9
Flexible Laryngoscopy for In-office Procedures
An aging U.S. population with higher general anesthetic risk profiles, new endoscopes with better imaging and features for office procedures, and digital recording systems have influenced a shift of upper airway procedures into the office from the operating room. Furthermore, the development of a new generation of vocal fold injectables and lasers with flexible fibers and other applications is transforming the range of opportunities for treatment of disorders of the larynx, pharynx, esophagus, and trachea.
 Background
Background
Although access to the upper airway began in the office with the introduction of mirror laryngoscopy by Garcia in 1854, the movement of endoscopy to the operating room eventually evolved for better precision and improved imaging.1 Specifically, the operating room setting provided direct, unimpeded access to the larynx, trachea, or esophagus, with better lighting and a minimum of patient movement.
In 1857, Czermak used artificial light sources and a tooth-held concave mirror to focus light into the larynx. Kirstein tirelessly promoted direct laryngoscopy in the office, which he described as “veritably a surgical method.” “Autoscopy,” as it was called, was performed with the patient in the sitting position and required an assistant to position and reassure the patient. Jackson formalized this surgical technique with his exhaustive teachings and original illustrations; he promoted the supine positioning of the patient, which heralded its evolution into an operating suite. The use of a suspension apparatus by Killian led to enhanced precision as the surgeon could employ two hands to operate.
The advent of reliable general anesthesia in the 1960s completed the triad of optimal conditions for laryngeal surgery in the operating room: direct visualization with suspension, stillness of the patient, and bimanual manipulation of tissues by the surgeon. The advances came at the expense of cardiovascular morbidity produced largely by anesthetic agents, a dilemma we still face today. The addition and popularization of microscopic laryngeal examination by Scalco, Jako, Klein-sasser, and others brought new precision through magnification.2–4 Jako’s addition of microinstruments with dimensions more appropriate to small-volume laryngeal pathology also aided in this regard, and they have not been substantially modified since their introduction in the 1960s.5
Despite the advantages of performing laryngeal surgery in the operating room, technological advances have also allowed better laryngeal visualization in the office setting. During the early 1970s, the advent of flexible fiberoptic technology and the reliable delivery of topical anesthetics such as lidocaine made awake examinations of the larynx, pharynx, trachea, and esophagus possible. Convenience, low cost, reasonable color, image veracity, and the breadth of applications soon influenced the practice of otolaryngologists, gastroenterologists, pulmonologists, and others. Rigid endoscopy of the larynx using angled telescopes transformed the field of laryngeal endoscopy in the office by allowing the consistent application of stroboscopic light. The color resolution and image resolution achieved with rigid endoscopes in the office were clearly superior to flexible fiberoptic technology, but the distance from the targeted lesion had limits; the endoscope could be angled in only so close to the larynx, limited by the tongue base.
We now live in what some have called the “Golden Age” of laryngology given the improvements in imaging, new office lasers, and vocal fold injectables. Arguably, the most influential component of the new technologies is the distal chip flexible endoscope. The most recent generation of scopes provides excellent lighting, proximal control of the distal tip, different sizes for various applications, image processing for video display, integration into photodocumentation units, and the critically important working channels. The features of upper airway endoscopes and their uses in office interventions are worth detailed discussion.
 Imaging Equipment and Access to the Upper Airway
Imaging Equipment and Access to the Upper Airway
A variety of visualizing and interventional tools are available to the surgeon for office-based procedures. Mirror laryngoscopy, though inexpensive and widely available, does not permit video archiving and is limited by patient tolerance. Mirror laryngoscopy does not permit effective visualization by a student. On the other hand, when flexible laryngoscopy is employed to examine the larynx, the endoscope is attached to a camera and a video monitor. By viewing the larynx on the video monitor, the surgeon enjoys a magnified view of the laryngopharynx, and multiple individuals can view the images simultaneously. After the examination, the images can be reviewed with the patient and family. Video archiving is also an available option when flexible laryngoscopy is employed. Archived images can be compared with subsequent examinations of the same patient, allowing a better evaluation of disease progression or response to treatment. Flexible transnasal endoscopy, using either fiberoptic or “distal chip” technology, permits excellent visualization of all segments of the upper airway.
More recently, transnasal esophagoscopes have allowed the surgeon to examine the esophagus while sparing the patient intravenous sedation. Recent reports confirm that diagnostic efficacy is comparable with that of the gold standard of larger endoscopes used by gastroenterologists.6,7 A major advance in flexible technology is the advent of working channels within the endoscope itself. These channels permit the delivery of anesthetic agents, small biopsy forceps, laser fibers, and suction. Surgeons can therefore simultaneously visualize and operate on the esophagus or upper airway without the need of an operative assistant.
Telescopic rigid endoscopy, performed transorally, is generally employed for visualization of the laryngopharynx, with or without the addition of stroboscopy. If the patient holds his or her own tongue, the surgeon can perform bimanual tasks for simultaneous transoral visualization and placement of instruments for the delivery of therapeutic agents, as described by Ford.8
Delivery of treatment agents to the larynx, such as injectable bulking materials or steroids, can be achieved transorally, transnasally, or transcutaneously. The pathway of delivery is dependent upon equipment availability, patient tolerance, surgeon preference, and the availability and/or necessity of an operative assistant. Indirect surgery has been extensively reported on by Omori et al.9 This technique employs transnasal visualization by an operative assistant using a flexible scope and transoral delivery of agents performed by the senior surgeon. Transoral delivery is often preferred as the delivery needle is directly viewed as it penetrates the vocal fold, ensuring accurate placement of the injection.8
In patients with a gag reflex that cannot be controlled with topical anesthesia and coaching, a transnasal approach is available. A needle at the tip of a flexible cannula is passed through the working channel of a flexible endoscope for delivery of a glottic injectable.10,11
Transcutaneous delivery, with simultaneous flexible laryngoscopy allowing a superior view of the larynx, is performed through the cricothyroid membrane, the thyroid cartilage, or, as recently described by Getz et al., through the thyrohyoid membrane.12–14 Transcutaneous delivery is a popular choice but may not allow the surgeon a direct view of the needle tip, which is below the vocal folds when using the cricothyroid membrane approach, potentially reducing precision.
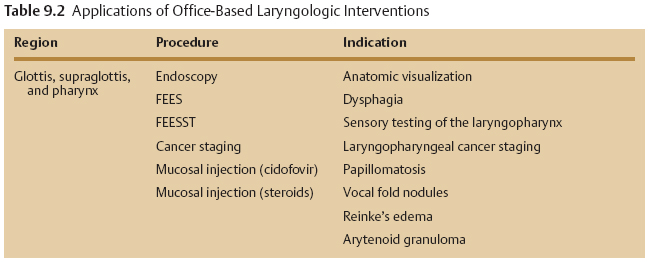
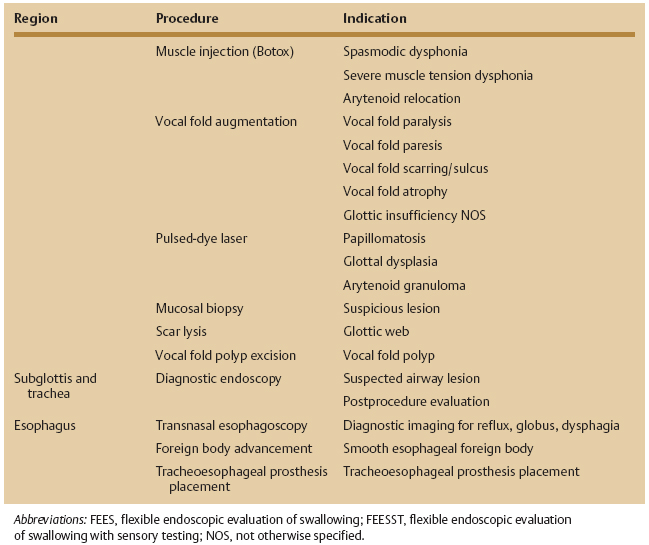
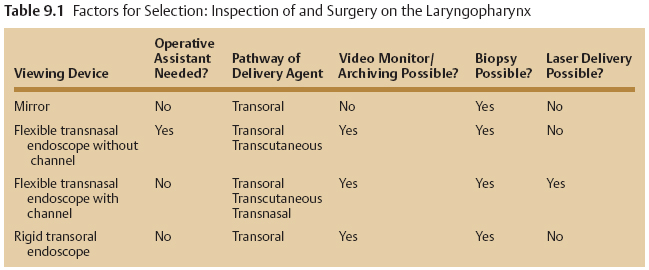
Table 9.1 lists factors to consider in the selection of procedures to be performed in the office setting.
 Indications
Indications
Office-based laryngologic procedures involve visualization of the upper aerodigestive tract, specifically the glottic and supraglottic larynx, pharynx, subglottic larynx and trachea, and the esophagus. Indications for these procedures include diagnostic imaging and/or tissue manipulation. Table 9.2 provides an overview of reported office-based procedures including the indications. Patients are selected for office-based procedures for some of the following reasons:
- surgeon preference to directly monitor vocal feedback;
- surgeon preference to enhance efficiency;
- patient preference to avoid general anesthesia;
- patient desire to reduce cost if private-pay;
- avoidance of general anesthesia if medically unsuitable;
- poor laryngeal exposure under direct laryngoscopy;
- refractory lesions previously treated under general anesthesia.15,16
 Contraindications
Contraindications
Contraindications to office-based procedures are determined by surgeon comfort, patient factors, and lesion type. If the surgeon does not possess sufficient experience with a particular technique or if there is a possible lack of necessary equipment, then microlaryngoscopy under general anesthesia should be selected.
A severe gag reflex that cannot be overcome with topical anesthesia and coaching or reduced jaw opening from trismus or temporomandibular joint disorders will likely preclude successful performance of office procedures.
Although bleeding diatheses from medications or systemic disease are cited as contraindications to office-based procedures, Bastian and Delsupehe report that none of 20 patients on aspirin, nonsteroidal antiinflammatory agents, or warfarin had airway distress, although there was a longer interval required for spontaneous coagulation.16
The type of lesion may also dictate whether a surgeon opts for office management. For example, it is generally held that benign subepithelial pathology such as nodules, polyps, cysts, and Reinke’s edema require a level of precision that office surgery does not afford.15,17,18 However, Omori et al. have reported on the extensive use of indirect surgery for removal of vocal fold polyps using specially designed instruments.9 Omori’s group, while not excising nodules or Reinke’s edema, has reported treatment using transoral steroid injection resulting in improved objective voice measures.19,20 Tai et al. caution against the biopsy of overtly vascular lesions such as hemangioma.18 If the full extent of a lesion cannot be establish by office examination, then direct inspection under general anesthesia is likely warranted. Additionally, given the delicate nature of the vocal fold and the relative imprecision of indirect surgery, Hogikyan and Pynnonen warn that biopsy of superficial lesions suspicious for malignancy may sacrifice normal tissue while not producing accurate information about the depth of lesion invasion.15
 Safety
Safety
Office-based procedures on the laryngopharynx and esophagus enjoy an excellent safety record. In 192 invasive procedures on the laryngopharynx performed mostly without intravenous sedation, Bastian and Delsupehe report no episodes of airway compromise, laryngospasm, cardiovascular event, undue bleeding, or unplanned hospitalizations.16 Additional reports with more than 100 procedures on the laryngopharynx, including cancer biopsies, confirm no episodes of undue bleeding, aspiration, or laryngeal trauma. These reports describe a brief, self-limited period of production of blood-tinged secretions after many interventions.9,18 Hogikyan and Pynnonen reported a case of excessive bleeding requiring temporary tracheotomy.15 Tai et al. report a single case of airway compromise after Teflon injection that resolved after 1 week of medical therapy as an inpatient.18
Diagnostic evaluation of the laryngopharynx using flexible endoscopic evaluation of swallowing (FEES) with sensory testing has resulted in mild epistaxis in about 1% of cases.21,22 A careful evaluation of safety by Cohen et al. also records no episodes of airway compromise or laryngospasm and no symptomatic events related to intraprocedural bradycardia or tachycardia.22
Use of the transnasal esophagoscope has been gaining in popularity, and a recent report by Postma et al. suggests an excellent safety record in 611 patients. None had epistaxis requiring packing, and only two had vasovagal episodes that were self-limited.23
One might expect to find an increased incidence of complications when evaluating the airway in the office setting. Reported series, however, do not support this assumption. In 37 transnasal examinations of the airway performed using only topical anesthesia, Hogikyan observed no airway distress or laryngospasm.24 Even in the pediatric population and without specific topical anesthesia applied to the larynx and airway, there were no episodes of airway compromise or laryngospasm in 105 patients as reported by Lindstrom et al.25
 Uses
Uses
Bastian has elegantly reported on the specific use of the flexible endoscope for FEES testing.26 The inclusion of colored dye into food products assists the endoscopic observer in an evaluation of the passage of different food consistencies through the pharynx. Aviv demonstrated the comparable efficacy of this modality in predicting aspiration pneumonia when compared with standard modified barium swallow.27 Bastian et al. have employed FEES for cancer staging within the laryngopharynx.28 Using variable-strength puffs of air to illicit the laryngeal adductor reflex, Aviv et al. have added sensory testing of the laryngopharynx to FEES. This addition allows the otolaryngologist to evaluate laryngeal sensation changes from aging, vocal fold paralysis, stroke, and reflux.29–33
In-office laryngeal tissue manipulations, including the injection of biologically active agents such as cidofovir for papilloma, have been reported.34 Steroids have been successfully delivered into the glottis for treatment of vocal fold nodules, Reinke’s edema, arytenoid granulomas, and contact ulcers.9,15,16,18–20 Favorable results from these in-office procedures argue in support of their efficacy, although injections under general anesthesia have been the historic preference of surgeons for these pathologies. Transoral delivery of Botox for the treatment of spasmodic dysphonia has been championed by Ford and others to enhance precise delivery of the drug thereby reducing the required dosage.35 Additional indications for laryngopharyngeal Botox injection include tremor, refractory muscle tension dysphonia, cricopharyngeal achalasia, and other neurologic disorders.
Injectable glottic bulking agents, once limited to Teflon, are multiple and can be used in the treatment of the diverse pathologies that produce glottic insufficiency.36–40 These newer injectables offer favorable, short- to intermediate-term correction of glottic insufficiency. Patients should be counseled that the improvements in swallowing and voice, though substantial, will be temporary. Fortunately, reinjection is a viable option. Specifically, vocal fold paralysis, paresis, atrophy, scarring, and iatrogenic tissue loss (eg, cancer resection) can all be addressed with office-based glottic augmentation/medialization.
The successful application, in the office setting, of the 585-nm pulsed dye laser, delivered through a flexible endoscope, for treatment of various glottic pathologies has been reported. Use of the laser to vaporize tissue or coagulate vessels allows the reduction of small-volume refractory disease such as recurrent respiratory papillomatosis and dysplasia with keratosis (leukoplakia).41
Given the added safety concerns in the subglottis and trachea, aggressive interventions in these anatomic regions are generally reserved for the more controlled setting of the operating room. Pure visualization of these regions in the office, however, has proven effective and avoids repeated exposure to general anesthesia. Favorable safety records, even in children, argue for office-based airway evaluation in patients not at risk of imminent obstruction or rapidly evolving disease.
The in-office imaging of the esophagus is principally diagnostic in the evaluation of dysphagia, globus pharyngeus sensation, and esophageal reflux disease. In-office esophageal interventions make use of the internal side channel of the transnasal esophagoscope for delivery of small biopsy forceps and grasping instruments. In-office foreign body advancement into the stomach and assistance in the placement of tracheoesophageal prosthesis for postlaryngectomy voice restoration have been reported.23
 Conclusion
Conclusion
Advances in technology improving the resolution of flexible laryngeal imaging have resulted in a renewed interest in office-based laryngology procedures. The introduction of newer injectable bulking agents and flexible laser technology coupled with flexible imaging has already changed the treatment approach for many patients away from the operating room toward well-tolerated, quick, and effective treatments in the office. This trend is likely to continue, and the indications for office-based procedures will likely expand.
 Clinical Examples
Clinical Examples
Case Study 1
A 66-year-old man with a history of smoking was noted to have a suspicious supraglottic mass. Given the patient’s reduced lung capacity and excellent office imaging of the mass, it was biopsied in clinic. For the biopsy, the patient sat in an examination chair opposite the surgeon (Fig. 9.1). After the application of topical anesthetic (atomized 4% lidocaine) to the posterior oral cavity, faucial pillars, and posterior pharyngeal wall, the patient held his own tongue so that the surgeon could use two hands—the left for holding the rigid endoscope (attached to a camera and video monitor) and the right for delivering three separate 1-mL aliquots of 4% lidocaine onto the larynx via an Abraham cannula (curved cannula seen in Fig. 9.2). The right hand was then used to hold the transoral biopsy forceps and biopsy the area in question. This patient reported a 0 of 5 on the FACES pain scale when asked his pain level for the procedure (Fig. 9.3).
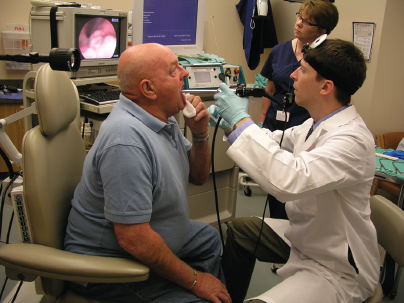
Fig. 9.1 The patient sits opposite the surgeon. The surgeon uses two hands while the patient holds his own tongue. The image on the video monitor is easy for the surgeon to see and allows for magnification and better precision.
Case Study 2
A 25-year-old man with distal tracheal papillomatosis underwent a scheduled Revolix laser (AllMed Systems, Pleasanton, CA) treatment in the office. First, lidocaine/Afrin atomized spray was applied to each nasal cavity, and cottonoid pledgets with the same solution were placed into each nasal cavity (Fig. 9.4). A distal chip endoscope with a working channel was introduced through the more patent nasal cavity and advanced toward the laryngopharynx. Three separate 1-mL aliquots of 4% lidocaine were introduced via a standard syringe at the level of the inferior supraglottis onto the vocal folds while the patient was phonating (Fig. 9.5). At the end of the phonatory gesture, the patient was instructed to breathe in deeply, at which time the lidocaine descended into the trachea allowing for dense tracheal mucosal anesthesia. The patient’s cough reaction all but disappeared after the first application of the lidocaine. The flexible laser fiber was then delivered into the working channel of the endoscope that had been passed easily into the trachea (Fig. 9.6). The papilloma was then treated intralesionally and superficially with the laser to reduce it in size. This patient reported a 1 on the FACES pain scale.
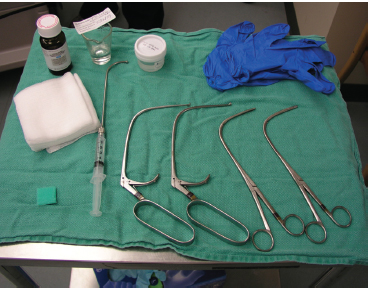
Fig. 9.2 A standard set of equipment for a transoral laryngeal biopsy. Pictured here are four curved biopsy forceps: two short and two long. Also present is the Abraham cannula attached to the plastic syringe; this is used to deliver lidocaine to the supraglottis and glottis.
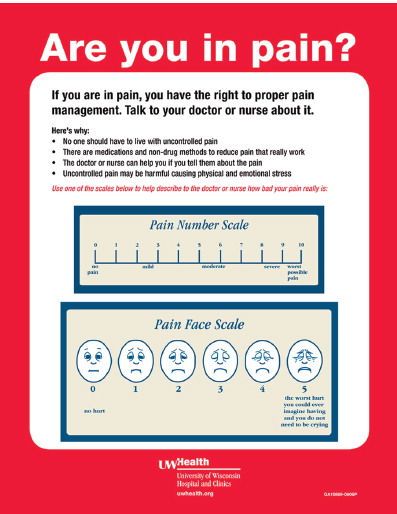
Fig. 9.3 This laminated placard is presented to the patient at the end of each procedure so that their pain scale can be assessed. Often, the patient is also asked where their pain was most intense (eg, the nose) and how to improve the experience if there were to be another procedure.

Fig. 9.4 The patient has had cottonoid pledgets moistened with a 50/50 mixture of 4% lidocaine and oxymetazoline placed into each nasal cavity to minimize discomfort when the flexible endoscope is passed through the more patent side.

Fig. 9.5 One milliliter of 4% lidocaine is introduced into a syringe and the rest of the syringe filled with air. The syringe is then attached to the proximal port of the working channel via a Luer-Lok. When the endoscope is in position, the lidocaine is gently delivered onto the vocal folds as the patient initiates a prolonged phonatory gesture such as a sustained “ee.”

Fig. 9.6 The laser fiber has been introduced into the working channel of the endoscope until its tip exits the distal port of the working channel. The tracheal papilloma can be seen on the video monitor to the patient’s left. Protective eyewear and masks are used during the procedure.
References
1. Karmody CS. The history of laryngology. In: Fried MP, ed. The Larynx: A Multidisciplinary Approach, 2nd ed. St. Louis, MO: Mosby; 1996:3–11
2. Kleinsasser O. Mikrochirurgie im Kehlkopf. Arch Ohren Nasen Kehlkopfheilkd 1964;183:428–433
3. Kleinsasser O. Microlaryngoscopy and Endolaryngeal Microsurgery. Philadelphia, PA: W.B. Saunders; 1968
4. Scalco AN, Shipman WF, Tabb HG. Microscopic suspension laryngoscopy. Ann Otol Rhinol Laryngol 1960;69:1134–1138
5. Howard C, Jako GJ. General anesthesia for direct laryngoscopy and endolaryngeal microsurgery. Eye Ear Nose Throat Mon 1969;48:474–477
6. Thota PN, Zuccaro G Jr, Vargo JJ II, Conwell DL, Dumot JA, Xu M. A randomized prospective trial comparing unsedated esophagoscopy via transnasal and transoral routes using a 4-mm video endoscope with conventional endoscopy with sedation. Endoscopy 2005;37:559–565
7. Preiss C, Charton JP, Schumacher B, Neuhaus H. A randomized trial of unsedated transnasal small-caliber esophagogastroduodenoscopy (EGD) versus peroral small-caliber EGD versus conventional EGD. Endoscopy 2003;35:641–646
8. Ford CN, Roy N, Sandage M, Bless DM. Rigid endoscopy for monitoring indirect vocal fold injection. Laryngoscope 1998;108:1584–1586
9. Omori K, Shinohara K, Tsuji T, Kojima H. Videoendoscopic laryngeal surgery. Ann Otol Rhinol Laryngol 2000;109:149–155
10. Montgomery P, Sharma A, Qayyum A, Mierzwa K. Direct phonoplasty under local anaesthetic. J Laryngol Otol 2005;119:134–137
11. Trask DK, Shellenberger DL, Hoffman HT. Transnasal, endoscopic vocal fold augmentation. Laryngoscope 2005;115:2262–2265
12. Getz AE, Scharf J, Amin MR. Thyrohyoid approach to cidofovir injection: a case study. J Voice 2005;19: 501–503
13. Berke GS, Gerratt B, Kreiman J, Jackson K. Treatment of Parkinson hypophonia with percutaneous collagen augmentation. Laryngoscope 1999;109:1295–1299
14. Ward PH, Hanson DG, Abemayor E. Transcutaneous Teflon injection of the paralyzed vocal cord: a new technique. Laryngoscope 1985;95:644–649
15. Hogikyan ND, Pynnonen M. Indirect laryngeal surgery in the clinical voice laboratory: the renewal of a lost art. Ear Nose Throat J 2000;79:350, 354, 357–358
16. Bastian RW, Delsupehe KG. Indirect larynx and pharynx surgery: a replacement for direct laryngoscopy. Laryngoscope 1996;106:1280–1286
17. Mahieu HF, Dikkers FG. Indirect microlaryngostroboscopic surgery. Arch Otolaryngol Head Neck Surg 1992;118:21–24
18. Tai SK, Chu PY, Chang SY. Transoral laryngeal surgery under flexible laryngovideostroboscopy. J Voice 1998;12:233–238
19. Tateya I, Omori K, Kojima H, Hirano S, Kaneko K, Ito J. Steroid injection to vocal nodules using fiberoptic laryngeal surgery under topical anesthesia. Eur Arch Otorhinolaryngol 2004;261:489–492
20. Tateya I, Omori K, Kojima H, Hirano S, Kaneko K, Ito J. Steroid injection for Reinke’s edema using fiberoptic laryngeal surgery. Acta Otolaryngol 2003;123: 417–420
21. Aviv JE, Murry T, Zschommler A, Cohen M, Gartner C. Flexible endoscopic evaluation of swallowing with sensory testing: patient characteristics and analysis of safety in 1,340 consecutive examinations. Ann Otol Rhinol Laryngol 2005;114:173–176
