18
18 
Principles and Complications of Medical Therapy of Glaucoma
Rick E. Bendel and Mark S. Juzych
Definition
How are the Principles and Complications of Medical Therapy of Glaucoma Defined?
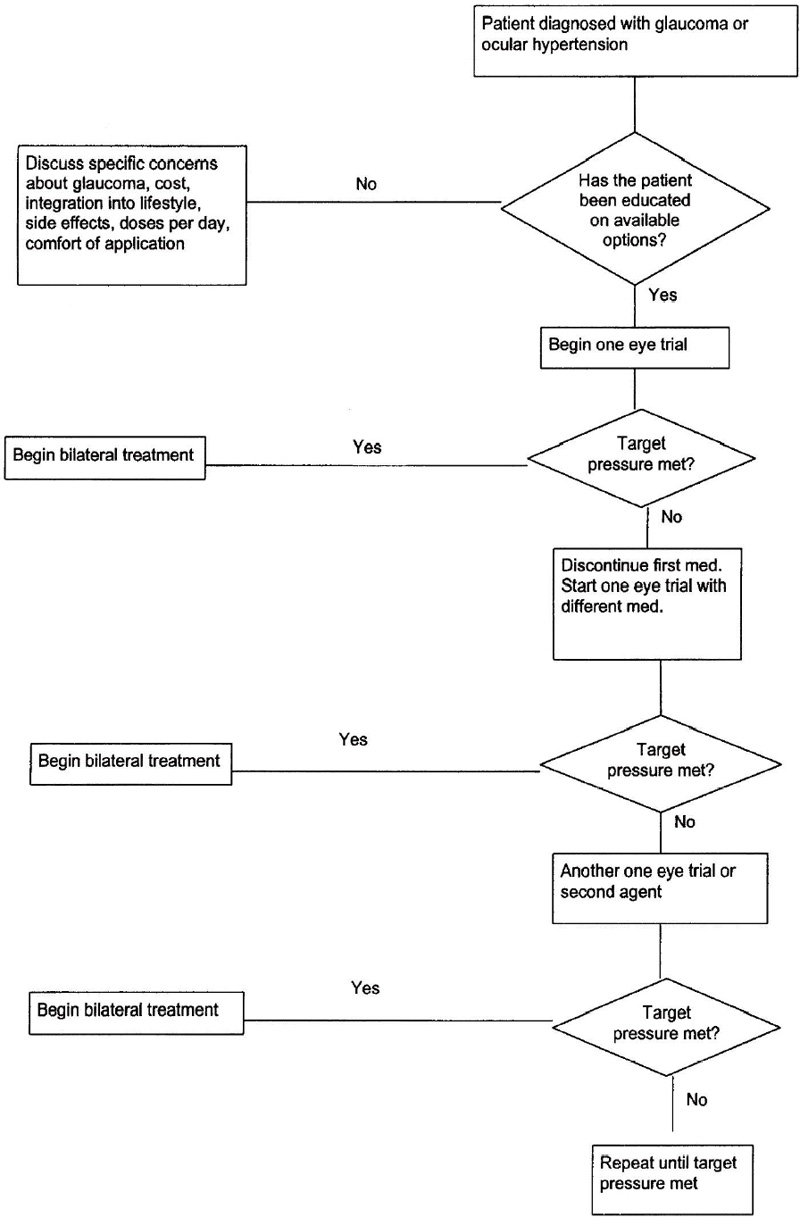
There are numerous recommendations on how to best use all of the available therapies for treating glaucoma patients. Such a proliferation of therapies indicates that no one pathway is best for any given patient, although now more than ever there are several good options. The six classes of drugs—miotics, beta-blockers, α-agonists, epinephrine derivatives, carbonic anhydrase inhibitors, and prostaglandin analogues—offer more than 20 different medications. Therefore, treatment must be tailored to each patient individually. (Tables 18–1 and 18–2 and Fig. 18–1).
This chapter offers an overview of the medications and their profiles, the importance of patient compliance, and how to optimize the lifelong treatment of glaucoma patients.
α-Adrenergic Blocking Agents COSOPT (dorzolamide hydrochloride-timolol maleate ophthalmic solution) Betagan Liquifilm (levobunolol hydrochloride) Betimol 0.25%, 0.5% (timolol hemihydrate) Ocupress ophthalmic solution, 1% sterile (carteolol hydrochloride) OptiPranolol (metipranolol 0.3%) sterile ophthalmic solution (metipranolol hydrochloride) TIMOPTIC 0.25% and 0.5% (timolol maleate ophthalmic solution) in OCUDOSE (dispenser) TIMOPTIC 0.25% and 0.5% (timolol maleate ophthalmic solution) TIMOPTIC-XE 0.25% and 0.5% (timolol maleate ophthalmic gel-forming solution) Selective β-Adrenergics Betoptic ophthalmic solution 0.5% (betaxolol hydrochloride) Betoptic S ophthalmic suspension 0.25% (bextaxolol hydrochloride) Carbonic Anhydrase Inhibitors Azopt ophthalmic suspension 1% (brinzolamide) COSOPT (dorzolamide hydrochloride-timolol maleate ophthalmic solution) Daranide tablets (dichlorphenamide) Diamox intravenous and tablets (acetazolamide) Diamox sequel (acetazolamide) Neptazane tablets (methazolamide) TRUSOPT sterile ophthalmic solution 2% (dorzolamide hydrochloride ophthalmic solution) Hypertonic Agents OSMOGLYN oral osmotic agent (glycerin) ISMOTIC (isosorbide) Miotics Humorsol sterile ophthalmic solution Phospholine iodide ophthalmic solution (echothiophate iodide) MIOSTAT intraocular solution (carbachol) Ocusert Pilo-20 and Pilo-40 ocular therapeutic system (pilocarpine) Pilopine HS ophthalmic gel (pilocarpine hydrochloride) Pilocarpine ½%–10% —Pilagan (pilocarpine nitrate) —Pilocarpine hydrochloride Carbachol 0.75%–3.0% Prostaglandins Xalatan sterile ophthalmic solution (latanoprost) Sympathomimetics Alphagan ophthalmic solution 0.2% (brimonidine tartrate) EPIFRIN 1% sterile ophthalmic solution (epinephrine) Iopidine 0.5% ophthalmic solution (apraclonidine hydrochloride) IOPIDINE 1% sterile ophthalmic solution (apraclonidine hydrochloride) PROPINE (dipivefrin hydrochloride) |
| Medical History | Medications |
|---|---|
| Beta-Blockers | |
| Respiratory problems | Systemic beta-blockers |
| Cardiac problems | Glycosides |
| Brittle diabetes | Ca2+ channel blocker, especially verapamil |
| Hyperthyroid | |
| Impotence | |
| Depression | |
| Raynaud syndrome | |
| ? Hyperlipidemia | |
| Carbonic Anhydrase Inhibitors | |
| Respiratory acidosis | Aspirin |
| Hypokalemia | Diuretics |
| Sulfa allergy | Dilantin |
| Nephrolithiasis | Non steroidals |
| Incontinence | |
| Selective α-Adrenergic | |
| Renal failure | MAO inhibitors |
| Hepatic failure | Beta-blockers |
| Vascular disease | CNS depressants |
| Allergy | |
| Hypotension (brimonidine) | |
| Nonselective α-Adrenergic | |
| Cardiac disease | MAO inhibitors |
| Arrhythmia | Glycosides |
| Aphakia/pseudophakia | Beta-blockers |
| Hypertension | |
| Miotics | |
| Cataracts | Glycosides |
| Uveitis | Depolarizing agents (indirect agents) |
| Retinal detachment risk factors | |
| Occludable angles | |
| Bradycardia | |
| Prostaglandin Analogues | |
| Cystoid macular edema | None known |
| Uveitis | |
| Cosmesis, lash, iris, skin changes | |
CNS, central nervous sytem; MAO, monoamine oxidase. | |
Figure 18–1. Medical management of patient with glaucoma or ocular hypertension.
Epidemiology and Importance
How Important Is Compliance?
Several studies have attributed a considerable amount of visual loss to noncompliance, which may make it a leading preventable cause of blindness from glaucoma.1,2 One analysis in an urban setting indicated that 80% of visual loss in glaucoma occurred prior to presenting for diagnosis and treatment. Another 10% occurred as a result of noncompliance.2 Improper compliance with nearly all types of medications seems to occur about 50% of the time.3 Thus, a large proportion of the potentially preventable visual loss occurs as a result of noncompliance, which includes patients not filling prescriptions, as well as the improper use of medications, such as not taking them continually, discontinuing them prematurely, or taking them inappropriately. Compliance studies have consistently documented this problem. One population-based study found that administration errors precluded optimal response to therapy about 60% of the time.4 The most significant errors in taking medications occur about 40% of the time due to failure to fill the medication prescription, not taking it continually, or stopping altogether.4 The errors occurred due to a lack of patient comprehension, inadequate education, and improper prescription writing and labeling by physicians and pharmacists.
Diagnosis and Differential Diagnosis
Are Physicians Able to Judge the Compliance of Their Patients?
Most physicians assume that they have a fairly good idea about how well patients are complying by knowing them, interviewing them, and through experience. Studies have shown, however, that the doctor’s judgment of patient compliance is about the same as chance. Some 30 to 50% of patients knowingly omit doses of their medications, but not all of them will admit it to their doctor. A study of chronically used medications demonstrated that doctors overestimated their patients’ adherence to the regimen by about 50%, and patients’ overstated their adherence by about 100%.5 A study looking specifically at the compliance with topical pilocarpine using an electronic eye-drop monitor revealed a mean compliance rate of 76% [standard deviation (SD) = 24.3%].6 Based on interview, the patients stated they had taken 97.1% (SD = 5.9%) of the prescribed doses, with the highest rate of actual compliance being the 24 hours prior to their return appointment. Clinician experience and patient demographics seemed to have little impact on these estimates. In fact, one study showed that the more senior a physician, the more likely he is to overestimate compliance.7 A study in an ophthalmology residents’ clinic for compliance with follow-up of patients found that many reasons exist for noncompliance, but the only modifiable step was to decrease the length of the wait in the doctor’s office.8 Noncompliant patients are more likely to be glaucoma suspects and not on any medications. Several reasons for dissatisfaction in study patients were present including insurance, transportation problems and fear—the only thing a doctor’s office can modify is waiting time and efficiency of appointment. Eye care providers must accept that they may never really know what medications a patient is using.
Treatment and Management
How Can an Eye Care Provider Improve Patient Compliance?
Patients who understand their disease and have realistic expectations of their doctor and treatment regimen tend to be more compliant and have greater satisfaction with their health care.3 Careful and frequent supervision is associated with better compliance. Psychological and emotional issues play a larger role in determining compliance than demographic factors. Regular contact with the doctor improves compliance, as does effective communication between the two.9
With the glaucoma patient, the physician should keep the treatment as minimal as possible. Each time a new medication is started, a one-eye trial should be performed. Each medication has about an 80% chance of succeeding in a given patient. Wide diurnal variations of pressure preclude starting a drop in both eyes, as one may mistakenly judge an intraocular pressure (IOP) decrease to be a successful trial when it is in fact only a diurnal variation. Eyes tend to vary their pressure in a symmetric manner, so if a drop is put in just one eye, the physician then has a frame of reference in the contralateral eye that has not had a treatment change.
The physician should instruct patients to instill eye drops at times each day when they have other routine things to do, such as eating meals or brushing teeth. Giving the patients two sets of drops, to keep at home and at work, may also be helpful. Schedules arranged by color-coding can help simplify a regimen that might otherwise be too confusing for a patient to follow. If the patient is unable to instill the drops, the help of family members should be enlisted or an instillation device used. A study determined that eye care providers can maximize compliance by instructing the patient how to instill the drops, observing the patient administering the drop, and using combination drops whenever possible.10
What Are the Possible Ways the Conjunctiva Can React to a Topical Medication?
The effects of medications on the conjunctiva are a concern for patient comfort and the potential success of filtration surgery in the future. Medications may cause cicatrizing conjunctivitis, allergic (acute or chronic) conjunctivitis, toxic conjunctivitis (pH, tonicity, contaminants), cumulative deposition as in adrenochrome deposits, microbial imbalance, nonspecific irritation, and other subclinical cellular and ultrastructural changes.11
What Should be Done to Help Patients Reduce Their Side Effects from Any of These Medications?
Nasolacrimal duct occlusion and eyelid closure are well-established ways to increase ocular absorption while decreasing absorption into the blood.12,13 The ocular hypotensive effects of pilocarpine, timolol, and carbachol were increased by nasolacrimal occlusion, allowing half the concentration to be used as well as less frequent application.13 At the very least, patients should close their eyes for 1 minute after the drop is instilled. The most optimal application of drops would be nasolacrimal duct occlusion combined with eyelid closure for 5 minutes, but most patients find it difficult to sustain eyelid closure for 5 minutes, so 3 minutes is a good compromise. Patients taking timolol reduced serum levels by 65% with eyelid closure and 67% with nasolacrimal duct occlusion.14 Another study showed that nasolacrimal duct occlusion reduced blood levels of timolol by 71%.12 Fluorescein concentration was increased by 69% in the anterior chamber by nasolacrimal duct occlusion, and lid closure alone increased it by 46%, indicating that these methods increase the concentration of the medication in the eye while decreasing the amount of drug delivered to the nasal mucosa.14
How Do Beta-Blockers Lower IOP?
β-Adrenergic antagonists reduce the production of aqueous humor, β-Adrenergic receptors have been found on the iris, ciliary body, and trabecular meshwork. A plausible theory on the mechanism of action is that beta-blockade reduces the adenylyl cyclase activity, which reduces aqueous production.15
What Are the Differences Between the Beta-Blockers?
The nonselective beta-blockers are timolol maleate, timolol hemihydrate, carteolol, levobunolol, and metipranolol. Timolol maleate is also available in a solution that forms a gel in the eye after applying. The gel maintains the medication in contact with the eye for a longer period of time and may increase efficacy and lower side effects.16 However, a study comparing the systemic effects of once daily timolol hemihydrate and timolol gel-forming solution demonstrated that there was no significant difference in IOP reduction or in systemic beta-blockade between the two medications.17 Levobunolol has the longest half-life. Metipranolol is similarly effective, although clinicians need to be aware of the reports of granulomatous uveitis in patients treated with this drug.18,19 Carteolol may have some different pharmacologic features from the other beta-blocker because of its intrinsic sympathomimetic activity, although clinical studies have not yet demonstrated this.20
Betaxolol is cardioselective by minimizing β2-inhibition. Betaxolol 0.5% stings when applied, so a 0.25% suspension was developed for comfort, and it is equally efficacious.21 The suspension is thought to slow the delivery and enable a lower concentration to be used, lessening the local irritation produced by a bolus delivery of betaxolol. Most studies have found betaxolol to be less effective than timolol and levobunolol.22,23 Timolol 0.5% lowered IOP an average of 29% compared to 26% for betaxolol 0.5%; levobunolol lowered the IOP by 6.2 mm Hg compared to 3.7 mm Hg for betaxolol 0.5% in patients with an average baseline IOP of 25 mm Hg. Betaxolol is safer to use in patients with pulmonary disease, although it may still provoke asthma.24
Daily cost of β-adrenergic therapy should also be a consideration. A comparison of drop size, cost, and wasted medication found that generic timolol maleate and Betimol were the least expensive, at 55 and 57 cents per drop, respectively. Betoptic-S and Betagan were the most costly, at $1.60 and $1.35, respectively. Timopticxe had the largest drop volume (49 μL), whereas Ocupress (31 μL) had the smallest.25
What Are the Side Effects of Beta-Blockers?
Ocular side effects can include punctuate keratopathy, dry eyes, allergic blepharoconjunctivitis, nonrefractive visual disturbances, and occasionally corneal anesthesia.26,27 A study comparing betaxolol 0.5% and timolol 0.5% demonstrated that some corneas will develop a long-lasting corneal anesthesia after use of the drops, which can predispose a patient to more serious corneal complications, such as keratitis. This is more likely to occur in patients who are older than 70. The authors recommended performing periodic aesthesiometry to identify these patients.27
All of the beta-blockers may cause or worsen congestive heart failure, asthma, chronic obstructive pulmonary disease, depression, ankle edema, disturbed sleep, weakness, dermatologic and gastrointestinal problems, bradycardia, memory problems, impotence, hyperlipoproteinemia, and confusion, and may worsen Raynaud’s syndrome and myasthenia gravis.26–29
What Are Important Interactions Between Beta-Blockers and Calcium Channel Blockers?
Increased risk of lower blood pressure, bradycardia, atrioventricular (A-V) block, and even asystole are considerations for patients combining these medications. Verapamil is of special concern as cases of complete heart block, A-V nodal delay and sinus node dysfunction have been reported when timolol was used in combination with this calcium channel blocker.30,31 If a calcium antagonist needs to be used concomitantly with beta-blocker therapy for glaucoma, one should be used that has little effect on heart rate or conduction.
What About the Use of Topical Beta-Blockers and Diuretics?
Increased risk of systemic hypotension and the use of both drugs can increase hypolipoproteinemia. Thiazide diuretics are more likely to increase blood sugar and triglyceride levels.32
What About the Use of Topical Beta-Blockers and Cardiac Glycosides?
Most commonly, bradycardia may be potentiated. The risk of A-V dissociation is increased, and there are case reports of cardiac arrest.32 Xanthopsia is usually a symptom of digitalis toxicity, and with glaucoma medications it may also present as decreased visual acuity without xanthopsia.33
What About the Use of Topical Beta-Blockers and Angiotensin-Converting Enzyme Inhibitors?
These drugs are relatively safe to use together as long as the increased risk of systemic hypotension is addressed.
What Happens When Systemic and Topical Beta-Blockers Are Used at the Same Time?
All of the side effects of the topical beta-blockers may be exacerbated. It is important to remember that systemic administration of beta-blockers lowers IOP, and that topical administration is often less efficacious when these agents are taken orally.34 Special consideration must always be given to the cardiopulmonary status of any patient on topical and systemic beta-blockers concomitantly.
What About the Effects of Beta-Blockers on Blood Lipid Profiles?
Nonselective beta-blockers have been shown to unfavorably affect the lipid profile by reducing high-density lipoprotein (HDL) levels and increasing triglycerides35; at present there is no evidence to indicate that these changes affect the clinical outcome of the patient. Carteolol may have a slight advantage over other beta-blockers in that one study demonstrated a 3.3% reduction of HDL compared to an 8% reduction with timolol.35 The 58 healthy males in this study also showed a 4.0% increase in the total cholesterol (TC) to HDL ratio while taking carteolol, and a 10.0% increase in this ratio while on timolol 0.5%. The drugs were taken twice a day with no nasolacrimal duct occlusion. A recent 12-week study compared timolol 0.5% twice daily to carteolol 1% twice daily in women over 60 with open-angle glaucoma or ocular hypertension. The investigators found no change in HDL and TC/HDL while the patients were on carteolol, but found a decrease of HDL and an adverse effect on TC/HDL while the patients were on timolol.17 This may be due to the intrinsic sympathomimetic activity of carteolol. Although the studies are still considered preliminary, some ophthalmologists prefer carteolol to other beta-blockers in patients with unfavorable lipid profiles.
What About Patients Being Treated for Diabetes?
Adult-onset diabetes is an important risk factor in treating glaucoma. With multiple medical regimens for a patient to follow, compliance will become even more difficult, increasing the likelihood of complications. One of the most important complications of diabetic treatment is hypoglycemia. Beta-blockers can blunt or mask the symptoms of hypoglycemia, lower blood sugar, and delay recovery.32
Are There Other Systemic Medications to Keep in Mind When Treating a Patient with a Topical Beta-Blocker?
Hormonal replacement therapy in women may increase headache when used with a beta-blocker. Some beta-blockers have shown increased effect when used concomitantly.16 Aspirin and nonsteroidal antiinflammatory drugs can decrease the effect of beta-blockers. A patient treated with thyroid hormonal supplementation and converted to an euthyroid state may have a reduced effect of the beta-blocker.
How Do Carbonic Anhydrase Inhibitors Work?
They primarily work to decrease aqueous humor production by inhibiting the formation of bicarbonate in the ciliary processes, which is linked to sodium secretion to form aqueous. Systemic acidosis decreases aqueous formation, and although oral carbonic anhydrase inhibitors create a metabolic acidosis, it is unclear what amount of reduction in aqueous production this may cause.36
What Are the Different Carbonic Anhydrase Inhibitors Available?
Oral and topical carbonic anhydrase inhibitors are used to treat glaucoma. The oral agents that have been used in the chronic treatment of glaucoma include acetazolamide, methazolamide, ethoxzolamide (no longer available), and dichlorphenamide. Topical agents include dorzolamide and brinzolamide.
Acetazolamide is available in tablets, and is generally taken in doses of 125 to 250 mg four times a day. A twice-a-day slow-release capsule (Diamox Sequel 500 mg) is available. Methazolamide is available in 25- and 50-mg 50-tablets and administration is two or three times a day, up to 100 mg three times a day. Its half-life is 14 hours compared to 5 hours for acetazolamide. It produces less metabolic acidosis and fewer side effects compared to acetazolamide tablets, but is slightly less efficacious.37 One study showed a greater tolerance for Sequel compared to methazolamide.38 Dichlorphenamide has similar or perhaps greater efficacy at 25 to 50 mg up to three times a day, but is less well tolerated.38 The investigators in this study questioned whether maximal efficacy is associated with more severe side effects, which may indicate more extensive biochemical alterations from the medication.
Dorzolamide 2% was the first topical agent available, with brinzolamide 1% recently becoming available (used two to three times a day).
How Well Do the Topical Carbonic Anhydrase Inhibitors Work Compared to Timolol?
Dorzolamide 2% three times a day reduced the IOP by 22% at peak and 18% at trough.39 A 12-month double-masked study comparing timolol maleate 0.5% and betaxolol 0.5% twice daily and dorzolamide 2% three times daily found that peak IOP reduction measured 2 hours after instillation was not statistically different between the three medications.40 The trough IOP at 5 and 8 hours after instillation revealed that timolol’s IOP reduction was significantly better than betaxolol and brinzolamide, although the trough IOPs of the latter two were not significantly different from one another. Brinzolamide 1% administered twice and three times daily was compared to dorzolamide 2.0% three times daily and timolol maleate 0.5% twice daily41 In both dosing regimens brinzolamide was statistically equivalent to dorzolamide thrice daily, although neither of the drugs was as effective as timolol.
How Well Does Dorzolamide Work with Timolol, Now that the New Timolol/Dorzolamide Combination Drop has Become Available?
Aqueous flow reduction was found to be 18% for dorzolamide alone and 47% for timolol alone, and that the two used together were nearly completely additive at 55%.42 Note that in this study the aqueous inhibitory affect of timolol was 2.6 times as great as dorzolamide. The Dorzolamide Timolol Study found that the combination drop was comparable to timolol 0.5% twice a day and dorzolamide 2.0% three times in efficacy and tolerability.43 The study did find that the group of patients taking the timolol 0.5% twice a day and dorzolamide 2.0% three times a day had a slightly lower IOP in the early morning and the greatest IOP difference at hour 8, which was 2 hours after the midday dose of dorzolamide. The slightly lower IOP in the morning and afternoon are small and not thought to be significant. Other studies have shown that dorzolamide is additive to other aqueous suppressants that have been in previous long-term use by patients prior to instituting treatment with dorzolamide.44
Are Topical Agents as Effective as Oral Agents?
From anecdotal evidence, many physicians have felt that the topical agents are not as effective as oral agents, and the answers in the literature are still not clear. Some studies have shown that the agents are equally effective. Eyes treated with dorzolamide 2.0% three times a day were compared to those treated with acetazolamide 250 mg four times a day and were found to have similar reductions in aqueous humor formation and IOP.45 Also, the previous study did not demonstrate a further reduction in IOP when dorzolamide was added to patients on acetazolamide and vice versa, concluding that they are not addictive. A different study has demonstrated that dorzolamide reduced aqueous production by 17%, whereas acetazolamide reduced it by 30%. Adding acetazolamide to dorzolamide-treated eyes reduced aqueous production by an additional 16%.46 A single dose of dorzolamide was found to have a comparable high efficacy to a single dose of acetazolamide 125 mg in preventing pressure spikes following yttrium-aluminum-garnet (YAG) posterior capsulotomy.47 Other studies have shown that there is not a significant benefit when adding acetazolamide to an eye already treated with topical carbonic anhydrase inhibitors, and they are equally efficacious in eyes already on maximal medical therapy.48
Does Dorzolamide Have Any Influence on Visual Function?
Normal-tension glaucoma patients placed on dorzolamide had improved contrast sensitivity after 2 to 4 weeks of treatment compared to controls who received placebo.49 Patients were also found to have accelerated arteriovenous passage time, but no change in blood flow in retrobulbar vessels.
How Does Dorzolamide Compare to the More Recently Released Brinzolamide?
Brinzolamide 1% twice daily and brinzolamide 1% three times daily were found to be equally efficacious to one another and to dorzolamide three times daily.41 Ocular complaints were significantly less with brinzolamide, with only 2 to 3% complaining of ocular discomfort compared to 16.4% taking dorzolamide.41 Brinzolamide has a more physiologic pH, requiring it to be delivered as a suspension, compared to dorzolamide, which is more acidic but is delivered as a solution.
What Are the Side Effects of Carbonic Anhydrase Inhibitors?
Fortunately, the most common side effects are the most benign, albeit annoying. Most patients experience transient paresthesias, urinary frequency, and a metallic taste. Other annoying side effects, such as diarrhea, fatigue, malaise, nausea, renal colic, decreased libido, abdominal pain, and depression, may continue throughout the course of treatment. More serious side effects include renal stone formation, hirsutism, and the most rare but dreaded bone marrow suppression.32 Serious and near-fatal complications such as Stevens-Johnson syndrome can occur after even one dose of an oral carbonic anhydrase inhibitor, such as after a cataract surgery or laser procedure when a single dose may be given, even when no sulfa allergy is present.50 The agents all include a sulfonamide group on their ring structure, so sulfa allergy is a contraindication. All of these side effects are much less common, but possible, with topically applied carbonic anhydrase inhibitors. During clinical trials with dorzolamide, urinary and hematologic tests were routinely performed and did not find any disturbances.51 This study suggests that the systemic inhibition of carbonic anhydrase is insufficient to produce biochemical adverse effects. Five percent of patients discontinue topical carbonic anhydrase inhibitors due to adverse reactions, most of which are ocular.
Many systemic drug interactions occur with carbonic anhydrase inhibitors and some important interactions to keep in mind are described below.
What Are Some Concerns When a Patient on Carbonic Anhydrase Inhibitors Is Being Treated with Calcium Channel Blockers?
The side effects of nausea and/or vomiting and malaise may become worse. Both of these drugs can cause paresthesias.
Is Concomitant Use of Carbonic Anhydrase Inhibitors and Diuretics a Special Concern?
Both drugs can lead to hypokalemia, which makes the adverse effects of carbonic anhydrase inhibitors worse and also causes a greater chance of toxicity from cardiac glycosides.32 The chance of developing agranulocytosis is greater when they are used together.
What About Carbonic Anydrase Inhibitors Used with Angiotensin-Converting Enzyme Inhibitors?
Both drugs can lead to bone marrow suppression.
How About Carbonic Anhydrase Inhibitors Used Concurrently with Systemic Beta-Blockers?
They are relatively safe to use together, but both can cause insomnia, dizziness, depression, and nausea/vomiting.
What Are the Special Considerations About Concomitant Use of Carbonic Anhydrase Inhibitors and Aspirin?
Both drugs can lead to metabolic acidosis and can also cause hypokalemia. There are reports of carbonic anhydrase inhibitor accumulation in the central nervous system and subsequent depression when salicylates were used together.32
Other nonsteroidal antiinflammatory drugs may decrease the efficacy of carbonic anhydrase inhibitors, and both may lead to bone marrow suppression.
How About Patients Who Are Being Treated for Diabetes with Hypoglycemics?
Carbonic anhydrase inhibitors can increase blood glucose levels. Elevated blood sugars are more poorly tolerated with lowered levels of potassium.
What Are Some Other Common Medications that Can Interact with Carbonic Anhydrase Inhibitors?
Headaches may become worse in patients on hormonal replacement. Patients on thyroid replacement may have a lower uptake of iodine by the thyroid gland. Acetazolamide has been shown to cause a significant increase in the blood levels of cyclosporine.52 Cyclosporine blood levels that have been in the safe therapeutic range have been shown to increase five times when acetazolamide is given, which enhances the likelihood of toxicity.
What Are the Different Types of Miotics?
The direct-acting agents are acetylcholine chloride and pilocarpine. Indirect-acting agents are anticholinesterases, including echothiophate iodide, demecarium bromide, and diisopropyl fluorophosphate. Carbachol has both direct- and indirect-acting mechanisms.
How Do Miotics Work?
Direct-acting agents stimulate the parasympathetic muscarinic receptor site, resulting in contraction of the longitudinal muscle of the ciliary body attached to the scleral spur, which in turn results in improved aqueous outflow through the trabecular meshwork.53,54 Indirect-acting agents inactivate acetylcholinesterases. The reversible agent demecarium inactivates acetylcholinesterase by binding to it, and the action may be reversed by slow hydrolysis. The irreversible agents bind by alkyl phosphorylation to the enzyme, resulting in its inactivation. The end result is accumulation of acetylcholine at the muscarinic receptors, increasing their degree of stimulation. Pilocarpine is generally used four times daily, carbachol three times daily, and the indirect agents once or twice daily. The frequent dosing of the pilocarpine is difficult for most patients; a weekly Ocusert delivery system is available, and a slow-release 4% pilocarpine gel administered at bedtime is also available. The other advantage of Ocusert is that the pilocarpine base is free of preservatives.
Side effects occur with the use of miotics, and a few systemic medication considerations are important to keep in mind. These adverse effects are reviewed below.
What Are the Side Effects of Miotics?
Ocular side effects are quite common. Patients usually experience a temporal and/or supraorbital headache as the medication activates the ciliary muscle, but over a short period of time this resolves. The pupillary miosis results in reduced vision in lower illumination and considerable difficulty in patients with central lens opacities. Accommodative myopia is induced which is greater in younger patients, minimal in patients over 60, and nonexistent in pseudophakes. Retinal detachment may occur, shallowing of the lens/iris diaphragm may induce acute- or chronic-angle closure, and iris cysts may develop.55,56 Although the etiology and causality of retinal detachments are not proven, conservative recommendations before starting a patient on miotics include a 360-degree retinal exam and pretreatment of chorioretinal disease. Then it is recommended to start with the lowest dose, time-released delivery when possible, and patient education should be provided.55 Although time-released pilocarpine is considered safer, it has also been associated with retinal detachments.56 Cataracts may be exacerbated or formed with the use of these agents; they are dose related and will continue to develop after cessation of therapy.57 Patients over the age of 60 appear more vulnerable to this effect, although a 13-year-old girl developed lens opacities after the use miotics for treating esotropia.58 Increased permeability of the blood-aqueous barrier occurs, which is of concern when these patients undergo intraocular surgery. Increased conjunctival fibrosis and cicatricial pemphigoid have also been reported.11 All of the above-mentioned side effects can occur with all of the miotics, but are more prevalent with the stronger indirect-acting miotics.
Patients with angle recession have experienced IOP increases after being placed on miotics. These patients probably rely more on uveoscleral outflow, which the miotics decrease.59 The authors tested this theory, and found that the rare patient with an IOP increase on miotics may experience a therapeutic IOP decrease on mydriatics.
Systemic side effects include nausea and/or vomiting, slowing of the heart, sweating, pulmonary edema, diarrhea, and bronchospasm. The activation of the muscarinic receptors on these organs causes these side effects. Corneal absorption is variable with these drops, and it is advantageous to have them instilled after other topical drops to facilitate uptake.
Can Miotics Be Dangerous to Patients Who Receive Anesthesia?
Cholinesterase inhibitors may result in prolonged respiratory depression in patients receiving succinylcholine during general anesthesia.32 The agents inhibit endogenous cholinesterase, which means that the body will be unable to inactivate succinylcholine, giving it a dramatically prolonged effect.
What Type of Interactions Can Occur with Concomitant Use of Miotics and Angiotensin-Converting Enzyme Inhibitors and/or Calcium Channel Blockers?
Headache may be worsened, vasodilatation may be increased, and hypotension may result.
What Can Systemic Beta-Blockers Do While a Patient Is on Miotics?
Bronchoconstriction may be aggravated in patients with asthmatic tendencies. Beta-blockers may increase the risk of nausea and vomiting or may result in lower blood pressure.
Thyroid supplementation may increase tremor, muscle weakness, and diarrhea. Nonsteroidals, aspirin, and hormonal replacement can exacerbate headache and the chance for nausea and/or vomiting.
What Are the Different Types of α-Adrenergic Agonists?
The major subtypes used in the treatment of glaucoma are selective and nonselective agonists. The nonselective agonists include epinephrine and dipivefrin. The selective agonists include apraclonidine and brimonidine.
How Do Nonselective α-Adrenergic Agonists Work?
Nonselective agents have both α- and β-adrenergic activity. A complex mechanism involving the autonomic nervous system and receptors in the eye results in reduction of IOP. α-Adrenergic activity decreases aqueous production, whereas β-adrenergic activity increases it60 and probably increases conventional and uveoscleral outflow.34
How Do Selective α-Adrenergic Agonists Work?
Apraclonidine lowers IOP by decreasing aqueous humor formation. Although it does not alter outflow, it may decrease episcleral venous pressure. Brimonidine decreases aqueous production and may also increase uveoscleral outflow.
What Are the Side Effects of the Nonselective α-Adrenergic Agonists?
Initial vasoconstriction followed by vasodilatation can result in hyperemia, which is not clinically significant but may be cosmetically annoying to the patient. Tearing and irritation are also quite common, with occasional episodes of brow ache and even corneal edema. Mydriasis may result in photophobia, which may be enhanced by the use of beta-blockers and may precipitate angle closure. Allergic blepharoconjunctivitis may result after long-term use in about 10 to 15% of patients,61 and adrenochrome deposits have long been known to develop.32 They cause a breakdown of the blood-aqueous barrier, and 10 to 20% of aphakic patients may develop cystoid macular edema.62,63 The incidence is probably much greater as only more significant visual loss seems to be noticed; visual loss in people who were formerly 20/20 and have dropped to only 20/30 or 20/40 may go unnoticed.62 Angiographically, the macular edema was found to be completely reversible with cessation of its use.63
Systemic side effects include tachycardia, arrhythmias, extrasystoles, hypertension and headache.61 These agents should probably be avoided in patients with hyperthyroidism or cardiac disease and in patients being treated for depression with monoamine oxidase inhibitors and tricyclics.
What Are the Advantages of the Prodrug Dipivefrin?
Its concentration is one-twentieth that of epinephrine, and as a result cardiovascular and systemic side effects are not clinically significant; furthermore, it must be activated by corneal esterases. Its local side effects are less, except that long-term use often results in a follicular conjunctivitis and hyperemia, but no adrenochrome deposits.64 Cystoid macular edema seems to occur less frequently with dipivefrin than with epinephrine, although the incidence would be expected to be similar since its efficacy is based on the intraocular concentration of epinephrine.65
What Are the Side Effects of Selective α-Adrenergic Agonists?
Ocular effects include lid retraction, conjunctival blanching and subsequent redilatation. The most annoying and common problems that occur in 10 to 50% of patients are allergic blepharoconjunctivitis and dermatitis.66 They are much more common and severe with apraclonidine, which is infrequently used today since brimonidine became available. The allergy occurs in 10 to 15% of patients on brimonidine after 3 to 9 months of treatment.
Systemic side effects are most commonly dry mouth and/or nose. The advantage of apraclonidine is that it does not easily cross the blood-brain barrier, lessening the chance of centrally mediated effects, which include inhibited central sympathetic activity resulting in fatigue, drowsiness, and hypotension.66 Brimonidine is more lipophilic and thus crosses the blood-brain barrier more easily and may cause these side effects.67
What Are Some Possible Effects Nonsteroidal Drugs or Aspirin May Have When Used with a-Adrenergics?
Both of these agents can decrease the IOP-lowering effect of the adrenergics. Sometimes when they are used together they may increase blood pressure.32
Are There Interactions with Angiotensin-Converting Enzyme Inhibitors?
α-Adrenergics may decrease their efficacy.
What About Calcium Channel Blockers and Diuretics?
Both drugs may increase the possibility of nausea/vomiting, diarrhea, and abdominal pain. Diuretics may also increase the chances of palpitations and headache.
Are There Any Concerns in Diabetics or Patients on Thyroid Supplements?
The α-adrenergics can stimulate hyperglycemia and decrease the effect of insulin. Thyroxin can increase the efficacy of adrenergics and make a patient more susceptible to a pressor response.
What Are the Available Prostaglandins?
Presently, in the United States, latanoprost 0.005% is the only available agent. Unoprostone is under investigation here and is becoming widely used in Japan and Latin America, and it seems to have fewer local ocular side effects in preliminary studies.68,69
What Are the Side Effects of Latanoprost?
The most common and disturbing side effect to patients and practitioners is the deepening of the iris color. It is much more common, up to 20 to 30%, in mixed-color irides compared to solid-color irides.70 A case report indicated that after 5 months of treatment a 13-month-old infant developed increased pigmentation with blue-gray eyes.71 Patients may experience conjunctival hyperemia when instilling latanoprost and possibly cystoid macular edema. Another side effect has become better known with unilateral use of the medication—thickening and lengthening of lashes.72 An investigator found an average of 19.5% increase in lash length, increased number of lashes, more abundant vellus hairs in the lateral canthal area, hyperpigmentation of the lashes, and increased curling. The effect is more prominent with more darkly pigmented hair. One of the first case reports of lash changes demonstrated that the changes became obvious at 14 weeks in a single-treated eye, and 8 weeks after latanoprost 0.005% was added to the contralateral eye the lashes appeared the same in both eyes.73
Systemic side effects are limited due to the low concentration and short half-life in the blood. The multicenter trials did not reveal any serious systemic side effects, but some patients do experience a flu-like syndrome, upper respiratory symptoms, and headache.32 The study involving 277 patients for 24 months in the United Kingdom did not reveal any systemic side effects.74
What Is Known About Latanoprost and Cystoid Macular Edema?
There are case reports of possible cystoid macular edema, but the causality is not clear.75 In general, these cases have occurred in eyes with a past history of retinal disease and aphakia. A recent study demonstrated increased blood aqueous disruption and an increased incidence of angiographically documented cystoid macular edema in early postoperative pseudophakes, and that aqueous flare was increased over the eyes of patients not taking latanoprost 0.005%. The aqueous flare difference was not present on the first postoperative day but rather at 3 days and 2 weeks, suggesting that latanoprost enhances the production of inflammatory mediators. However, the concurrent use of topical nonsteroidals significantly prevented these side effects while not decreasing the IOP lowering effect of latanoprost.76
Does the Time of Instillation Matter?
The clinical trials of the drug had protocols with a standardized application at 8:00 P.M. No evidence clearly indicates that the time of instillation affects the drug’s efficacy. Latanoprost was felt to be more effective when used at night because of the results of the Scandinavian arm of the clinical trials. Scandinavian patients were found to have significantly greater IOP reduction when latanoprost 0.005% was instilled in the evening compared to the morning.77 This has not been produced in any other studies and may have been caused by a difference in study design or patient population. Around-the-clock efficacy has been well demonstrated by a study instilling latanoprost 0.005% in the morning and monitoring IOP around the clock.78 The results demonstrated equally efficacious IOP reduction during the day and during the night.
How Does the Efficacy of Latanoprost Compare to that of Timolol?
Studies routinely use timolol as the standard against which other drugs are compared. Latanoprost is the only drug that has shown around-the-clock better control than timolol.70 One study has shown that latanoprost offers a significantly lower IOP than timolol, and when patients were switched to latanoprost a significantly greater IOP reduction was obtained.78 Patients who had been treated with timolol 0.5% twice daily for 1 year were switched to latanoprost 0.005% once a day, and showed an additional 8% IOP reduction.
Does Latanoprost Work with Miotics?
Logically these two medications would seem to be antagonistic because miotics decrease uveoscleral outflow by contracting the ciliary muscle, and the mechanism of action of latanoprost is to increase uveoscleral outflow. Uveoscleral outflow is theorized to occur through the interstitial spaces of the ciliary muscle, which are decreased by cholinergic agonists.79,80 A study using supramaximal dosages of physostigmine in conjunction with latanoprost found the effects to be mostly additive, although the maximal effect was less than in previous studies where latanoprost 0.005% was the only eye medication.81 Eyes suboptimally controlled on maximum tolerated medications demonstrated significantly lower IOP when latanoprost was added, and any strength of pilocarpine did not have a significant effect on its efficacy.82 The only factors in this study found to decrease its efficacy were a starting IOP of greater than 24 mm Hg and more than two previous incisional glaucoma surgeries.
How Well Does Latanoprost Work with Topical Carbonic Anhydrase Inhibitors?
Fluorophotometry revealed that latanoprost had no effect on the aqueous suppression of dorzolamide and that the two agents were additive.44,83 Aqueous humor was suppressed 13% by dorzolamide 2%, and no suppression was found with latanoprost 0.005%. The two drugs are additive but do not enhance the activity of the second drug. The authors recommend that both drugs be tried separately and then added together to see if the effect of the agents used together is superior to either drug used alone.83
Are There Drug Interactions?
No significant drug interactions have yet been reported.
What Is the Role of Hyperosmotic Agents in the Treatment of Glaucoma?
The hyperosmotic agents are used as a short-term or emergency treatment of glaucoma, such as acute angle-closure glaucoma, preparation for intraocular surgery, and with other acute IOP elevations.
What Are the Available Hyperosmotic Agents?
Intravenous agents include urea, mannitol, ascorbic acid, and sorbitol and glycerol solutions. Oral agents include isosorbide, glycerol, and ethyl alcohol. The oral agents are slightly less effective and take effect a little more slowly than the intravenous agents.84
What Are the Side Effects of the Hyperosmotic Agents?
Common side effects are diuresis, headache, and back pain, and the oral agents also commonly cause nausea and vomiting.85 The agents may cause severe side effects of volume and electrolyte derangements in patients with cardiac, pulmonary, or renal deficiencies, such as congestive heart failure and hyponatremia.32,86 Acute renal failure has also been reported in patients with previously normal renal function.87 Subdural hemorrhage has also occurred and is theorized to be a result of cortical shrinkage from dehydration, causing fragile veins to rupture.88
How Do the Hyperosmotic Agents Work?
The agents increase the serum osmolality and draw water from the eye, primarily from the vitreous.89 The IOP-lowering effect is greater the higher the IOP, and a relatively minor effect is seen in an eye with a normal IOP.90 A rebound increase in IOP is possible when the serum/vitreous gradient may reverse as a result of a lower serum osmolality following significant diuresis.
In Which Settings Are the Hyperosmotics Most Effective?
They are particularly useful for acute angle closure. Not only do they lower the IOP rapidly, but due to vitreous shrinkage they also deepen the anterior chamber.84 The reduction of vitreous hydration is also particularly useful in ciliary block glaucoma.91 Transient and dramatic IOP increase after trauma and hyphema may also be quite responsive.92 Finally, many surgeons feel that preoperative administration lowers some surgical risks during intraocular surgery, but it is not clear if there is any benefit with smaller-incision cataract surgery.
What About Using Marijuana for Glaucoma?
Interest in cannabinoids started in the 1970s when miotics, epinephrine, and oral carbonic anhydrase inhibitors were the only medications available.93 Smoking marijuana reduces IOP in about 65% of people by about 20 to 25%.94,95 Topical application has not proven effective in humans. The mechanism of its action is unclear, and it may be an epiphenomenon associated with the euphoria and relaxation; only patients who experienced a “high” had significant IOP reduction.93 Another study showed that the IOP reduction followed a decrease in blood pressure, suggesting that the mechanism may be decreased perfusion to the ciliary body.95
What Are the Side Effects of Marijuana, Inhaled or Ingested?
Ocular side effects include hyperemia, decreased lacrimation, nystagmus, blepharospasm, and photophobia. Systemic side effects of smoking marijuana include hypotension, euphoria, conjunctival hyperemia, tachycardia, and alter ation of mental status. Long-term side effects are at least emphysematous changes to the lungs and possibly changes in the hormonal system and brain.96 In a disease that requires 24-hour control and a lifetime commitment to treatment, these side effects are unacceptable. Additionally, smoking marijuana lowers IOP for only 3 to 4 hours, and control would require frequent administration. About 3,000 marijuana cigarettes would need to be smoked each year.94 In spite of these drawbacks, a recent review of the medicinal uses of marijuana has stated that further research needs to be done on its potential uses to treat glaucoma, and that there may be some settings where its use may be helpful.97
How May Cannabinoids Become a Part of Glaucoma Regimens in the Future?
Cannabinoid analogues are being developed that are capable of reducing IOP without the side effects of marijuana.98 Newer topical delivery systems and oral formulations that lack the psychoactive aspects or marijuana may make routine use of this class of drugs more feasible.94 Further research may develop this class as a new and useful medication to treat some glaucoma patients.
What Is The Best Way to Decide on and Begin Treatment?
Figure 18–1 is a simple methodical paradigm that facilitates successful, simple, and effective glaucoma treatment for every patient. Table 18–2 highlights classes of glaucoma medications to avoid with certain medical conditions and medications.
Future Considerations
What Are Some Possible Agents Being Developed for the Treatment of Glaucoma?
These include cytoskeletal agents, lipids, neuroprotective agents, and calcium channel blockers.
Cytoskeletal agents include latrunculins, cytochalasins, ethacrynic acid, protein kinase inhibitors such as staurosporin, and calcium chelators.99,100 In general, these agents seem to work by altering the architecture of the conventional outflow channels in the eye to create better outflow. Actin cytoskeleton disorganization in the trabecular meshwork can increase the outflow facility, which appears to be the mechanism of these agents.100 In monkey eyes treated with latrunculin-A, outflow facility was significantly increased without serious adverse side effects. Mechanism seems to be destabilization of the actin filament network, decreasing outflow resistance.101 Another class of agents has been designed to degrade hyaluronic acid, which seems to improve aqueous outflow.102 Preliminary studies have been encouraging.
Several ocular hypotensive lipids are being actively investigated. One of these agents, AGN-192024 0.03%, used once daily was compared to latanoprost 0.005% once daily and found to offer at least equal efficacy in lowering IOP and better diurnal pressure control.103 The lipid was found to be well tolerated and safe, with the most common side effect being mild hyperemia.
Ethacrynic acid is a loop diuretic that has been under investigation in the treatment of glaucoma since the late 1980s.104 Studies have shown that it may increase outflow facility by creating changes in Schlemm’s canal that may be related to its inhibition of microtubule assembly. The initial study showed that it significantly increased outflow facility acutely in human cadaver eyes with no obvious toxic effects.104 A topical ethacrynic acid ointment was found to effectively lower IOP in monkeys by the fifth day, and its efficacy was similar to that of timolol 0.5%. Mild eyelid edema, conjunctival hyperemia, discharge, and one corneal erosion were noted.105 Introduction of the drug has been limited by its potential for local and systemic toxicity and short duration of action. The other agents have similar challenges and potential at this time.
What Is the Role of Calcium Channel Blockers in the Treatment of Glaucoma?
Calcium channel blockers act by binding membrane-bound calcium channels and inhibiting the influx of calcium. These drugs have been under investigation for potential ophthalmic uses due to the interest in vasospasm in normal tension glaucoma and their ability to lower IOP. Studies have had variable results on the topical effects of verapamil, most demonstrating a significantly lower IOP.106,107 Topical administration was found to increase facility of outflow by 64%.106 However, an earlier study has shown that the topical use of nifedipine, diltiazem, and verapamil caused transient elevations of IOP in both humans and rabbits.108 The increase in IOP was found to be greater in rabbits than humans and may have been related to the detected increase in blood flow to the treated eye, causing a greater production of aqueous. Another investigator used a similar protocol with a much lower concentration of topical verapamil—0.125% versus 1 to 2%—and found a significant reduction in IOP.109 A biphasic response to verapamil may be present, and even with the smaller concentrations a contralateral effect was present. It remains clear that a more conclusive study needs to be performed before topical agents will have any role in the treatment of glaucoma.
Systemic administration of nifedipine showed improvement and stability in visual fields of some normal-tension glaucoma patients.110–112 One study demonstrated that normal-tension glaucoma patients had a much lower rate of progression on their visual fields—11% versus 56%—than controls not taking oral calcium channel blockers.110 Similarly, the treated low-tension glaucoma patients showed no progression of optic nerve damage compared to 44% who showed progression without the calcium channel blocker. No benefit was found in taking calcium channel blockers for open-angle glaucoma.110 One of the larger studies investigating calcium channel blockers found no benefit in visual field, IOP, or optic disc changes in 83 treated patients compared to a control group of patients.113 No detrimental side effects were noted.
A series has shown improvement of visual fields in patients taking systemic calcium channel blockers. Patients with normal-tension glaucoma felt to be associated with vasospasm tended to show improvement in visual field while taking calcium channel blockers.111 Vasospasm was determined by improved cold recovery rate in peripheral vessels while on nifedipine. Focal defects were the least responsive. A study comparing repeat performance of visual fields and measured color vision found that some normal-tension glaucoma patients on calcium channel blockers had significant performance-corrected improvement.112 Another study failed to show uniform improvement in visual field tests, but noted significant improvement in contrast sensitivity in patients who showed improved retrobulbar blood flow with nimodipine administration.114 A newer calcium channel blocker, nilvadipine, has demonstrated potential for treatment in normal-tension glaucoma.115 It has the advantage of not lowering blood pressure in normotensive patients while increasing perfusion of the optic nerve, retina, and choroid in patients with normal-tension glaucoma. This study suggests that calcium channel blockers may be beneficial for a certain subgroup of normal-tension glaucoma patients. More conclusive and prospective studies are needed before calcium channel blockers are routinely applied to the treatment of patients.
What Has Generated All the Interest in Neuroprotection?
It is well known that even in spite of good treatment, IOP reduction, and compliance, many patients will go blind from glaucoma.116 This has created a desperate search for a better way to control the damage from glaucoma. Although the etiology of visual loss in glaucoma is multifactorial and not clear in many instances, ophthalmologists concur that it is caused by the death of retinal ganglion cells. Neuroprotection therapy could potential prevent visual loss in any glaucoma patient independent of which type of glaucoma the patient has.117
Areas of research include heat shock proteins,118 glutamate toxicity, and many others. Hyperthermia prior to ischemic exposure has been found to be neuroprotective in the rat model. Isolation of these protective substrates may yield a source of neuroprotective agents.118 Brimonidine has come into the limelight recently due to a study with axonal rat crush injury that demonstrated axons survived better when treated with brimonidine.119 Retinal ganglion cells and nerve fibers treated with brimonidine showed significantly less cell death than those treated with timolol or the saline control. Additionally, the neuroprotective effect was blocked by rauwolscine, the α2-adrenoreceptor antagonist.119 Additional studies have also shown that brimonidine was also protective against several other mechanisms of nerve injury including light stress, ischemia, and calibrated nerve compression.120 This is an actively researched area by the pharmaceutical company, but as of yet no clinically relevant studies have been completed and the information is only theoretical at this point.
N-methyl-D-aspartate (NMDA) receptor antagonists are thought to have therapeutic potential in numerous central nervous system disorders ranging from acute neurodegeneration, such as strokes and trauma, to chronic neuro-degeneration, such as Parkinson’s disease.121 Memantine is felt to be one of the most well-tolerated drugs in this class. It has become of interest in treating glaucoma because it was shown to block toxicity caused by glutamate.122 Clinical studies using memantine to treat glaucoma are presently in progress. Investigators found that the NMDA antagonist eliprodil was protective against glutamate cytotoxicity in retinal neurons.123
Similar studies of medications currently used yielded neuroprotective effects based on the above models. A study using a rat retina showed that betaxolol is a neuroprotective agent and attenuates the effects on the retina induced by raising the IOP to simulate an ischemic insult, as may occur in glaucoma.124 Further study of betaxolol revealed that in addition to its IOP-lowering effects, it has calcium channel blocker activity that may enable it to be neuroprotective.125
How Can the Proliferation of Medications and Studies Enable Better Treatment of a Glaucoma Patient?
Editorials, trade journals, review journals, peer-reviewed journals, and professional meetings find that glaucoma treatment is a marketable subject. There are now more treatment options than ever before, but still some patients go blind. An editorial summarized the situation well by saying the power of experience must be carefully integrated with the databased protocols and the constraints of preferred practice plans.126
How Do Physicians Initiate, Modify, and Continue Therapy?
Perhaps the most important aspect of treatment is education and support. Clinicians are trained to rely heavily on objective indices such as IOP, perimetry, optic nerve fiber layer, and nerve head analysis and vision. Treatment has a major impact on the patient’s life. Recent studies have shown that glaucoma patients have a lower quality of life than healthy peers. Patients with glaucoma experience fatigue, and their social satisfaction and physical and mental health were significantly worse than controls.127 Knowing how glaucoma is affecting the life of the patient enables the physician to tailor treatment to the needs of the patient. The Glaucoma Symptom Scale has recently been introduced as a brief and reliable estimate of the symptoms associated with glaucoma and its treatments.128 A recent retrospective study found that the average cost of treating a newly diagnosed glaucoma patient will be about $2,100 during the first 2 years.129 Whatever the treatment course you follow it will have a major impact on your patients life. Knowing how glaucoma is effecting the lives of our patients will enable a treatment to be tailored that works best for each individual patient.
How Can Patients Become Better Informed?
In-office videos and handout literature are available to inform patients about their treatments and disease. More resources are becoming available on the World Wide Web, which enable patients to become more involved in their own treatment. Good web sites include:
- The Glaucoma Foundation—www.glaucomafoundation.org/info
- Glaucoma Research Foundation—www.glaucoma.org
- American Academy of Ophthalmology—www.eyenet.org
- Prevent Blindness America—www.preventblindness.org
- The National Eye Institute Information Center—www.nei.nih.gov
The patient’s active involvement in treatment increases compliance.
References
1. Van Buskirk EM: The compliance factor [editorial]. Am J Ophthalmol 1986;101:609–610.
3. Evans L, Spelman M: The problem of non-compliance with drug therapy. Drugs 1983;25:63–76.
26. Van Buskirk EM: Adverse reactions from timolol administration. Ophthalmology 1980;87:447–450.
28.Britman NA: Cardiac effects of topical timolol [letter]. N Engl J Med 1979;300:566.
32. Goodman LS, Gilman A, Hardman JG, et al: Goodman & Gilman’s the pharmacological basis of therapeutics, 9th ed. New York:McGraw-Hill Health Professions Division, 1996.
60. Schenker HI, Yablonski ME, Podos SM, et al: Fluorophotometric study of epinephrine and timolol in human subjects. Arch Ophthalmol 1981;99:1212–1216.
61. Becker B, Morton WR: Topical epinephrine in glaucoma suspects. Am J Ophthalmol 1966;62:272–277.
62. Kolker AE, Becker B: Epinephrine maculopathy. Arch Ophthalmol 1968;79:552–562,.
64. Wandel T, Spinak M: Toxicity of dipivalyl epinephrine. Ophthalmology 1981;88:259–260.
67. Burke J, Schwartz M: Preclinical evaluation of brimonidine. Surv Ophthalmol 1996;41:S9–18.
89. Robbins R, Galin MA: Effect of osmotic agents on the vitreous body. Arch Ophthalmol 1969;82:694.
90. Drance SM: Effect of oral glycerol on intraocular pressure in normal and glaucomatous eyes. Arch Ophthalmol 1964;72:491.
92. Kolker AE: Hyperostotic agents in glaucoma. Invest Ophthalmol 1970;9:418.
121. Parsons CG, Danysz W, Quack G: Memantine is a clinically well tolerated N-methyl-D-aspartate (NMDA) receptor antagonist—a review of preclinical data. Neuropharmacology 1999;38:735–767.
129. Kobelt-Nguyen G, Gerdtham UG, Alm A: Costs of treating primary open-angle glaucoma and ocular hypertension: a retrospective, observational two-year chart review of newly diagnosed patients in Sweden and the United States. J Glaucoma 1998;7:95–104.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree