Giant Papillary Conjunctivitis
E. Lee Stock
David M. Meisler
Renee Yang
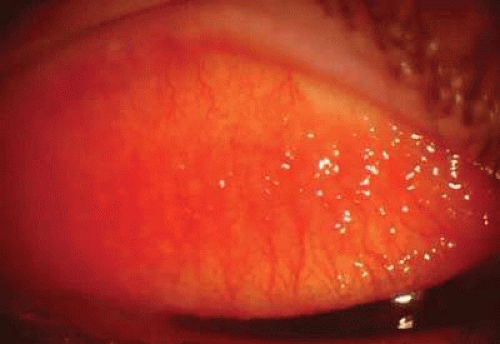
Giant papillary conjunctivitis (GPC), first described by Spring1 in 1974, is an inflammatory disorder of the external eye characterized by papillary hypertrophy of the upper tarsal conjunctiva. It is most commonly associated with contact lens wear. It has also been associated with ocular prostheses2 and exposed sutures. Itching and burning, discomfort (foreign-body sensation), and increased mucus production are the symptoms of GPC.3 Patients usually report a past ocular history of contact lens wear or ocular surgery (cataract, keratoplasty, and enucleation). The signs of GPC include mucous discharge, papillary conjunctivitis consisting of enlarged papillae (Fig. 1), lid edema, and ptosis (Fig. 2). Giant papillae are greater than 0.3 mm and are seen on the superior tarsal conjunctiva.4 GPC shares other signs with vernal conjunctivitis, including Trantas dots and limbal gelatinous elevations.5 Apical fibrotic appearing changes of the papillae have been reported clinically, but it is unclear if these changes are transient or permanent (Fig. 3). Letter
Pathophysiology
Theories involving immune and mechanical mechanisms have been espoused in the pathophysiology of GPC. Most theories implicate proteinaceous material deposited on the lens surface for either the allergic or the mechanical mechanisms to take effect.
Adsorption onto Contact Lenses
Deposits on Lenses
The adsorption of tear proteins onto the surface of hydrophilic contact lenses6 has been documented by many different methods. The deposits found on spoiled contact lenses include lipids that do not appear to be antigenic,7 and proteins. Many tear proteins that have been identified on contact lenses include lysozyme, lactoferrin, protein G, prealbumin, albumin, and immunoglobulins.8,9,10,11,12,13,14,15 All hydrogel lenses develop a proteinaceous coating that begins almost immediately after insertion.16,17,18 In a model of protein deposition, a dual layer forms over the contact lens surface immediately after insertion. The first (primary) layer that forms is composed mainly of irreversibly bound denatured proteins. The pellicle, a mucoprotein layer, is partially reversible, is denatured, and tries to equilibrate with the tear film. Lens biocompatibility is largely determined by the primary layer and its biochemical structure because the primary layer is more apt to undergo conformational changes than the second layer. It has been suggested, but not proved, that it is this protein and tear film interaction that ultimately determines whether a contact lens surface is biocompatible. If it is not biocompatible, adverse external ocular responses such as GPC may result.11,19
The type of contact lens may explain how deposits collect on the contact lens surface of patients who develop GPC. The extent to which protein is deposited on the anterior contact lens surface seems to depend on the polymer content, structure, and charge.20,21 Lenses with higher water content tend to develop more deposits than lenses with lower water content.22 The high porosity may allow more tear film components to enter and embed in the contact lens matrix.12,19,23 The net ionic charge of the polymer also influences protein buildup. Lysozyme, a positively charged protein, is attracted to negatively charged ionic materials.24,25,26 Studies have shown that lenses with both high water content and ionic properties have the greatest deposition of proteinaceous material.6,17,22,27 Furthermore, protein may not deposit uniformly on hydrogels. Some lenses tend to build up protein on the edge, compared with a more uniform distribution on lenses from other groups.28
The hydrogel fabrication process appears to induce a different protein adsorption behavior.29 Lathe-cut lenses tend to adsorb twice the amount of protein as spincast lenses.30 Another study showed lathed hydrogels to have deposits in the lathe marks even after vigorous cleaning.31
It may seem logical to assume that the greater the amount of deposit, the greater the likelihood of developing GPC. However, there has not been a definitive association between GPC with a particular lens type and the amount of protein deposited on the contact lens surface,32 further questioning the importance of proteins. Increased deposition of protein on lenses of some GPC patients may be the result of the inflammatory reaction rather than the cause of the reaction9,19 Furthermore, the deposits on soft contact lenses of patients with GPC appear no different on scanning electron microscopy from deposits on lenses of asymptomatic wearers.19
Biochemical Nature of Protein Deposits.
The biochemical nature of protein deposits rather than the quantity or appearance of bound protein may be important. For example, once lysozyme is bound irreversibly to the lens surface, it undergoes molecular conformational changes.30,31 Lens-bound protein may be denatured by shearing forces and stresses interacting at the anterior lens surface, such as cyclical drying and rewetting.23 Once lysozyme has been denatured, its interactions with other layers in the tear film are altered, and this interaction may play a role in inducing GPC.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree