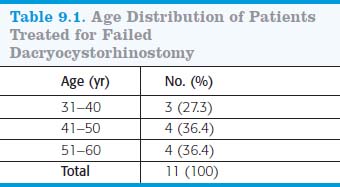
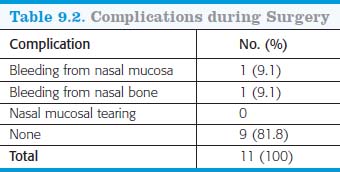
Toti’s technique was modified by other surgeons. External dacryocystorhinostomy is now the most popular operation performed to treat nasolacrimal duct obstruction and the standard by which other treatment methods can be measured and compared. The success rate of external dacryocystorhinostomy (DCR) has been reported between 80% and 99%, depending on the surgeon’s experience. Primary DCR failure is commonly due to scarring at the rhinostomy site. Various other methods to relieve the obstruction of the nasolacrimal duct have been adopted. These include endoscopic DCR, endoscopic laser nasal DCR, dacryocystoplasty, and endoscopic radiofrequency–assisted DCR. Numerous modifications in various surgical steps of the original DCR operation have been introduced over the years for a better surgical outcome, without altering the basic concept. We present a new intervention using the Fugo blade under B-scan guidance in DCR that failed because of fibrous tissue at the osteotomy site. The objective of our study was to determine the success rate of this technique in management of a failed DCR. TECHNIQUE This prospective study was conducted at Sarojini Naidu Medical College, Agra, India, from November 2006 through February 2008. A total of 11 patients who had failed DCRs were recruited—all from the outpatient department. The inclusion criteria were epiphora and a history of a previous DCR surgery. All patients recruited for the surgery were evaluated. Complete ophthalmic examination was performed, including determination of visual acuity, corneal opacities or ulceration, and other ocular comorbidity. Patients were then assessed with a lacrimal sac regurgitation test, syringing, probing, and nasal examination. B-scanning of the sac area was performed to look for possible causes of obstruction. Patients who exhibited fibrous tissue at the osteotomy site as detected on B-scan were included in the study. All patients were also systemically evaluated for diabetes mellitus and hypertension (Figs. 9.1–9.3). None of the patients was subjected to Schirmer’s test, Jones test, or dacryocystography because simple regurgitation, syringing, and probing provided ample proof of the level of blockage in the lacrimal system. Written informed consent was obtained from all patients. Anesthesia All operations were performed under local anesthesia. Nasal packing was done with gauze soaked in 4% Xylocaine (lidocaine) and 1 in 100,000 adrenaline (epinephrine). Proper packing of the nasal cavity helped to anesthetize the mucosa, achieving good hemostasis. The area surrounding the lacrimal sac was infiltrated with 2% lidocaine with 1 in 100,000 epinephrine. About 4 to 5 ml of lidocaine was enough for successful anesthesia of the area. Figure 9.1. The Fugo probe tip inserted though the lower puncta and B-scan probe applied to the sac area. Figure 9.2. B-scan of an anastomotic area (arrow) showing fibrous tissue. Figure 9.3. The Fugo tip introduced into the sac area (long arrow) and cutting fibrous tissue (short arrow). Surgical Technique Postoperative Management The nasal pack was removed postoperatively. Patients were prescribed gatifloxacin (Zymar) eye drops three times daily for 2 weeks and oral ciprofloxacin 500 mg twice daily for 2 weeks and diclofenac 25 mg twice daily for 1 week. Follow-up was done on the first and second postoperative days and 10 days, 1 month, and 6 months after the surgery. Syringing was done on the 10th postoperative day to assess the patency of the lacrimal system. A successful outcome was defined as resolution of symptoms such as epiphora and discharge and a patent lacrimal system on irrigation. Note: Percentages do not add to 100 because of rounding. Summary Eleven patients underwent intervention for failed DCR with this Fugo blade technique. Most patients were between 41 and 60 years of age (72.7%) (Table 9.1). The study participants were predominantly female (72.2%). Women have significantly smaller dimensions in the lower nasolacrimal fossa and middle nasolacrimal duct. Hormonal changes that bring about a generalized de-epithelization in the body may cause the same within the lacrimal sac and duct. An already narrow lacrimal fossa in women predisposes them to obstruction by sloughed off debris. In addition, the injudicious use of cheap or adulterated eye cosmetics applied to the wrong side of the eyelashes can also play important role in obstruction of the nasolacrimal system. All patients were operated on under local anesthesia. Selection of proper anesthesia is vital for the success of a procedure. The advantages of local anesthesia are that it is relatively cheap and safe, and when properly administered it is as effective as general anesthesia. During surgery, some patients experienced bleeding from the nasal mucosa, bleeding from nasal bone, or both. Nasal mucosal tearing was seen in none. Surgery was uneventful in 10 patients (81.8%) (Table 9.2). No complications such as bleeding from the nose, wound infection, or cellulitis were seen in the immediate postoperative period. The overall success rate was 91% after an average follow-up of 6 months. Only 1 patient continued to have troublesome epiphora and required further surgery. The cause of failure in this case was small osteotomy size. Summary Using the Fugo plasma blade to repair a failed DCR had several advantages. Pain and hemorrhaging were minimal, postoperative facial swelling and scarring were absent, and symptoms resolved rapidly after surgery. This is the first study to use the Fugo plasma blade to treat a failed DCR. No incision, no sutures, no pain, no blood, and a nearly 100% success rate are all factors likely to make the Fugo blade the choice of many surgeons in the future to manage cases of failed DCR. Suggested Reading McGrath D. Fugo blade effective tool for multiple surgical applications. Eurotimes. 2008;13(6):43. Singh D. Peep-hole surgery for dacryocystitis. Trop Ophthalmol. 2002;2:11–12.
 bstruction of the nasolacrimal duct results in disrupted outflow of tears, a condition commonly known as “epiphora.” Epiphora remains one of the most bothersome complications of lacrimal system obstruction and has social implications. In 1904, French ophthalmologist Adeo Toti introduced an operation that he called “dacryocystorhinostomy” for the treatment of obstructive epiphora. He proposed that after creating an external approach to the lacrimal sac, its portion near the canaliculi should be preserved and absorbed into the nose by creating a window in the lateral wall of the nose.
bstruction of the nasolacrimal duct results in disrupted outflow of tears, a condition commonly known as “epiphora.” Epiphora remains one of the most bothersome complications of lacrimal system obstruction and has social implications. In 1904, French ophthalmologist Adeo Toti introduced an operation that he called “dacryocystorhinostomy” for the treatment of obstructive epiphora. He proposed that after creating an external approach to the lacrimal sac, its portion near the canaliculi should be preserved and absorbed into the nose by creating a window in the lateral wall of the nose.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree