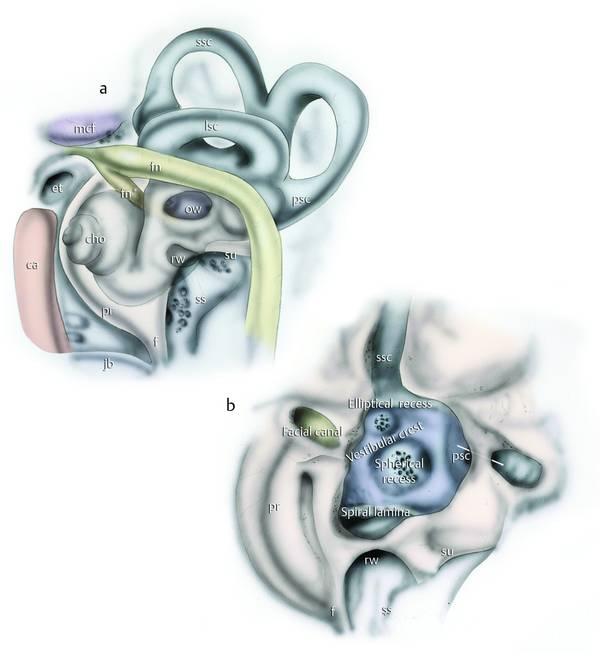
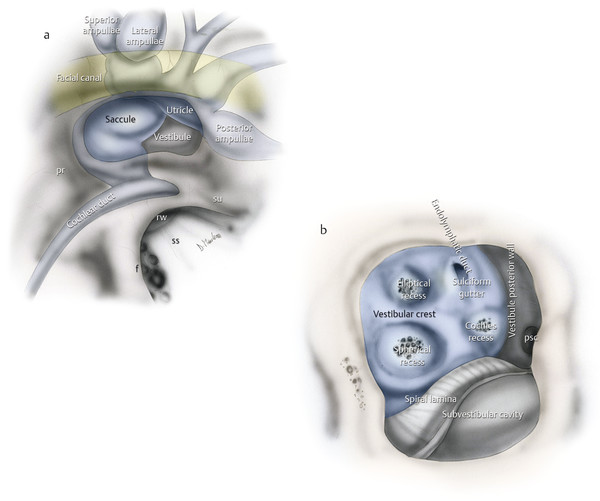
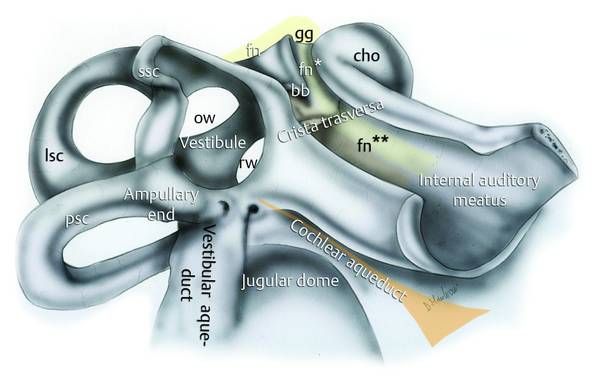
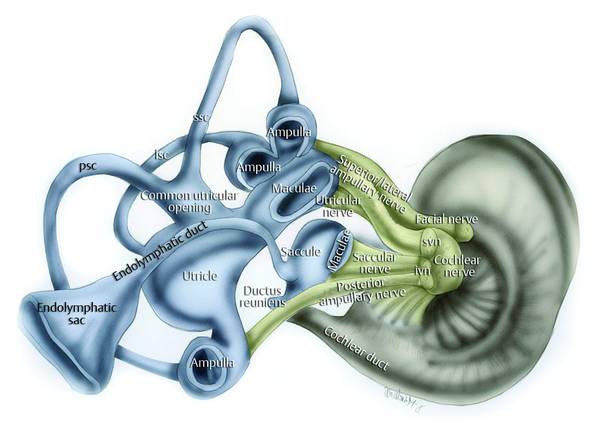
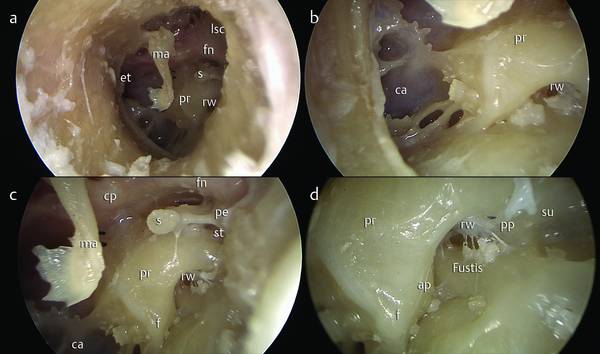
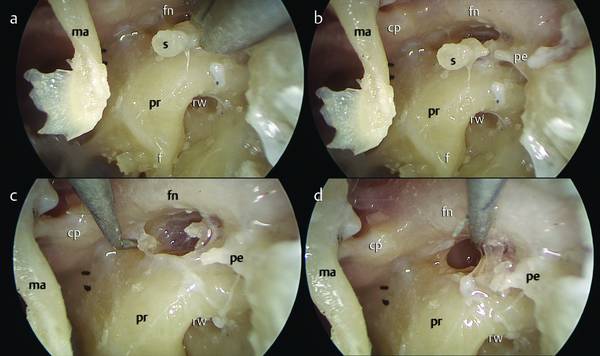
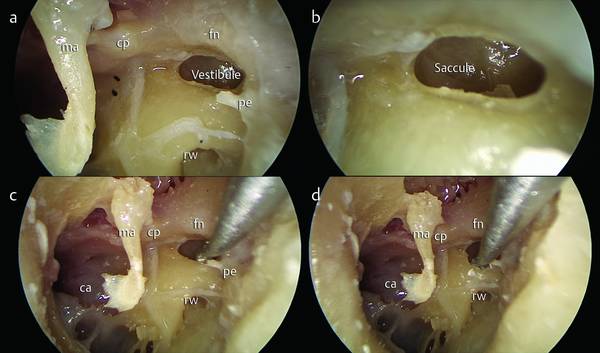
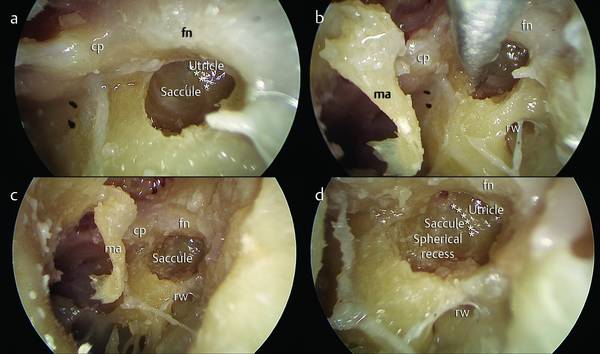
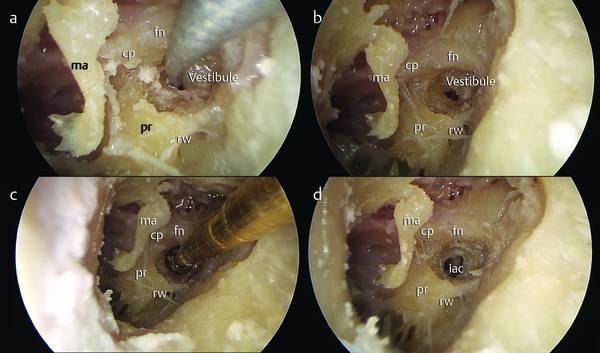
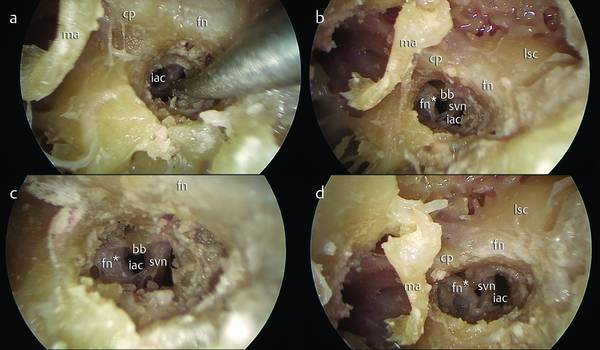
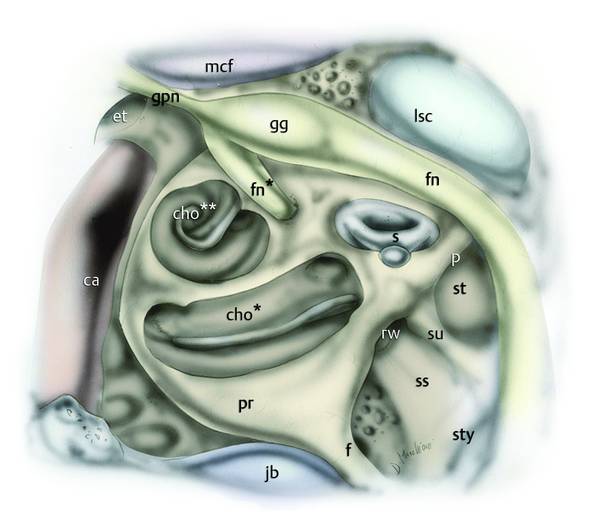
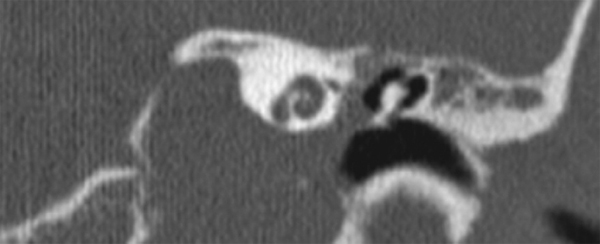
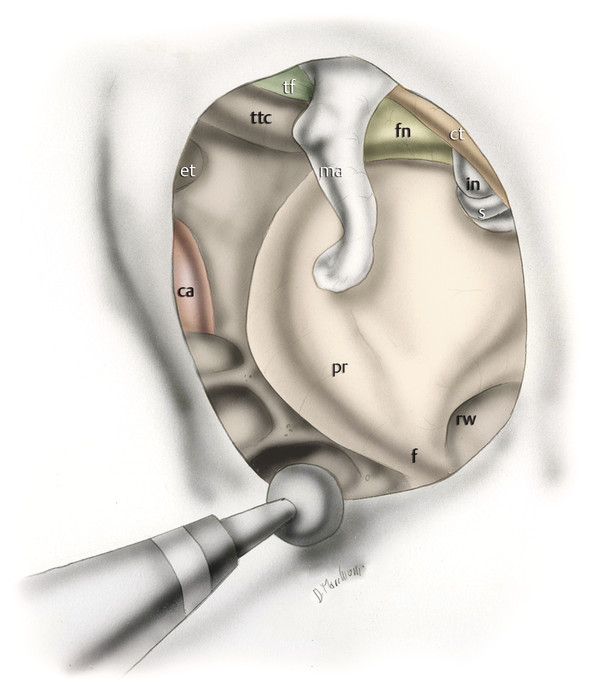
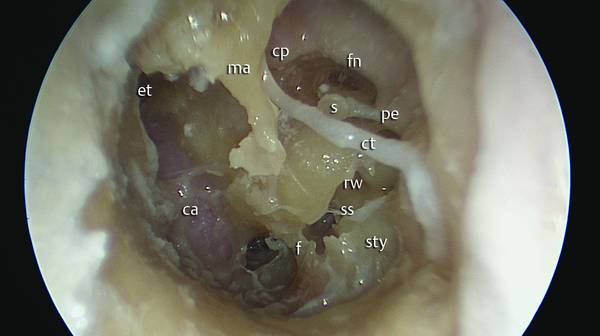
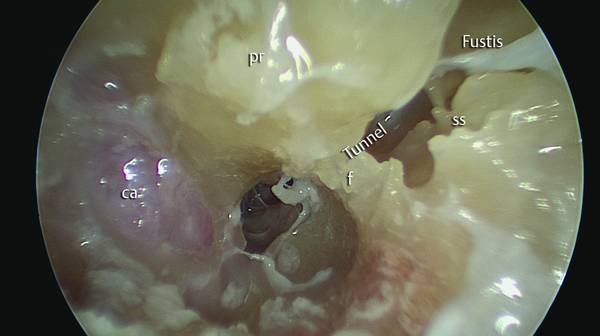
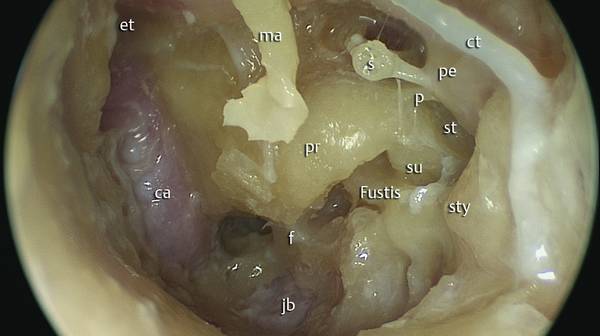
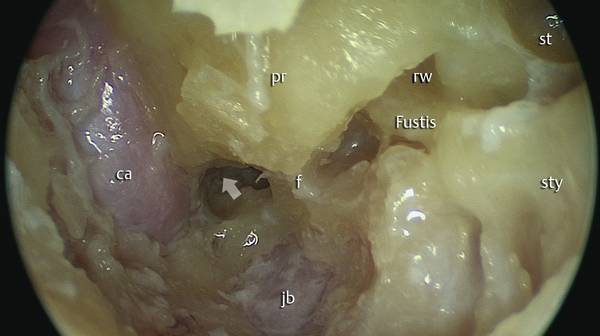
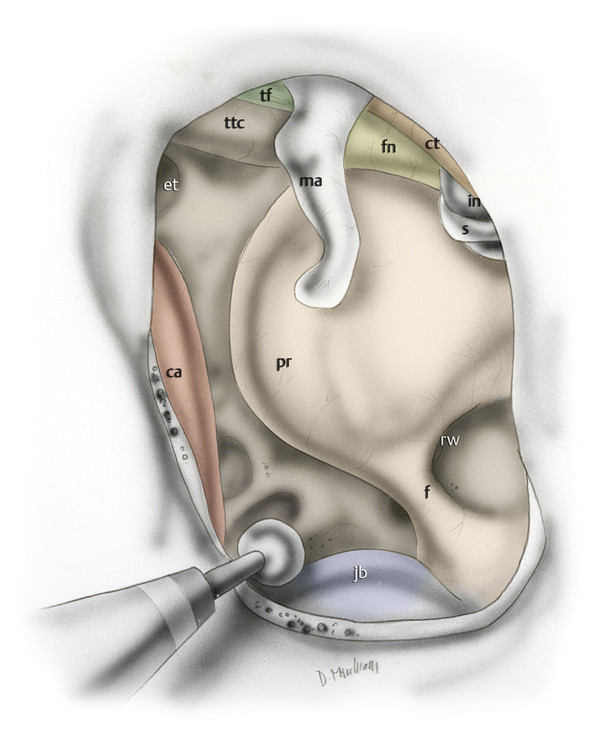
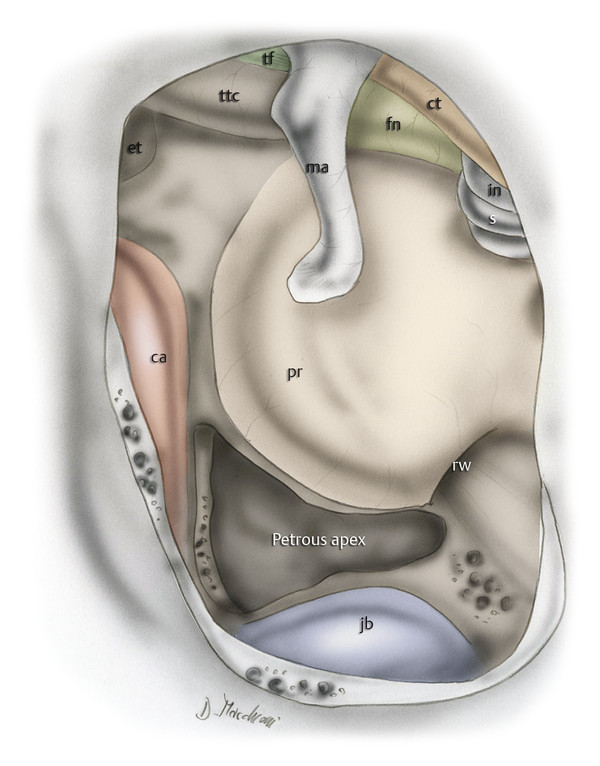
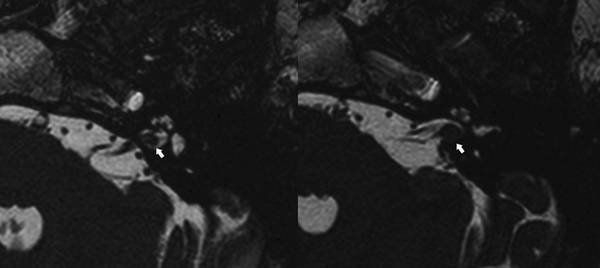
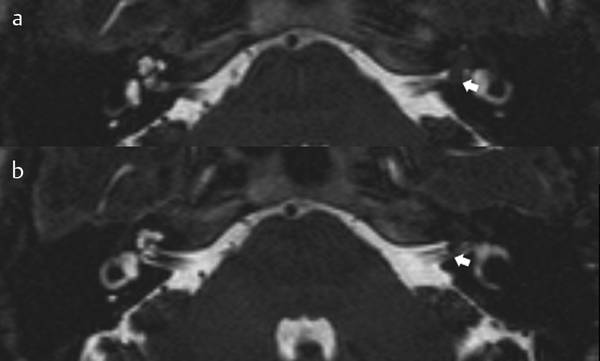
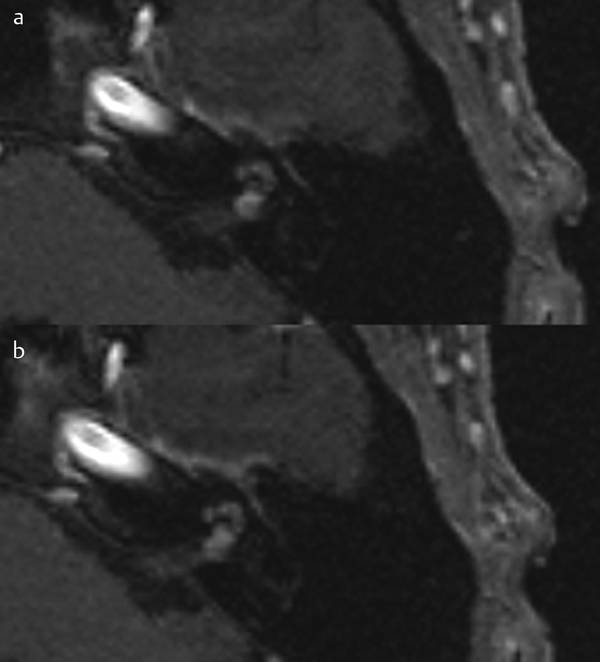
Exclusively Endoscopic Transcanal Approach to the Inner Ear and Petrous Apex From their introduction, exclusively endoscopic approaches to the petrous bone represented new opportunities for treatment of many diseases involving that region,1 with better tissue preservation than achieved with standard microscopic techniques, possibly lower morbidity, and better preservation of vital structures such as facial nerve or otic capsule. Just as in middle ear endoscopic approaches, the pathology is located and attacked directly, limiting the damage or destruction of healthy tissue. Nevertheless, key problems in every kind of approach to petrous bone pathology are represented by preservation of facial nerve function and of hearing. Other anatomical structures that need to be maximally preserved are few in number but are very important: Dura mater of the posterior cranial fossa Dura mater of the middle cranial fossa Labyrinthine tract of the facial nerve Tympanic tract of the facial nerve Vertical tract of the internal carotid artery Horizontal portion of the internal carotid artery Jugular bulb Cochlea Posterior labyrinth. The fundamental prerequisite for this type of surgery is precise knowledge of the anatomy, and in particular the surgical anatomy, under endoscopic vision. The purpose of this chapter is to illustrate the preliminary experiences with exclusively transcanal endoscopic approaches to petrous bone pathology (in particular to the petrous apex and the fundus of the internal auditory canal). The following chapter will focus on combined approaches (endoscopic/microscopic). A further distinction can be made between approaches that allow sparing of the cochlear function and approaches that necessitate destruction of the inner ear with loss of auditory function. Note that none of these approaches requires the rerouting of the facial nerve. We consider two different exclusively transcanal approaches: Exclusively transcanal endoscopic infracochlear approach Exclusively transcanal, transvestibular/transcochlear approach. The vestibule is located between the tympanic cavity laterally and the internal auditory canal medially. Familiarity with the anatomy of the medial wall of the vestibule is fundamental in planning a transcanal approach to the fundus of the internal auditory canal (▶ Fig. 18.1, ▶ Fig. 18.2, ▶ Fig. 18.3). The medial wall of the vestibule presents important anatomical landmarks: Spherical recess Elliptical recess. These two anatomical landmarks are two hollows in the medial vestibular wall separated by a bony ridge called the vestibular crest. This crest circumscribes the spherical recess and exhibits an inferior concavity. Fig. 18.1 a, b Left ear. The most important anatomical structures lying in the medial wall of the tympanic cavity. It is important to note the position of the intralabyrinthine facial nerve in the medial wall of the tympanic cavity; this segment of the facial nerve arises from the geniculate ganglion and runs just above the medial turn of the cochlea, with oblique orientation from laterally to medially, inserting into the fundus of the internal auditory canal, close to the spherical recess of the vestibule. b The oval window has been enlarged, removing the tympanic facial nerve in order to see the entire medial wall of the vestibule. In this way we can note the relationship between the spherical recess and the elliptical recess. The spherical recess is represented by a cribrose plate where the inferior vestibular nerve is inserted; the elliptical recess looks smaller and is represented by a cribrose plate where the superior vestibular nerve is inserted. Enlarging the oval window inferiorly allows one to see the osseous spiral lamina. This structure is the line of separation between the vestibule and the cochlea. On the posterior wall of the vestibule at the level of the spherical recess, a posterior semicircular canal opening is present (white arrow). ssc, superior semicircular canal; lsc, lateral semicircular canal; psc, posterior semicircular canal; mcf, middle cranial fossa; fn, facial nerve; et, eustachian tube; ow, oval window; rw, round window; cho, cochlea ; su, subiculum; ca, carotid artery; pr, promontory; ss, sinus subtympanicus; f, finiculus; jb, jugular bulb. Fig. 18.2 a, b Left ear. View of the oval window after stapes removal. Drawing showing the position of the saccule and the utricle with respect to the oval window. The saccule is occupying the major anterior portion visible through the oval window, from a lateral to medial view. Redrawn from Anson BJ, Donaldson JA, Warpeha RL, Winch TR. Symposium: management of Ménière’s disease. II. Anatomic considerations. Laryngoscope 1965;75(10):1497–1517. Ss: sinus subtympanicus; rw: round window; f: finiculus ; su: subiculum; pr: promontory; psc: posterior semicircular canal. Fig. 18.3 Left ear. Anatomical relationships between the vestibule and the fundus of the internal auditory canal from behind. The inner facial nerve is represented in yellow; the labyrinthine facial nerve is descending from the geniculate ganglion to the fundus of the internal auditory canal; the intracanal facial nerve runs from laterally to medially, from anteriorly to posteriorly. fn, facial nerve; fn*, labyrinthine facial nerve; fn**, intracanal facial nerve; ow, oval window; rw, round window; bb, Bill’s bar; gg, geniculate ganglion; cho, cochlea; psc, posterior semicircular canal; ssc, superior semicircular canal; lsc, lateral semicircular canal. The spherical recess is a microperforated bone area where the inferior vestibular nerve enters (it represents the superior cribriform macula) (▶ Fig. 18.4). After removal of the stapes the most caudal portion of the medial vestibular wall and saccule are visible (see Endoscopic dissection 1 [▶ Fig. 18.5, ▶ Fig. 18.6, ▶ Fig. 18.7, ▶ Fig. 18.8, ▶ Fig. 18.9, ▶ Fig. 18.10]): the spherical recess is located in the anterior portion of the visible vestibule after stapes removal. The spherical recess separates the fundus of the internal auditory canal from the vestibule: it is a particularly fragile bone wall that is easily removable with a curette (see Endoscopic dissection 1 [▶ Fig. 18.9]). Removing the spherical recess causes CSF leakage in the patient because it creates a communication between internal auditory canal and middle ear and also interrupts the inferior vestibular nerve. Fig. 18.4 Left ear. Drawing showing the acoustic-facial nerves from behind into the internal auditory canal. The eighth nerve, upon passing into the internal auditory canal under the facial nerve, is divided into two branches: the cochlear nerve and the vestibular nerve. The cochlear nerve runs into the fundus of the internal auditory canal, attaching to the foraminous tract of the fundus, consisting of the tractus spiralis foraminosus. The vestibular nerve is divided into two branches: the upper branch is divided into the utricular nerve (which attaches on the elliptical recess) and the superior ampullary nerve (for the superior membranous ampulla); the lower branch is divided into the saccular nerve (which attaches on the spherical recess) and the posterior ampullary nerve, which passes into the singular foramen. svn, superior vestibular nerve; ivn, inferior vestibular nerve; ssc, superior semicircular canal; lsc, lateral semicircular canal; psc, posterior semicircular canal. Fig. 18.5 Endoscopic dissection 1. Left ear. Transcanal endoscopic transvestibular approach. a The eardrum and the skin of the external auditory canal have been removed, as have the incus and the head of the malleus. b The carotid artery is detected in the protympanic space. c, d The promontory and the round window niche are recognized endoscopically. fn, facial nerve; pr, promontory; ma, malleus; s, stapes; rw, round window; pp, posterior pillar; ap, anterior pillar; su, subiculum; cp, cochleariform process; st, sinus tympani; et, eustachian tube; pe, pyramidal eminence; lsc, lateral semicircular canal; ca, carotid artery. Fig. 18.6 Endoscopic dissection 1. Left ear. Transcanal endoscopic transvestibular approach. The stapes is removed to provide an endoscopic view of the medial wall of the vestibule. Before (a, b) and after (c, d) stapes removal. fn, facial nerve; s, stapes; ma, malleus; pr, promontory; pe, pyramidal eminence; cp, cochleariform process; rw, round window. Fig. 18.7 Endoscopic dissection 1. Left ear. Transcanal endoscopic transvestibular approach. a, b The medial wall of the vestibule is detected. c, d The inferior lip of the oval window is enlarged with a curette. fn, facial nerve; ma, malleus; cp, cochleariform process; pe, pyramidal eminence, rw, round window; ca, carotid artery. Fig. 18.8 Endoscopic dissection 1. Left ear. Transcanal endoscopic transvestibular approach. a–d Enlarging the anterior lip of the oval window provides direct access to the spherical recess. fn, facial nerve; ma, malleus; cp, cochleariform process; rw, round window; ******, vestibular crest. Fig. 18.9 Endoscopic dissection 1. Left ear. Transcanal endoscopic transvestibular approach. a, b The spherical recess is opened with a curette; this procedure allows entry into the fundus of the internal auditory canal close to the facial nerve. c, d A diamond bur is used to enlarge the communication between the internal auditory canal and the tympanic cavity. fn, facial nerve; ma, malleus; cp, cochleariform process; rw, round window; pr, promontory; iac, internal auditory canal. Fig. 18.10 Endoscopic dissection 1. Left ear. Transcanal endoscopic transvestibular approach. a–d The facial nerve in the internal auditory canal is detected; enlarging the communication between the internal auditory canal and the vestibule inferiorly and anteriorly, we are able to see the cochlear nerve entering into the cochlea. fn, facial nerve; ma, malleus; cp, cochleariform process; iac, internal auditory canal; fn*, intracanal facial nerve; lsc, lateral semicircular canal; bb, Bill’s bar; svn, superior vestibular nerve. The utricular recess is smaller and is located in a posterosuperior position to the spherical recess. It is an oval hollow located on the utricle (▶ Fig. 18.1, ▶ Fig. 18.2). This is a cribrose area adherent to the superior vestibular nerve. Endoscopic viewing of the elliptical recess is difficult due to its anatomical position: it is located cephalad to the plane passing through the tympanic portion of the facial nerve. To access this area with a transcanal endoscopic approach therefore necessitates a rerouting of the tympanic portion of the facial nerve. This cribriform area is very thin and separates the superior portion of the internal auditory canal from the vestibule. Posteriorly to the elliptical recess we can find the sulciform gutter (fossula sulciformis), which is a small cleft located in the most cranial portion of the vestibule’s medial wall, beyond the elliptical recess and beneath the end of the common crus on the superior portion of the vestibule (▶ Fig. 18.2). The sulciform gutter has a slightly oblique route and goes deep cranially, creating a vestibular opening of the vestibular aqueduct. The cochlea is conical in form and located almost horizontally in front of the vestibule (▶ Fig. 18.11); its apex (cupula) is directed forward and lateralward, with a slight inclination downward, toward the upper and front part of the labyrinthic wall of the tympanic cavity; its base corresponds with the bottom of the internal acoustic meatus, and is perforated by numerous apertures for the passage of the cochlear division of the acoustic nerve. It measures about 5 mm from base to apex, and its breadth across the base is about 9 mm. It consists of a conical-shaped central axis, the modiolus; a canal, the inner wall of which is formed by the central axis, wound spirally around it for 2¾ turns, from the base to the apex; and a delicate lamina, the osseous spiral lamina, which projects from the modiolus, and, following the windings of the canal, partially subdivides it into two. A membrane, termed the basilar membrane, stretches from the free border of this lamina to the outer wall of the bony cochlea and completely separates the canal into two passages, which, however, communicate with each other at the apex of the modiolus by a small opening named the helicotrema. Fig. 18.11 Left ear. Transcanal transcochlear/transvestibular approach. Relationship between the cochlear turns, the facial nerve, and the vestibule. Global view of the tympanic cavity after removal of the tensor tympani muscle and after partial removal of the promontory bony wall, exposing the basal, middle, and apical turns of the cochlea. The labyrinthine facial nerve is detected just above the medial and apical turns of the cochlea, descending from the geniculate ganglion to the fundus of the internal auditory canal. fn, facial nerve; lsc, lateral semicircular canal; pr, promontory; gg, geniculate ganglion; rw, round window; ca, carotid artery; s, stapes; gpn, greater petrosal nerve; mcf, middle cranial fossa; et, eustachian tube; jb, jugular bulb; p, ponticulus; st, sinus tympani; su, subiculum; sty, styloid complex; f, finiculus; ss, sinus subtympanicus; cho*, basal turn of the cochlea; cho**, medial and apical turns of the cochlea; fn*, labyrinthine facial nerve. The first 3 to 4 mm of the basal turn of the cochlea is called the subvestibular portion of the cochlea because it is located beneath the vestibule under the oval window. Here it is separated from the vestibule by a cleft whose inner wall is formed by the last quarter of the first turn of the cochlea; this is the vestibulocochlear cleft. The next portion of the basal coil is carried anteriorly by the helicoid form of the cochlea. It closely approximates the floor of the fundus of the internal auditory canal. The base of the cochlea is in intimate relation with the low portion of the fundus of the internal auditory canal via the tractus spiralis foraminosus. The tractus spiralis foraminosus is an opening in the cochlear area of the bottom of the internal acoustic meatus through which the fibers of the cochlear nerve leave the bony labyrinth to enter the internal auditory canal. This area is very thin and is easily removed, thus allowing the opening of the internal auditory canal in its more caudal portion and exposure of cochlear nerve. Cholesterol granuloma of the temporal bone, located inferiorly to the cochlea, with preoperative preserved hearing function (▶ Fig. 18.12) Cholesteatoma infiltrating the tunnel under the finiculus bone, reaching the petrous apex Cholesteatoma with sinus subtympanicus infiltration, and extension inferior to the cochlea (i.e., tunnel). Fig. 18.12 CT, coronal view, showing a cholesterol granuloma involving the petrous apex in a patient with normal function and aspect of the cochlea. In this case a transcanal infracochlear approach would be proposed. In the initial steps a 0°, 15-cm, 3-mm optic is used. Circular incision of the skin of the external auditory canal with a round knife or a Vesalius device with angled tip. Removal of the external ear canal skin with the tympanic membrane, as a glove finger. Detachment of the tympanic membrane from the handle of the malleus, whose integrity is maintained. Circumferential calibration of the bony external ear canal (see ▶ 17.3.2 in Chapter ▶ 17). The drilling is then extended to the inferior bony anulus so as to obtain a good view of the hypotympanic region with 0° optic—jugular bulb identification and skeletonization (▶ Fig. 18.13; see also Endoscopic dissection 2 [▶ Fig. 18.14, ▶ Fig. 18.15, ▶ Fig. 18.16, ▶ Fig. 18.17]). Identification of the vertical tract of the carotid artery in the case of an anterior extension of the pathology (▶ Fig. 18.18 and Endoscopic dissection 2 [▶ Fig. 18.15, ▶ Fig. 18.16]). Drilling with a diamond bur of the medial aspect of the tympanic cavity between jugular bulb and basal turn of the cochlea, represented by the caudal portion of the promontory, until the pathology is reached (▶ Fig. 18.19). Draining of the pathology in the case of granuloma. Further possible widening of the approach can be required in the case of cholesteatoma, to completely clear the matrix of the pathology. At this point the cavity can be explored with 45° optics to detect any residual disease and remove it with angled instruments. The ear canal skin and tympanic membrane are repositioned at the end of the operation. Fig. 18.13 Left ear. Endoscopic transcanal infracochlear approach. After the eardrum and skin of the external auditory canal are removed, a diamond bur is used to enlarge the external auditory canal by drilling the bony wall. fn, facial nerve; ct, chorda tympani; ma, malleus; pr, promontory; rw, round window; f, finiculus; ca, carotid artery; et, eustachian tube; in, incus; s, stapes; ttc, tensor tympani canal; tf, tensor fold. Fig. 18.14 Endoscopic dissection 2. Left ear. Endoscopic transcanal infracochlear approach. Dissection specimen. Infracochlear approach. The external auditory canal was enlarged and the carotid artery was identified. The finiculus is used as landmark to establish the position of the jugular bulb. fn, facial nerve; ct, chorda tympani; ma, malleus; rw, round window; f, finiculus; ca, carotid artery; et, eustachian tube; s, stapes; pe, pyramidal eminence; ss, sinus subtympanicus; sty, styloid complex. Fig. 18.15 Endoscopic dissection 2. Left ear. Endoscopic transcanal infracochlear approach. Dissection specimen. Magnification of the hypotympanum. The finiculus indicates the position of the jugular bulb. The tunnel is visible under the finiculus and the anterior pillar. The vertical portion of the carotid artery is the anterior limit of the dissection. pr, promontory; f, finiculus; ss, subtympanic sinus; ca, carotid artery. Fig. 18.16 Endoscopic dissection 2. Left ear. Endoscopic transcanal infracochlear approach. Dissection specimen. The bony wall of the hypotympanum close to the finiculus is removed to expose the jugular bulb. ct, chorda tympani; ma, malleus; f, finiculus; ca, carotid artery; et, eustachian tube; s, stapes; pe, pyramidal eminence; sty, styloid complex; p, ponticulus; st, sinus tympani; su, subiculum; jb, jugular bulb. Fig. 18.17 Endoscopic dissection 2. Left ear. Endoscopic transcanal infracochlear approach. Dissection specimen. The bone between the carotid artery, the jugular bulb, and the promontory is gently removed in order to reach the petrous apex (white arrow) under the cochlea. ca, carotid artery; jb, jugular bulb; f, finiculus; pr, promontory; rw, round window; st, sinus tympani; sty, styloid complex. Fig. 18.18 Left ear. Endoscopic transcanal infracochlear approach. The drill is used to reveal the anatomical position of the internal carotid artery and the jugular bulb. fn, facial nerve; ct, chorda tympani; ma, malleus; pr, promontory; rw, round window; f, finiculus; ca, carotid artery; et, eustachian tube; in, incus; s, stapes; ttc, tensor tympani canal; tf, tensor fold; jb, jugular bulb. Fig. 18.19 Left ear. Endoscopic transcanal infracochlear approach, The bone of the medial wall of the tympanic cavity, between the carotid artery anteriorly, the jugular bulb posteriorly, and the promontory superiorly, is removed in order to reach the petrous apex while preserving cochlear function. fn, facial nerve; ct, chorda tympani; ma, malleus; pr, promontory; rw, round window; ca, carotid artery; et, eustachian tube; in, incus; s, stapes; ttc, tensor tympani canal; tf, tensor fold; jb, jugular bulb. In some cases in which the jugular bulb is particularly high in the hypotympanum, the use of a 0° endoscope enables immediate identification the area of the bulb in relationship to the caudal end of the finiculus—in the majority of cases some millimeters anterior to this area (▶ Fig. 18.15, ▶ Fig. 18.16). A diamond bur may help to further skeletonize the jugular bulb, which will become an important landmark. In some other cases, in contrast, the jugular bulb is located particularly inferiorly, and an accurate and deep drilling of the hypotympanic cells at the level of the finiculus and the tunnel will be necessary to correctly identify the structure. A tunnel positioned under the cochlea leads toward the vertical tract of the internal carotid artery. The endoscopic approach is indicated for pathologies of the petrous apex and the fundus of the internal auditory canal (IAC) with exclusively infracochlear, infravestibular, and paracarotid extension. Indication is limited to pathologies without mastoid involvement: Mesotympanic cholesteatoma extending medially to the inner ear (infracochlear and/or vestibular extension and/or anterior extension to the carotid region) Cholesterinic granuloma of the petrous apex with anterior extension Small symptomatic acoustic neuroma with exclusive involvement of the fundus of the IAC not responding to conservative treatment (▶ Fig. 18.20) Cochlear schwannoma with or without extension to the IAC (▶ Fig. 18.21, ▶ Fig. 18.22). At present few patients undergo this endoscopic approach and it is certainly an experimental approach, but preliminary results are interesting and they open new perspectives in endoscopic ear surgery even in hidden areas that are otherwise difficult to reach without invasive approaches. Fig. 18.20 a, b MRI, axial view, showing a small schwannoma (arrow) located in the fundus of the internal auditory canal. Fig. 18.21 a, b MRI, axial view. MRI shows a cochlear schwannoma (arrow) involving the cochlea and spreading into the fundus of the internal auditory canal (white arrow). Fig. 18.22 a, b MRI, axial view. MRI shows hyperintense signal of an intracochlear neoplasm involving the fundus of the internal auditory canal. Cholesterol granulomas with loss of auditory function Facial nerve neuroma (geniculate ganglion of the tympanic tract of the nerve with loss of auditory function) Small neuromas of the fundus of the IAC with vertigo and loss of auditory function Intralabyrinthine or cochlear schwannomas with vertiginous symptomatology associated with sensorineural hearing loss with or without extension into the fundus of the IAC. A high-resolution CT scan is always necessary to study the bone details of this area and the relationships between the fundus of the internal auditory canal, the vestibule, and the cochlea. MRI is important in studying the relationships between pathology and nervous structures (e.g., the facial nerve). MRI is always necessary in an endoscopic approach to the internal auditory canal to study the route of the anterior inferior cerebellar artery and labyrinthine artery. An endoscopic approach might be dangerous in the presence of a loop of the anterior inferior cerebellar artery into the IAC. An endoscopic approach is contraindicated in this rare situation. Transcanal endoscopic circumferential incision of the skin 3 mm from the anulus. Using a 0° endoscope, the skin of the external auditory canal and the eardrum are totally dissected and removed. The external auditory canal is drilled circumferentially until a good exposure is achieved. This is a simple but fundamental step because it allows the introduction of surgical instruments and the use of a 4-mm endoscope. Nonetheless, a second surgeon may help the first operator with suction. Next, identification of large vessels in the tympanic cavity has to be made before proceeding: the jugular bulb in the hypotympanum and the vertical tract of the carotid artery (▶ Fig. 18.23). The ossicular chain is then removed: removal of the incus and malleus after sectioning of the tendon at the cochleariform process exposes the second portion of the facial nerve to the geniculate ganglion and the greater petrosal nerve (GPN) anteriorly (▶ Fig. 18.24
18.1 Introduction
18.1.1 Anatomical Concepts1–4
18.2 Exclusively Transcanal Endoscopic Infracochlear Approach5–7
18.2.1 Indications
18.2.2 Surgical Steps
Key Points
18.3 Exclusively Transcanal Endoscopic Transvestibular/Transcochlear Approach 8–10
18.3.1 Indications
18.3.2 Preoperative Examinations
18.3.3 Surgical Steps
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


