12 
Definition of the Problem
Based on current teaching regarding glaucoma, glaucoma associated with ocular surgery can be defined as any evidence of optic nerve deterioration and visual field loss that follows either extraocular or intraocular surgery. However, given that such complicated instances have traditionally included problems that occur acutely, prior to the onset of changes in either the optic nerve or visual field, for the purposes of this chapter we will include those instances in which the intraocular pressure (IOP) is simply elevated. However, elevated IOP is simply a risk factor and should not be defined solely in one’s definition of glaucoma.
Epidemiology and Importance
Elevated IOP is important to recognize following any surgery given its significant role as a risk factor in some patients as a key “driver” for developing glaucoma. A transient increase in IOP is certainly less worrisome than a 20% or greater sustained increase that may occur in a patient with moderate or severe cupping of the optic nerve. Over time, patients may develop the characteristic changes in the optic nerve and/or the visual field if the unsuspecting clinician fails to closely monitor the patient’s course.
There is a range of glaucomas that can follow ocular surgery, from a steroid-induced glaucoma, which may occur following any extraocular or intraocular procedure, to angle closure, which may follow a scleral buckling procedure. Because all of these glaucomas are due to another reason, they are considered “secondary” However, these complications, which may follow ocular surgery, can be either open angle or angle closure in nature.
These glaucomas may be further broken down according to a mechanistic classification. The secondary glaucomas can be classified into three subcategories: (1) pretrabecular, (2) trabecular, and (3) posttrabecular. Examples of pretrabecular glaucomas are represented by glaucomas such as neovascular glaucoma, in which a fibrovascular membrane is present, or by the occurrence of epithelial down-growth following a complicated procedure. When red blood cells obstruct the trabecular meshwork, such as ghost cell glaucoma or hemorrhagic glaucoma, the trabecular meshwork becomes the primary factor that contributes to elevated IOP. Sometimes, however, the site of resistance is beyond the trabecular meshwork. When there is an elevation in episcleral venous pressure, as in Sturge-Weber syndrome, or there is a carotid-cavernous fistula, the intraocular pressure can be significantly affected. For those patients who present with a secondary angle-closure glaucoma, one can consider either an anterior or “pulling” mechanism or a posterior or “pushing” mechanism. The anterior secondary angle closure would be typified by neovascular glaucoma or iridocorneal endothelial syndrome. The posterior or pushing mechanism can be further subdivided into pupillary block, such as an intumescent lens, or an elevation in pressure that occurs in the absence of pupillary block, such as ciliary block glaucoma.1 whichever classification one uses, it is important to recognize and address the underlying cause prior to undertaking aggressive intervention, which can worsen the problem.
What Are the Demographic Characteristics of Patients Who May Develop Glaucoma After Ocular Surgery?
There is no age, gender, race, or ethnic group predilection for any of these glaucomas. However, there are certain ocular characteristics that may make some problems more likely to occur. For example, an eye that may be significantly hyperopic will be more likely to develop malignant glaucoma following laser iridotomy. Similarly, a patient on chronic miotic therapy may also develop malignant glaucoma following filtration surgery. An eye that has evidenced an elevation in IOP prior to cataract surgery would be more likely to develop an elevation in IOP following surgery. Moreover, known steroid responders need careful monitoring in the postoperative period.
What Are the Biological Characteristics of Patients Who May Develop Glaucoma After Ocular Surgery?
There are no biologic characteristics, such as blood levels of antibodies, chemicals, and enzymes, cellular constituents of the blood, and measurements of physiologic functions of different organ systems, that are characteristic for glaucomas associated with ocular surgery.
What Are the Social and Financial Factors of Patients Who May Develop Glaucoma After Ocular Surgery?
Physicians need to assess the patient’s ability to pay for the surgical expenses and postoperative medications before undertaking any surgery. Referral to appropriate social agencies and counseling is essential.
What Are the Personal Habits of Patients Who May Develop Glaucoma?
There are no personal habits, such as tobacco or drug abuse, diet, and physical exercise, which are likely to contribute to the development of these glaucomas. Patients who are noncompliant with their medications and those with no family or social support warrant careful postoperative observation.
What Are the Genetic Characteristics of Patients Who May Develop Glaucoma After Ocular Surgery?
A patient who may have a genetic predilection for glaucoma has a higher risk of developing a glaucoma associated with ocular surgery. Any surgical trauma may trigger the condition. See Chapters 1, 2, and 5 for discussions regarding the genetics of these diseases.
Diagnosis and Differential Diagnosis
How Is Glaucoma Associated with Ocular Surgery Diagnosed?
Glaucoma associated with ocular surgery is diagnosed as in other glaucomas. A comprehensive history is necessary, and should include reports of previous trauma, previous reports of elevated pressure, or the ingestion or topical use of steroids or other medications that can confound the clinical picture. A discussion with the referring physician would also be helpful to determine if there were unusual occurrences during prior surgery.
An evaluation of the optic nerve and the visual field are key steps to assessing the level of damage. However, it is important to determine if there are any anatomic changes that can be addressed to alleviate any significant increase in IOP. The ongoing medical or surgical management of the eye will be dependent on the outcome of gonioscopy, disc evaluation, and perimetry.
Can Glaucoma Occur with Any Type of Surgery?
Generally, yes. Patients who undergo even extraocular procedures such as strabismus or refractive surgery can develop steroid-induced glaucoma, for example. Patients who are susceptible may develop an elevation in IOP after 2 weeks or more of continuous use of steroids. It is estimated that 5% of nondiabetic and 20% of diabetics may potentially evidence an increase in IOP.2 If closely monitored and the patients have not been using topical steroids for a prolonged period of time, then stopping the offending medication will usually result in the IOP returning to baseline.
Generally, patients with preexistent glaucoma may find their condition worsening after ocular surgery. As noted previously, both open-angle and angle-closure glaucomas may be encountered in patients undergoing ocular procedures.
Can Glaucoma Occur Following Laser Procedures?
Yes, there are four laser procedures that will be highlighted here: laser iridotomy, laser photocoagulation, neodymium:yttrium-aluminum-garnet (Nd:YAG) capsulotomy, and laser trabeculoplasty.
A transient increase in IOP may arise following any intraocular procedure. However, since well-tolerated and fast-acting antiglaucoma medications have been introduced, the incidence of pressure elevation following these procedures occurs less often. Consider a series of patients who underwent laser iridotomy described by Lewis and coworkers3; 289 eyes of 179 patients underwent peripheral laser iridotomy. Patients’ diagnoses were narrow occludable angles, open-angle glaucoma, or chronic angle closure. Patients were treated perioperatively with pilocarpine and apraclonidine. No patients developed an increase in IOP of 25 mm Hg or greater. Only 0.7% of eyes with narrow occludable angles, 0.9% of eyes with open-angle glaucoma, and none of the patients with chronic angle-closure glaucoma developed an IOP elevation of more than 10 mm Hg compared to baseline. Thus, to avoid an increase in IOP in the immediate postoperative period, it is prudent to pretreat with an antiglaucoma medication such as apraclonidine, brimonidine tartrate, dorzolamide, brinzolamide, or pilocarpine. However, if a patient is chronically using an agent, the efficacy may be reduced in the perioperative period. Such reduced efficacy has been noted in patients who were chronically treated with apraclonidine and received this same drug following laser therapy.4
Malignant glaucoma or ciliary block glaucoma has been reported following laser iridotomy. This process may be worsened by the use of miotics postoperatively. It has been postulated that some of these eyes may have begun the process of aqueous misdirection prior to the completion of the laser procedure.5 Bilateral malignant glaucoma has been described in a 50-year-old patient who underwent bilateral laser iridotomies. The patient failed to respond to miotics but did respond to atropine and cyclopentolate. It was postulated that systemic hydrochlorothiazide therapy may have contributed to this presentation.6 Nevertheless, malignant glaucoma should be suspected if the anterior chamber shallows and the pressure elevates following laser iridotomy
Another secondary glaucoma that may occur in association with laser iridotomy procedures is pupillary block glaucoma. In uveitic patients, it is common for laser iridotomies to close if there is a significant degree of inflammation. When one completes a laser iridotomy using the argon laser, posterior synechiae can form. Thus, in the presence of a once-patent laser iridotomy now closed, pupillary block can occur. This phenomenon is more likely to occur if pilocarpine is used postoperatively, considering the tendency of this medication to increase inflammation.
Treatment and Management
How Are the Complications of Malignant Glaucoma and Pupillary Block, Which May Occur Following Laser Iridotomy, Managed?
Malignant or ciliary block glaucoma following laser iridotomy is initially treated with cycloplegic and mydriatic agents, agents that relax the ciliary body enabling its rotation posteriorly, and aqueous suppressants, which reduce the production of aqueous that may become loculated posterior to the vitreous. Essentially the cycloplegic agent paralyzes the circular ciliary muscle fibers and epinephrine tightens the zonules between the ciliary muscle and the lens. Using vitreous dehydrators such as isosorbide 45% at 1.5 cc/kg body weight or intravenous mannitol may assist in eliminating the continued accumulation of fluid in or behind the posterior hyaloid face as well as reduce the pressure of the vitreous body on the anterior segment. Topical antiinflammatory agents should be added to control the inflammation. Peripheral iridoplasty may also be helpful.
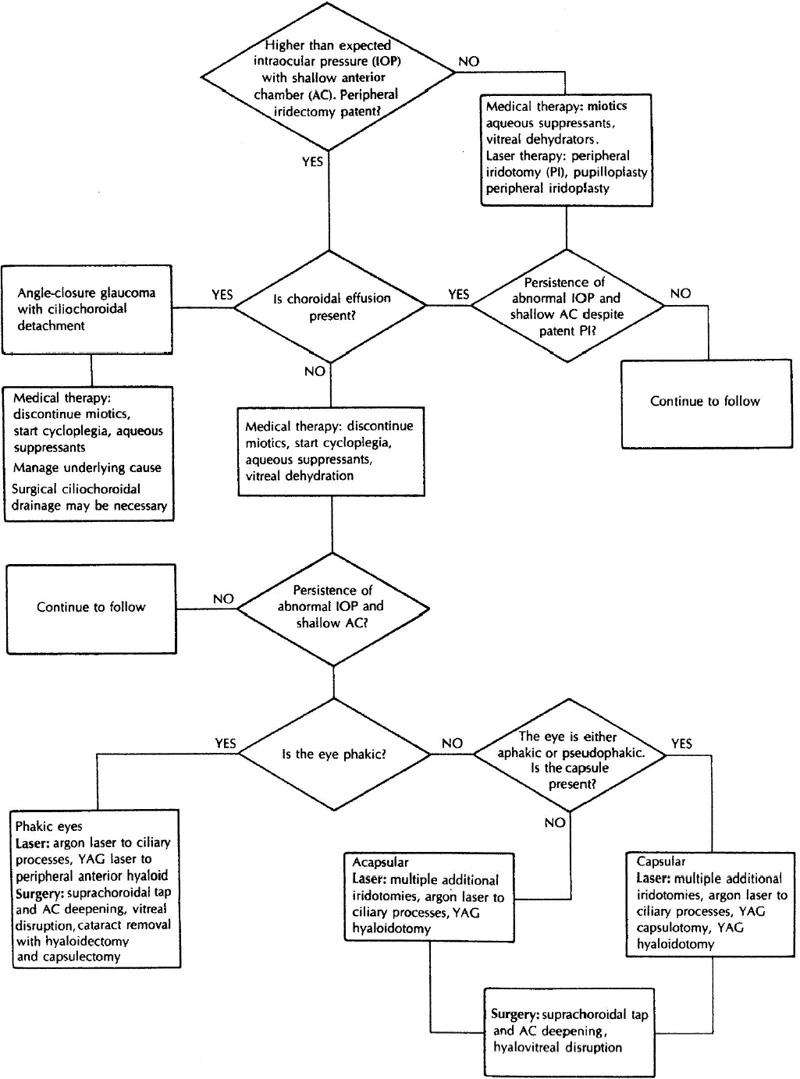
Figure 12–1 presents a decision tree that outlines the course of management for malignant glaucoma. Essentially, before one can diagnose ciliary block glaucoma, a patent iridotomy should be present. Otherwise the patient needs to be treated initially for pupillary block glaucoma with the completion of an iridotomy. If there is still a shallow chamber and the IOP is still somewhat elevated, then a choroidal effusion must be ruled out. If there is choroidal effusion, then this patient has angle-closure glaucoma with ciliochoroidal detachment. Cycloplegics and aqueous suppressants should be prescribed and the underlying cause of the ciliochoroidal detachment should be addressed. Argon laser iridoplasty can be tried, or surgical drainage of the choroidal detachment may be required if there is an excessively high IOP or corneal decompensation. However, usually patients will recover with medical therapy over time. If, on the other hand, there is no choroidal effusion, then the eye indeed has developed malignant or ciliary block glaucoma. Medical therapy should be instituted, specifically atropine 1% q.i.d., phenylephrine 10% q.i.d., acetazolamide 250 q.i.d., and a hyperosmotic agent usually b.i.d. This regimen is continued for 4 or 5 days. If this medical regimen is successful then systemic and the mydriatic agents are discontinued.7 If the problem persists then laser or surgical therapy may be necessary as outlined in Figure 12–1. If the patient is aphakic or pseudophakic, then one can proceed directly to laser or surgical therapy.
If one encounters pupillary block in a uveitic patient following an unsuccessful laser iridotomy procedure, then it is important to reestablish a patent iridotomy. The Nd:YAG laser is less likely to close, and thus completing a laser iridotomy with this laser should be attempted. Intense use of antiinflammatory agents should be considered, and systemic agents may be necessary to overcome the inflammation. Finally, if laser iridotomy is not successful, then a surgical iridectomy should be completed. However, if there is extensive permanent closure of the trabecular meshwork, then a trabeculectomy with adjunctive use of antimetabolites such as mitomycin-C should be performed.
Figure 12–1. Diagnosis and management of malignant glaucoma. (Adapted from Higginbotham EJ, Lee DA (eds): Management of Difficult Glaucoma. Boston: Blackwell Scientific, 1994.)
How Are the Complications of Laser Photocoagulation Managed?
This secondary angle-closure problem should be successfully managed by performing laser iridoplasty to deepen the angle recess, initiating cycloplegics to deepen the anterior chamber, and adding topical and systemic antiinflammatory agents. Antiglaucoma medications, particularly aqueous suppressants can be used as needed. Once the inflammatory insult has subsided, the pressure often decreases.
What Is the Etiology of Pressure Elevation Following Nd:YAG Capsulotomy and How Is It Managed?
An increase in IOP may occur following posterior capsulotomy. In a series of 897 Nd:YAG laser posterior capsulotomies, newly diagnosed glaucoma was noted in seven patients (0.78%), and five patients (0.56%) evidenced worsening of preexisting glaucoma.8
It is unknown what causes the increase in IOP following Nd:YAG capsulotomy, however, some authors have postulated that small amounts of lens and/or capsular particulates may seriously impair outflow. The Nd:YAG may also cause shock-wave damage to the trabecular meshwork.9 Patients with preexisting glaucoma are more likely to develop an IOP greater than 30 mm Hg within 1 hour following surgery.10
With the advent of α-agonists, the incidence of pressure elevation has markedly decreased. Either apraclonidine 0.5 or 1% or brimonidine tartrate 0.2% can be administered prior to or after the laser procedure, thus blunting the increase in pressure. Topical carbonic anhydrase inhibitors have also been used in this setting. Patients who are already taking an α-agonist have been shown to demonstrate less of an effect when an additional dose is given either before or after laser therapy. If the IOP is sustained, then the medical regimen will need to be adjusted. The frequency of postoperative follow-up of patients is dictated by the level of IOP following the procedure. In most instances, patients are seen in 1 week and then in 4 to 6 weeks.
Interestingly, malignant glaucoma has also been reported following Nd:YAG posterior capsulotomy. A 50-year-old pseudophakic man underwent posterior capsulotomy. The anterior chamber shallowed and the IOP increased. A laser iridotomy failed to lower the IOP. Eventually the patient responded to medical therapy, specifically, atropine, phenylephrine, mannitol, and acetazolamide. The anterior chamber deepened and the IOP decreased.11
Is There a Risk of Glaucoma Following Refractive Surgery Procedures?
Steroid-induced glaucoma must always be considered when topical steroids are continued for several weeks. Another potential problem may occur when patients undergo LASIK. During this procedure, sometimes for several seconds, a suction ring is placed on the eye, which elevates the IOP to levels of 60 to 80 mm Hg. Patients with preexisting glaucoma should be cautioned against undergoing this procedure. It is still too early to know if eyes that have undergone this procedure will have long-term problems. However, early results suggest that such a short period of pressure elevation does not significantly harm eyes without glaucoma. All of these patients should be closely monitored. Relying solely on IOP is insufficient because the thickness of the cornea is altered during refractive surgery, and the accuracy of applanation tonometry will be altered. Thus, the examination of the optic nerve and visual field will be even more important in the detection of disease.
Two studies have demonstrated that changes that occur following photorefractive surgery and LASIK decreases the ability to accurately measure IOP. Mardelli and coworkers12 measured the IOP at baseline and 12 months following photorefractive keratectomy in 111 patients. There was a statistically significant decrease in the mean tonometric measurements in the treated eyes compared to control eyes (0.5 ± 2.1 mm Hg). This difference corresponds to a reduction in corneal thickness, which measured 23 ± 23 microns. LASIK also reduces the accuracy of tonometric measurements. Emara and coworkers13 documented a mean decrease in the central corneal thickness in 85 eyes of patients who underwent LASIK. The mean central corneal thickness was decreased by 73 μ compared to baseline. The difference between the mean pre-and post-LASIK measurements by applanation was 2.5 mm Hg, which was statistically significant.
Are There Concerns Following Laser Trabeculoplasty?
Elevated IOP can occur following laser trabeculoplasty. In the Glaucoma Laser Trial the acute effects of laser trabeculoplasty was assessed; 271 eyes underwent laser trabeculoplasty as an initial intervention. The IOP rose 5 mm Hg or greater in 34% of patients after one or two sessions; 12% of eyes demonstrated an increase of 10 mm Hg or more.14 However, a study by Elsas et al15 failed to demonstrate any long-term effect of pressure spikes on the visual field following trabeculoplasty. Sixty-one patients underwent visual fields 1, 3, and 6 months following laser trabeculoplasty. There were no significant perimetric changes noted. Finally, peripheral anterior synechiae can occur following laser trabeculoplasty; however, synechiae have no adverse effect on the outcome of the procedure.
Can Glaucoma Occur Following Other Procedures?
Yes, glaucoma can occur following cataract surgery, penetrating keratoplasty, scleral buckling procedures, vitrectomy, and even glaucoma surgery. Each of these entities will be discussed in turn.
Are There Specific Types of Patients Who Are at Greater Risk for Developing Glaucoma Following Cataract Surgery Besides Those Patients Who Have a History of Glaucoma?
Yes. Patients with a history of primary open angle glaucoma uveitis, pigmentary dispersion, exfoliation syndromes, a previous history of trauma, or preexisting peripheral anterior synechiae from any cause have a risk of developing an elevation in IOP following cataract surgery2 (Table 12–1).
What Is the Incidence of an Elevation of IOP Following Cataract Surgery?
The incidence of IOP elevation is dependent on the technique and complexity of surgery and the type of viscoelastic surgery that is used. When extracapsular cataract surgery was more commonly performed, it was estimated that 55% of patients evidenced a pressure elevation of 25 mm Hg or more.16 The newer techniques of phacoemulsification and smaller incisions have resulted in lower rates of pressure elevation. Clear corneal incisions are associated with a lower risk of pressure elevation.17 These episodes are often transient; however, patients with moderate or severe glaucomatous disease should be treated prophylactically in the first 24 hours following surgery.
What Are Some of the Reasons Associated with an Increase in IOP Following Cataract Surgery?
There are several ways in which IOP may become elevated following cataract surgery. It is helpful to consider those causes that may be associated with a deep anterior chamber versus a shallow anterior chamber. First, consider a deep anterior chamber. If the incision is made at the corneoscleral limbus, then distortion of the aqueous outflow pathway can contribute to a decrease in outflow facility.18 Another reason may be that the choice of viscoelastic substance and its incomplete removal from the eye may contribute to an elevation in IOP. Among the currently available substances, such as 1% sodium hyaluronate (Healon), a mixture of 3% sodium hyaluronate (Am Visc), 4% chondroitin sulfate (Viscoat), there is no particular one that causes a pressure elevation more frequently than another. Other causes of elevated IOP following cataract surgery include pigment dispersion, hyphema, and residual lens material and epithelial or fibrous ingrowth. This latter complication is caused by poor wound construction and can be difficult to manage. The diagnosis is made by observing a scalloped border on either the corneal endothelium or the anterior iris surface. One can apply an argon laser burn to the surface and if a fluffy, white lesion occurs, then it is likely epithelium.
Presentation: | Elevated intraocular pressure and deep anterior chamber |
Causes: | Distorted aqueous outflow pathway due to wound construction |
Presentation: | Elevated intraocular pressure and shallow anterior chamber |
Causes: | Pupillary block |
If the patient presents with a shallow chamber and elevation of IOP, then the differential is as follows: pupillary block, iridovitreal block, malignant glaucoma or ciliary block glaucoma, and choroidal effusion or hemorrhage. Pupillary block occurs more commonly in the setting of an anterior chamber lens implant and less commonly with posterior chamber lens implants. Iridovitreal block may occur if the anterior hyaloid face is adherent to the posterior iris, thus limiting the egress of fluid from the posterior chamber.19 Malignant glaucoma is characterized by entrapment of aqueous in the vitreous cavity or posterior to the posterior hyaloid face and can also present as a shallow anterior chamber and elevated IOP. Finally, if the patient reports severe pain and decreased vision, then choroidal hemorrhage must be considered. This complication may occur more commonly in patients who are high myopes, in patients with previously inflamed eyes, or in elderly patients who have undergone previous vitreous surgery, in particular. The surgical management of these complications will be discussed in Chapter 11.
How Is Glaucoma Associated with Cataract Surgery Managed?
For those patients who may simply evidence a transient increase in IOP, one can initiate antiglaucoma medications as needed. Intracameral acetylcholine (Miochol) and carbachol (Miostat) can effectively lower IOP.20 Postoperatively, if a problem persists, adrenergic antagonists, α-agonists, and topical carbonic anhydrase inhibitors may be considered as potential agents that can be used. Generally it may take up to 72 hours for the pressure to return to baseline if absolutely no viscoelastic substance was removed from the eye. Latanoprost may be considered if other drugs are not effective. Antiinflammatory drugs should be used, particularly in those instances in which residual lens material is present. If the IOP elevation persists beyond the immediate postoperative period, then the patient should be monitored by undergoing serial visual fields and close observation of the optic nerve. Laser trabeculoplasty may be a consideration for those patients who are not controlled with antiglaucoma medications, once the eye has healed and is quiet.21 The success among pseudophakic patients is approximately 50% following laser trabeculoplasty. If vitreous is present in the anterior chamber, laser trabeculoplasty should not be performed.22
If there is a shallow chamber and an elevation in IOP, then one should consider the differential considered above. If there is evidence of a choroidal effusion or hemorrhage, and if the IOP is excessively elevated, then one may consider drainage of the hemorrhage. Otherwise, antiglaucoma medications (excluding parasympathomimetics and latanoprost) should be used. Over time choroidals will resorb; however, sometimes the medications may be insufficient to control the secondary pressure elevation, particularly in an eye with severe glaucoma, and surgical intervention may be necessary.
If the peripheral iridectomy is not patent or present, then a peripheral iridotomy should be performed. If iridovitreal block is suspected, then the anterior hyaloid, which may be visible through the iridotomy, should be treated using the Nd:YAG laser. If malignant glaucoma is suspected, then Nd:YAG laser applications into the vitreous may be necessary as well as the completion of an Nd:YAG capsulotomy. Immediate deepening of the anterior chamber is usually observed if vitreolysis is successful in releasing trapped aqueous.
In any case, if initial attempts to control the pressure either medically or using specific laser procedures are not successful, then filtration surgery should be performed. Because these patients have undergone previous surgery, an antifibrotic agent should be used adjunctively.
What Types of Glaucoma Occur Following Penetrating Keratoplasty?
As in glaucoma following cataract surgery, there are several causes of elevated IOP and glaucoma following penetrating keratoplasty. These entities include distortion of the aqueous outflow pathway, angle-closure glaucoma, steroid-induced glaucoma, and worsening of preexisting glaucoma.2 Each of these entities will be considered in turn (Table 12–2).
Trabecular meshwork collapse |
Tight and mid-stromal suturing |
Loss of trabecular support |
Distorted angle by same-sized corneal buttons |
Angle-closure glaucoma with peripheral anterior synechiae formation |
Pupillary block |
Chronic uveitis |
Choroidal detachment with ciliary body rotation |
Ciliary block or malignant glaucoma |
Steroid-induced glaucoma |
Worsening of preexisting glaucoma |
Adapted from Higginbotham EJ, Lee DA (eds): Management of Difficult Glaucoma. Boston: Blackwell Scientific, 1994. |
What Are the Causes of the Distorted Anatomic Changes in the Aqueous Outflow Pathway?
Tight incision closure and employing a donor button that is the same size are two causes that have been implicated. Campbell and Grant23 experimentally sutured corneas without making incisions; when sutures were tightly knotted, there was an increase in outflow facility and collapse of the trabecular meshwork. This problem rarely occurs in phakic patients and has been reported to occur in as many as 70% of aphakic eyes.24 Apparently without the countersupport of the natural lens, the trabecular meshwork fails to maintain its normal anatomy. It is unclear if a pseudophakos provides sufficient counterbalance. Finally, same-size donor buttons have been implicated, as well, in distorting the angle, thus leading to an elevation in IOP.25
What Types of Angle-Closure Glaucoma Can Occur?
As occurs following cataract surgery, pupillary block and malignant glaucoma can occur in these cases, too. Even in the absence of pupillary block, the eye can experience closure due to peripheral anterior synechiae formation, which may be due to hypotony, a flaccid iris that becomes adherent, or uveitis.
What Are Some Additional Reasons for Either Elevated IOP or Glaucoma Occurring Postoperatively?
Steroid-induced glaucoma likely occurs more commonly than suspected, given the necessary frequent use of potent steroids following postpenetrating keratoplasty. The need for long-term use of these drugs contributes to the likelihood of this problem occurring.26 Moreover, as stated earlier, if a patient has preexisting glaucoma, then it is likely that the glaucoma will worsen if one does not take the necessary precautions to avoid IOP elevation.
How Is Elevated IOP or Glaucoma Following Penetrating Keratoplasty Managed?
There is little one can do to primarily correct the distortion of the trabecular meshwork. However, one can begin antiglaucoma medications early on, primarily aqueous suppressants. Miotics and prostaglandin analogues should be avoided due to the propensity of these agents to enhance inflammation in some eyes. Alpha-agonists may be considered as either a first-line or second-line class of drugs. The question of whether one should use a topical carbonic anhydrase inhibitor is an interesting one given the presence of carbonic anhydrase II in the corneal endothelium. It is probably wise not to use the topical agent in the acute or subacute period, but use the systemic agents instead. Considering that the corneal endothelium has carbonic anhydrase isoenzyme II as an important cellular component, the application of a topical carbonic anhydrase inhibitor may affect the ability of these endothelial cells to function. Generally, one should consider using through-and-through sutures and a oversized donor graft to decrease the chances of distorting the trabecular meshwork.
For patients who evidence malignant glaucoma, treatment begins with medical therapy first, particularly in phakic patients. In pseudophakic and aphakic patients, there is the advantage of being able to proceed directly to the application of the Nd:YAG laser to the anterior hyaloid face and, if necessary, into the vitreous.
The management of steroid-induced glaucoma can be a little tricky in this setting, given the need to continue potent steroids to avoid graft rejection. It is more important to keep the inflammation controlled rather than shift to less potent steroids. There are steroids, however, that claim similar potency to Pred forte 1% (prednisolone acetate 1%) but do not elevate IOP. Vexol 1% (Rimexolone 1%) and Lotemax 0.5% (Loteprednol 0.5%) are examples of such steroid formulations and thus may be tried in this setting. Nevertheless, antiglaucoma medications can be initiated.
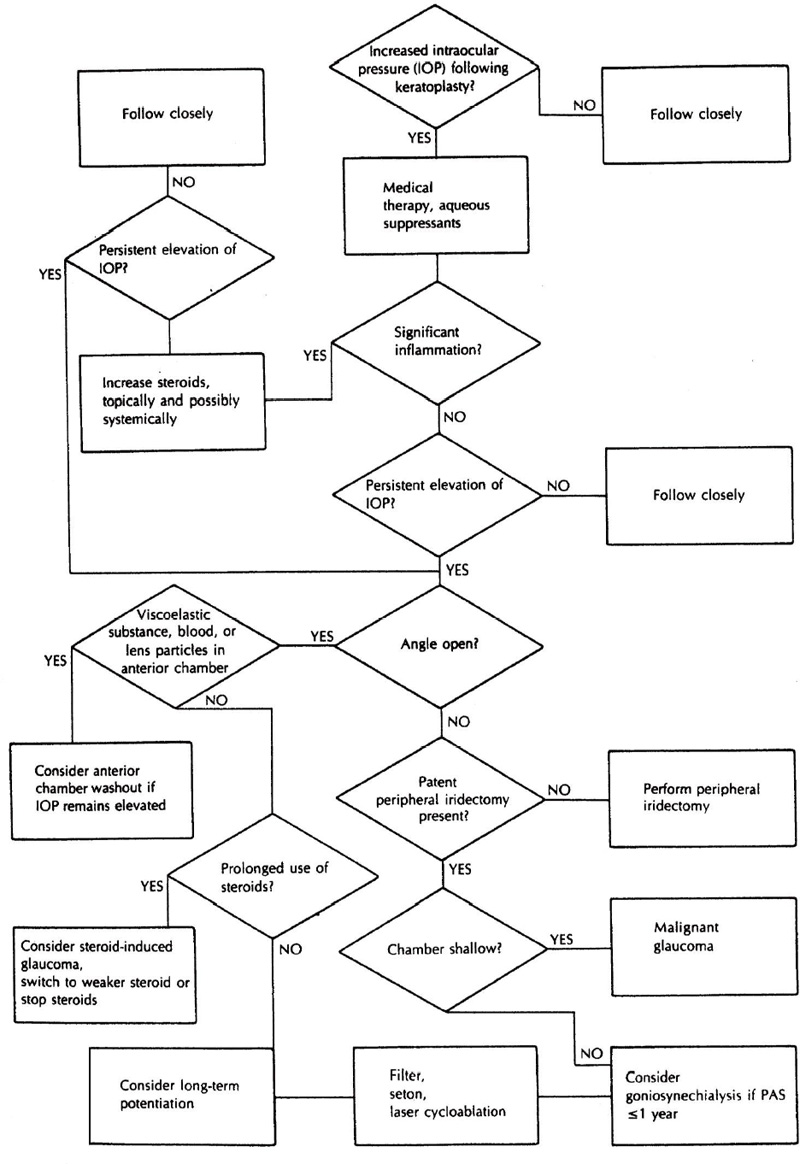
If there is significant visual field deterioration, optic nerve change or anticipated changes in either parameter in the presence of a sustained increase in IOP, then surgery may be necessary. If the angle is open and there is no previous history of laser trabeculoplasty, then this procedure can be performed. Van Meter and coworkers27 noted a 80% success of argon laser trabeculoplasty in aphakic and pseudophakic eyes following keratoplasty. Other options include a trabeculectomy with adjunctive use of antifibrotic agents, implantation of a glaucoma filtration device, or laser cycloablation. A summary of the above-discussed approach to the management of patients postkeratoplasty is highlighted in Figure 12–2.
What Types of Glaucoma Are Noted Following Retinal Surgery?
Three retinal procedures are considered here: (1) scleral buckling procedures, (2) pars plana vitrectomy, and*(3) intraocular gas or silicone oil (Table 12–3).
What Causes Glaucoma Following Scleral Buckling Procedures?
When a snug scleral buckle is applied, there is blockage of the vortex veins, which leads to increased transmural pressure in the capillaries of the ciliary processes and marked distention of the ciliary body vasculature. As the ciliary body swells, it rotates anteriorly and pushes the iris root into the angle. This mechanism has been confirmed experimentally.28,29 Pavlin and coworkers30 documented supraciliary effusions and ciliary body thickening in 15 patients 1 week following scleral buckling procedures using ultrasound biomicroscopy. Supraciliary fluid was noted in 80% of patients. The thickness of the ciliary body increased on average 0.15 ± 0.1 mm, and 55% of the patients evidenced anterior bowing of the iris. In three patients, the angle closed in one to three quadrants. In spite of these anatomic changes, none of these patients developed complete angle closure or glaucoma. Another reason may be linked to a scleral buckle that is positioned too anteriorly.
Figure 12–2. Management of the patient with postpenetrating keratoplasty-associated glaucoma. (Adapted from Higginbotham EJ, Lee DA (eds): Management of Difficult Glaucoma. Boston: Blackwell Scientific, 1994.)
Procedure: | Scleral buckling procedure |
Glaucomas: | Angle closure secondary to anterior rotation of the ciliary body |
Procedure: | Pars plana vitrectomy |
Glaucomas: | Hyphema |
Procedure: | Intraocular gas and silicone oil |
Glaucomas: | Pupillary block glaucoma |
What Causes Glaucoma Following Pars Plana Vitrectomy?
There are a variety of reasons why pars plana vitrectomy may result in glaucoma. Oftentimes, the reasons why one may decide to perform the pars plana vitrectomy may be linked to the causes of glaucoma following the procedure. First, consider blood in the anterior chamber. If there was a vitreous hemorrhage either pre- or postoperatively, then ghost cell glaucoma may develop 10 to 14 days following a fresh bleed. One may observe a layer of khaki-colored cells in the anterior chamber. Second, if a lensectomy was performed at the same time as a vitrectomy, then retained lens material may be present. Third, consider a diabetic patient who may have undergone a pars plana vitrectomy due to proliferative disease. It is not unusual to see iris and angle neovascularization occur prior to or following the procedure. Fourth, steroid-induced glaucoma is another important consideration in this setting as well as preexisting glaucoma. Finally, trauma can result in significant damage to not only the posterior segment but also the trabecular meshwork. Thus, signs of angle recession may be observed on gonioscopy.31
Malignant glaucoma has also been reported following vitrectomy. A 65-year-old without a previous history of malignant glaucoma developed aqueous misdirection following pars plana vitrectomy, scleral buckle, and extracapsular cataract extraction with posterior chamber intraocular lens implantation, despite medical therapy, Nd:YAG laser capsulo-hyaloidotomy, and surgical disruption of the anterior hyaloid face. The patient’s condition resolved after a repeat vitrectomy, which included hyaloido-capsulo-iridectomy.32 Thus, the management of ciliary block glaucoma can be challenging.
Because Intraocular Gas and Silicone Oil Are Placed in the Posterior Segment, How Can These Surgical Adjuncts Cause Problems in the Anterior Segment?
Intraocular pressure can increase within the eye if the intraocular gas bubble expands. If the patient is required to lie in a prone position, then blood and fibrin can clog the trabecular meshwork directly.33 On the other hand, if the patient is allowed to lie on his or her back, then the anterior chamber can shallow and obstruct egress of aqueous from the anterior chamber. Pupillary block can occur if the flow of fluid from the posterior segment to the anterior segment has been completely blocked.34
When silicone oil begins to emulsify, small bubbles can block the trabecular meshwork.35 Histologically, obstruction of the trabecular meshwork has been noted due to small silicone bubbles, pigmented cells, and silicone-laden macrophages.36 Higher viscosity silicone oil, the use of 5,000 centistokes, has been noted to result in fewer emulsified silicone droplets in the anterior chamber and a lower risk of glaucoma.36
Henderer et al37 of the Bascom Palmer Eye Institute in Miami, Florida, assessed the risk factors for the development of sustained IOP in a series of 532 patients who underwent silicone oil injection for the management of complex retinal detachments. Patients were further subdivided into two groups—those with and without cytomegalovirus. Among those patients with cytomegalovirus, 10% had hypotony by 6 months. By 1 year, 5.9% evidenced an elevation in IOP and 10% were noted to be hypotonous. On the other hand, among those patients without cytomegalovirus, 12.9% had an elevated IOP and 14.1% developed hypotony by 6 months. At 1 year, there were 21% of patients with an elevation in IOP and 27.3% evidenced hypotony. Risk factors for an elevation in IOP include previously diagnosed glaucoma, diabetes mellitus, and an already-high IOP.
How Are Such Difficult Glaucomas Managed?
One’s initial approach should be medical management, beginning with adrenergic antagonists and topical carbonic anhydrase inhibitors. Depending on the magnitude of the pressure elevation, then systemic carbonic anhydrase inhibitors may be required. Acetazolamide 250 mg q.i.d. will often control the pressure more consistently than the sequels in this acute period. It may be necessary in these acutely inflamed eyes to use topical steroids and even systemic steroids.
If there is pupillary block due to a gas bubble, for example, then a laser iridotomy should be performed. In the setting of silicone oil and pupillary block, an inferior laser iridotomy should be performed. If there is anterior rotation of the ciliary body due to a tight buckle, then peripheral iridoplasty or gonioplasty should be attempted. In those patients in whom the silicone oil is a problem, laser cycloablation may be the first choice. If the silicone oil is fairly compartmentalized, consider a filtration device.
Evidence of ghost cell glaucoma would suggest the need to wash out the anterior chamber. Similarly, retained lens material that is problematic should be removed. In patients who chronically have an increase in IOP and loss or anticipated loss of field or neuroretinal rim deterioration of the optic nerve, trabeculectomy with an antifibrotic agent or filtration device should be considered.
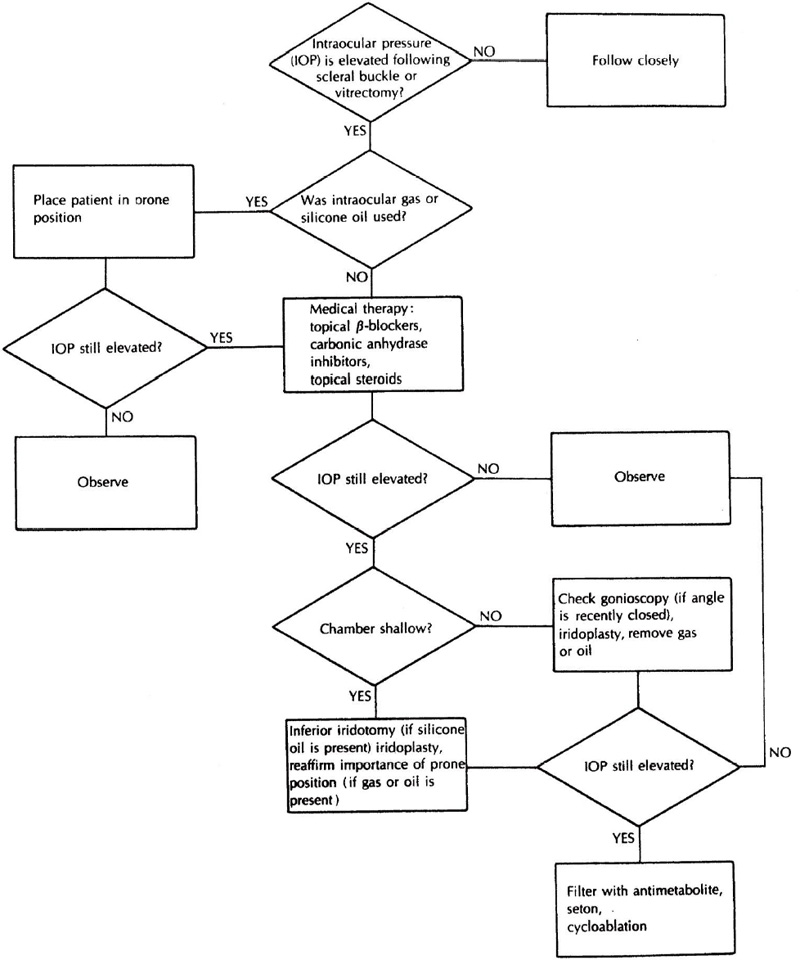
It may be necessary to remove some of the intraocular gas if the IOP is excessively elevated. IOP elevation has been associated with central retinal vein occlusion.33 A summary of the treatment of patients following retinal surgery is shown in Figure 12–3.
Figure 12–3. Management of the patient after vitrectomy and scleral buckle. (Adapted from Higginbotham EJ, Lee DA (eds): Management of Difficult Glaucoma. Boston: Blackwell Scientific, 1994.)
Even Following Glaucoma Surgery, Can There Be a Sustained Increase in IOP?
Yes, any time the eye is mechanically changed, there can be an undesirable outcome. Consider the possibilities of a sustained increased in IOP following trabeculectomy, glaucoma filtration device surgery, and laser cycloablation.
In a trabeculectomy, if the anterior chamber is deep and the pressure is high, one must consider the following: (1) blocked sclerostomy, (2) tight flap sutures, (3) choroidal effusion or hemorrhage, (4) steroid responder, (5) Tenon’s cyst or encapsulated bleb, (6) failed bleb, or (7) endophthalmitis. If the anterior chamber is shallow and the IOP is elevated, then consider the following: (1) pupillary block glaucoma, (2) malignant or ciliary block glaucoma, or (3) choroidal effusion or hemorrhage. The management of these entities is covered in other chapters.
When glaucoma filtration devices are used, there is a hypertensive phase that occurs 3 to 4 weeks following surgery, after which the IOP decreases. However, over time there may be a steady increase in pressure, which will require the initiation of antiglaucoma medications or potentially additional surgery. Entities to consider if faced with a sustained increase in IOP include the following: (1) blocked tube, (2) encapsulated bleb, and (3) steroid responder.
Finally, with regard to cycloablation the following scenarios should be considered: (1) inadequate treatment or (2) steroid responder.
Future Considerations
With the advent of newer techniques for performing cataract surgery, the risks of sustained elevation in IOP will continue to diminish over time. Smaller incisions and less reliance on viscoelastic substances throughout the procedure will minimize the distortion of the anatomy of the globe. Preventive measures such as pupilloplasty and larger donor grafts for avoiding glaucoma following penetrating keratoplasty are commonly employed. The introduction of valved filtration devices, which are easier to insert and manage postoperatively, facilitate one’s ability to control those patients who were once considered refractory to treatment.
There are new antiglaucoma medications, including combination drugs such as CoSopt (combination of timolol maleate and dorzolamide hydrochloride), and a drug which combines latanaprost and timolol. Medications on the horizon such as hypotensive topical lipids, new prostaglandin analogues, and neuroprotective agents such as systemic memantine will also provide additional therapeutic options for our patients.
Antifibrotic agents such as mitomycin-C and 5-fluorouracil have changed the number of patients who are now successfully filtered; future agents, however, which include antibodies to cytokines and growth hormones, may cause less hypotony than what is generally seen with these current agents. There have been many advances in ocular surgery that have improved the outcomes of our patients. There are still many more advances we can expect in the future.
References
2. Higginbotham EJ, Lee DA (eds): Management of Difficult Glaucoma. Boston: Blackwell Scientific, 1994.
5. Cashwell LF, Martin TJ: Malignant glaucoma after laser iridotomy. Ophthalmology 1992;99:651–659.
7. Epstein DL (ed): Chandler and Grant’s Glaucoma, 3d ed. Philadelphia: Lea & Febiger. 1986.
22. Reiss G, Wilensky J, Higginbotham EJ: Laser trabeculoplasty. Surv of Ophthalmol 1991;35:407–428.
33. Abrams GW, Swanson DE, Sabates, et al: The results of sulfur hexafluoride gas in vitreous surgery. Am J Ophthalmol 1982;94:165–171.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree