Figure 39.1 Illustration of various approaches to the cranial base. The far lateral transcondylar transtubercular approach (dark gray shading) provides a posterolateral trajectory to the craniovertebral junction to access lesions in the inferior clivus and ventral foramen magnum. The midline suboccipital approach (light gray shading), which provides direct access to the posterior foramen magnum, is limited in accessing ventral or ventrolateral lesions of the foramen magnum.
HISTORY
The most common symptoms of a lesion of the lower clivus and upper cervical spine are headache and pain in the neck. If the lower clivus and condyles are involved, as in cases with an extensive chordoma, pain may be associated with movement of the head. Schwannomas of the lower cranial nerves may have symptoms referable to the involved nerve (e.g., weakness of the tongue, hoarseness, or difficulty swallowing). If the lesion is large enough, there may be compression of the cervicomedullary junction, with associated long tract signs such as weakness or numbness, which is usually asymmetric. In such cases, upper motor neuron weakness, with spasticity, gait difficulties, and occasionally sensory loss, may be present.
Obviously, in cases of aneurysmal subarachnoid hemorrhage (SAH), the presentation will involve acute severe headache and impairment of the neurologic sensorium. Severe meningismus will accompany the SAH with neck rigidity. There is nothing specific to the presentation of a ruptured aneurysm of the posterior circulation in most cases, but a local hematoma may produce specific cranial nerve deficits, such as hearing loss or swallowing difficulty.
PHYSICAL EXAMINATION
During a thorough neurologic evaluation, particular attention should be paid to the cranial nerve examination. Even in the absence of symptomatology, subtle cranial nerve deficits may be noted. A diminished gag reflex may be the result of cranial nerve IX and X deficits that may not have reached the magnitude for the patient to note difficulty with swallowing. Long tract signs may manifest as upper motor weakness and spasticity with increased tone and associated reflexes in the affected arm or leg. Similarly, there may be associated sensory deficits of various modalities. Gait evaluation may reveal ataxia with a positive Romberg sign. In addition to the signs and symptoms of SAH, I have also seen presentation of dissecting aneurysms, common in the vertebral artery and PICA, presenting with specific ischemic syndromes, such as the lateral medullary syndrome of Wallenberg.
INDICATIONS
Classic indications for a far lateral approach include pathology anterior to the lower brainstem and upper cervical spine. This includes meningioma (at the foramen magnum or upper anterior spine in location), chordoma of the lower clivus or upper cervical spine, lower cranial nerve schwannoma, or vascular lesion (most commonly aneurysms) involving the vertebral artery or PICA.
CONTRAINDICATIONS
Contraindications for this approach are few, but include congenital anomalies of the upper cervical spine, which might predispose to instability and perhaps an isolated vertebral artery when the contralateral vertebral artery is compromised. This latter condition could increase the chances of devastating posterior circulation ischemia with injury to a sole vertebral artery. Relative contraindications to the approach are paralysis of the contralateral vocal cord or other dysfunction of the lower cranial nerves, which would predispose to a life-threatening bilateral vocal cord paralysis or swallowing difficulties with additional cranial nerve injury on the operated side.
PREOPERATIVE PLANNING
In most instances, magnetic resonance imaging with contrast enhancement is the best imaging study to characterize the nature of the tumor in the upper cervical or clival region. The signal characteristics of specific tumors are characteristic in this location. A meningioma usually will be isointense with the brain on T1-weighted imaging and will avidly enhance with the administration of gadolinium contrast. Chordomas may involve the bone of the clivus or upper cervical spine and are usually erosive. They do enhance with contrast administration, but more specifically are of high signal intensity on T2-weighted imaging, which is a useful tool to differentiate from other tumors such as metastasis. Any involvement or encasement of major vessels, often the vertebral artery or PICA at its origin, should be noted.
In cases of aneurysms, computed tomography (CT) will more accurately demonstrate subarachnoid blood and the predominant location (cervicomedullary cistern or 4th ventricle) may indicate a vertebrobasilar or PICA location. In these cases, a CT angiogram (CTA) study is indicated, which may demonstrate the aneurysm. In some cases, with extensive bone and beam-hardening artifacts in the base of the skull, a conventional digital subtraction angiogram will be necessary to demonstrate the vascular lesion, particularly in cases with dissecting aneurysms.
The rationale for choosing a far lateral approach to the cervicomedullary junction is to provide a more lateral trajectory to the region to avoid or reduce retraction on the brainstem and cerebellum (Fig. 39.1). The region is replete with important cranial nerves and the vertebral and basilar arteries and their branches and perforating vessels. During preoperative planning, imaging is carefully studied, noting the size and location of the tumor and its relationship to the brainstem and vasculature. It is common to encounter tumors in this location that completely encase one vertebral artery in its intradural course. As such, the potential for injury during resection must be considered during planning, and, in such cases, I like to document bilateral vertebral arteries that have a normal course and anastomose at the basilar junction. A common variant is a small vertebral artery on one side that terminally ends in PICA; in such cases, a balloon occlusion test of the involved vertebral artery should be performed, and planning will include repair or revascularization by bypass if the vessel cannot be sacrificed safely.
An important consideration when resecting tumors of this region is the stabilization of the craniocervical junction. I have had several cases in which extensive chordomas and glomus tumors in this location have resulted in bone erosion such that after their removal the craniocervical junction is destabilized by the tumor erosion and additional drilling of the bone. This needs to be anticipated, and I have performed both simultaneous and staged craniocervical stabilization procedures with spine specialists in these cases.
With vascular lesions, especially aneurysms of the vertebral artery or PICA, surgical planning will include any options for endovascular treatment of these lesions. If an open surgical approach is deemed the optimal treatment, planning for treatment will include anticipating options such as vessel sacrifice if tolerated or clip–wrap and bypass techniques.
SURGICAL TECHNIQUE
The location of the tumor, its area of attachment, and involvement of any vascular structures are noted and included in the decision-making process. The extent of drilling of the skull base and condyle is not uniform and is tailored to the particular tumor or vascular lesion. In general, more bone drilling is used for extensive chordomas in this location than for other tumors. The amount of the condyle removed is planned based on the trajectory needed. In most cases of vertebral artery or PICA aneurysms, extensive resection of the condyle or drilling of the jugular tubercle is not necessary.
It has been estimated by some authors that the posteromedial one-third of the occipital condyle may be resected without inducing instability. This issue should be considered on opening, and it should be determined prior to drilling whether bone removal in combination with tumor erosion will result in destabilization of the unilateral condyle region. I have had experience with such cases in which, in addition to the condyle itself, the bone superior to the condyle was involved with tumor such that the condyle was disconnected from the remainder of the skull base, which produced the same destabilizing result.
Far Lateral Transcondylar Approach
The patient is placed in the lateral position with the head in Mayfield three-point fixation (Fig. 39.2), with extensive padding between the legs and in the axilla. The upper arm is supported by an airplane rest and padded accordingly. An important feature of positioning is that the upper arm is directed inferiorly to pull the ipsilateral shoulder as low as possible. This, in combination with lateral flexion of the neck, provides more operative room in the lateral suboccipital–cervical region. A Foley catheter and arterial line are placed prior to positioning.
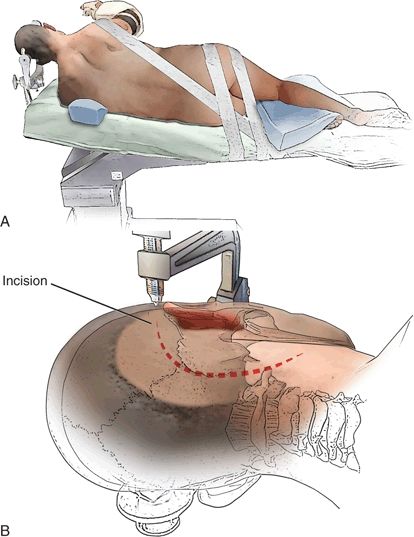
FIGURE 39.2 A> . Diagram showing the patient placed in the lateral position. The head is held in three-point pin fixation with the neck slightly flexed, the vertex angled slightly down, and the face slightly rotated ventrally, so that the ipsilateral external auditory meatus and the mastoid bone are at the highest point. B. Retroauricular curvilinear skin incision (dotted line).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


