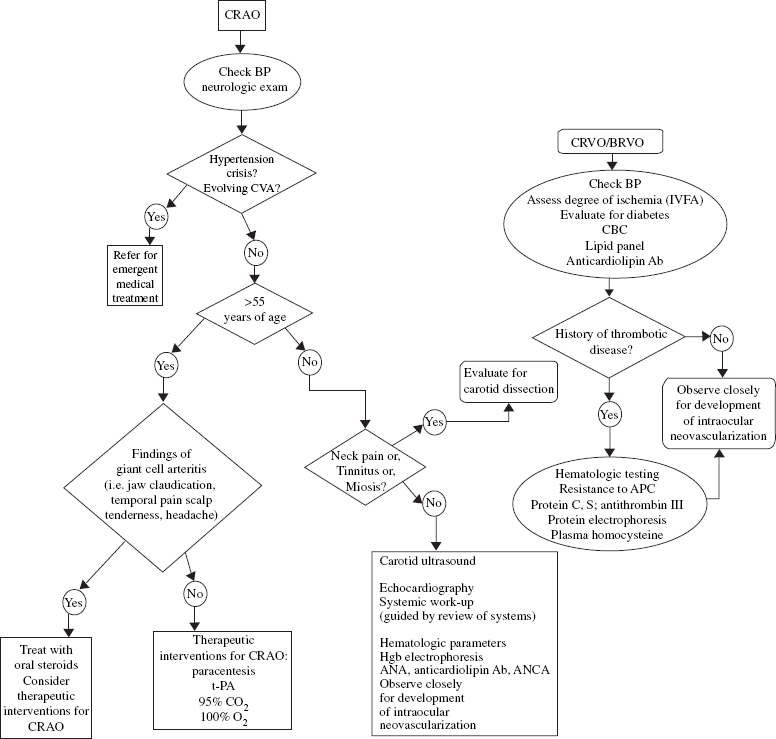
FIGURE 12–6. Evaluation and initial management of acute retinal vascular occlusion. CRAO, central retinal artery occlusion; CVA, cerebrovascular accident; CBC, complete blood count; t-PA, tissue plasminogen activator; APC, activated protein C; ANA, antinuclear antibody; BRVO, branch retinal vein occlusion; Ab, antibodies; ANCA, anti-neutrothir cytoplasmic antibodies; IVFA, intravenous fluorescein angiography.
- PRP should be applied when two clock hours of NVI or any NVA develops. Treatment in the CVOS consists of 1000 to 2000 spots of argon-green or blue green laser (500- to 1000-μm spot size, 0.2 seconds in duration, spaced 0.5 to 1 burn-width apart, to produce a medium-white burn at the level of the retinal pigment epithelium, or RPE). PRP may be supplemented if neovascularization persists.
- In patients younger than 60 years with vision of 20/50 or worse and good macular perfusion, grid photocoagulation may be considered. A trend toward visual improvement was seen in this subgroup of patients but because of small sample size did not achieve statistical significance.
- PRP should be applied when two clock hours of NVI or any NVA develops. Treatment in the CVOS consists of 1000 to 2000 spots of argon-green or blue green laser (500- to 1000-μm spot size, 0.2 seconds in duration, spaced 0.5 to 1 burn-width apart, to produce a medium-white burn at the level of the retinal pigment epithelium, or RPE). PRP may be supplemented if neovascularization persists.