22. Cohen MA, Setzen M, Perlman PW, Ditkoff M, Mattucci KF, Guss J. The safety of flexible endoscopic evaluation of swallowing with sensory testing in an outpatient otolaryngology setting. Laryngoscope 2003;113:21–24
23. Postma GN, Cohen JT, Belafsky PC, et al. Transnasal esophagoscopy: revisited (over 700 consecutive cases). Laryngoscope 2005;115:321–323
24. Hogikyan ND. Transnasal endoscopic examination of the subglottis and trachea using topical anesthesia in the otolaryngology clinic. Laryngoscope 1999;109(7 Pt 1):1170–1173
25. Lindstrom DR III, Book DT, Conley SF, Flanary VA, Kerschner JE. Office-based lower airway endoscopy in pediatric patients. Arch Otolaryngol Head Neck Surg 2003;129:847–853
26. Bastian RW. The videoendoscopic swallowing study: an alternative and partner to the videofluoroscopic swallowing study. Dysphagia 1993;8:359–367
27. Aviv JE. Prospective, randomized outcome study of endoscopy versus modified barium swallow in patients with dysphagia. Laryngoscope 2000;110:563–574
28. Bastian RW, Collins SL, Kaniff T, Matz GJ. Indirect videolaryngoscopy versus direct endoscopy for larynx and pharynx cancer staging. Toward elimination of preliminary direct laryngoscopy. Ann Otol Rhinol Laryngol 1989;98:693–698
29. Aviv JE, Kim T, Sacco RL, et al. FEESST: a new bedside endoscopic test of the motor and sensory components of swallowing. Ann Otol Rhinol Laryngol 1998;107(5 Pt 1):378–387
30. Aviv JE. Effects of aging on sensitivity of the pharyngeal and supraglottic areas. Am J Med 1997;103:74S–76S
31. Aviv JE, Sacco RL, Mohr JP, et al. Laryngopharyngeal sensory testing with modified barium swallow as predictors of aspiration pneumonia after stroke. Laryngoscope 1997;107:1254–1260
32. Aviv JE, Liu H, Parides M, Kaplan ST, Close LG. Laryngopharyngeal sensory deficits in patients with laryngopharyngeal reflux and dysphagia. Ann Otol Rhinol Laryngol 2000;109:1000–1006
33. Tabaee A, Murry T, Zschommler A, Desloge RB. Flexible endoscopic evaluation of swallowing with sensory testing in patients with unilateral vocal fold immobility: incidence and pathophysiology of aspiration. Laryngoscope 2005;115:565–569
34. Shehab N, Sweet BV, Hogikyan ND. Cidofovir for the treatment of recurrent respiratory papillomatosis: a review of the literature. Pharmacotherapy 2005;25: 977–989
35. Inagi K, Ford CN, Bless DM, Heisey D. Analysis of factors affecting botulinum toxin results in spasmodic dysphonia. J Voice 1996;10:306–313
36. McCulloch TM, Andrews BT, Hoffman HT, Graham SM, Karnell MP, Minnick C. Long-term follow-up of fat injection laryngoplasty for unilateral vocal cord paralysis. Laryngoscope 2002;112(7 Pt 1):1235–1238
37. Rosen CA, Thekdi AA. Vocal fold augmentation with injectable calcium hydroxylapatite: short-term results. J Voice 2004;18:387–391
38. Hertegård S, Hallén L, Laurent C, et al. Cross-linked hyaluronan versus collagen for injection treatment of glottal insufficiency: 2-year follow-up. Acta Otolaryngol 2004;124:1208–1214
39. Courey MS. Homologous collagen substances for vocal fold augmentation. Laryngoscope 2001;111:747–758
40. Chang HP, Chang SY. Autogenous fat intracordal injection as treatment for unilateral vocal palsy. Zhonghua Yi Xue Za Zhi (Taipei) 1996;58:114–120
41. Zeitels SM, Franco RA Jr, Dailey SH, Burns JA, Hillman RE, Anderson RR. Office-based treatment of glottal dysplasia and papillomatosis with the 585-nm pulsed dye laser and local anesthesia. Ann Otol Rhinol Laryngol 2004;113:265–276
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree