Chapter 7 Examination, history and special tests in pediatric ophthalmology
Assent and consent
Our ethical responsibilities as caregivers of children are essential. The omniscient doctor used to make all the decisions; now, with patient advocacy and participatory decisions, we have to share more of our responsibility for the good of our young patients and their families. The children also have a right to the truth.1 In consent, we try to define the limits of our young patients’ autonomy: what decisions can a child make on the information we provide? When can they evaluate risks, consequences, and benefits? Should we obtain a child’s assent, without coercion, to proceed with an unpleasant examination or treatment in the face of unequivocal parental consent? More on these issues in Chapter 58.
It is all about the child
Personality, timing, and the planned investigations all have their influence on the patient’s cooperation (Table 7.1). A crying infant will not yield useful information on its visual potential, but calming feeding – breast or bottle – can lead to a few moments of conclusive observation of a visual response. A worried 3-year-old with juvenile idiopathic arthritis might not volunteer for a slit-lamp examination, but given the chance to first talk about a cherished new pair of sneakers, or be shown how to do it by a sibling, may eagerly allow a good view of cells and flare. A shy teenager with papilledema might open up as soon as Mom leaves the room. Mostly, it is all in the act – how you do it!
Table 7.1 The 19 chronologic steps of a pediatric ophthalmology consultation – a progressive level of “intrusiveness” maximizes the cooperation and yield
| 1 | Observe before formal encounter – waiting room, on the way to the examinig room |
| 2 | Say “Hi” to child |
| 3 | Observe while greeting – body language (body & head), postures, visual behavior |
| 4 | Child in the chair alone, on parent’s lap, or in parent’s arms |
| 5 | History – parent, child, family photo album |
| 6 | Brückner’s |
| 7 | None dissociating binocularity tests – two-pencil test (2PT), Lang, Frisby. Head posture |
| 8 | VA* – binocular, better eye, worse eye |
| 9 | Dynamic retinoscopy |
| 10 | Extraocular muscles (EOM) – the frame |
| ** | __________________________________________________ |
| 11 | Pupils, corneal diameter, lids – fixation target, ruler with photo |
| 12 | Refined binocularity tests – progressive dissociation |
| 13 | Confrontation fields |
| 14 | Strabismus assessment |
| 15 | Drops |
| 16 | Intraocular pressure (IOP) |
| 17 | Refraction |
| 18 | Fundus |
| 19 | Reward |
* VA Monocular visual acuity (VA) testing might influence the results of binocularity assessment due to dissociation.
** This line denotes the point from which the examination requires equipment and manipulations near the child’s eyes. From here on, the child’s cooperation becomes a key issue.
The equipment
A successful examination room needs toys to satisfy children: small near fixation targets (silent, so not to test hearing) with a few able to transmit an internal light, an audible distant fixating target able to attract attention, and, finally, rewards to give. How many visual targets? “One toy, one gaze, one look” is a good rule (Fig. 7.2). In addition to the usual ophthalmic equipment, a portable slit-lamp and tonometer and appropriate vision charts complete the set. Other special equipment for infant vision, examination of premature newborns, full orthoptic assessment, and electrodiagnostic and imaging investigations are useful in specific circumstances.
History: include the children
Taking a history is crucial. The clues augment elusive clinical signs in a non-cooperative child. Time and opportunism, however, are of the essence. Loquacious parents with genetic disease, a room full of siblings and friends, etc., all distract from the task at hand. While it is tempting to get most of the history from the parents, the child’s perspective can be revealing. A parent might provide a very different account of a poorly compliant amblyopic child who has had a great summer at the grandparents’ without having to wear that patch! Important details become known only when we gain the confidence of our young patients. Examples include being bullied about wearing spectacles, or emergency room stories about pellet guns changed when only the mother is present. Poor family dynamics, “blame games,” avoidance, and miscommunications, socioeconomic and cultural issues can all be barriers. The mother is the usual key to a successful outcome. Her understanding, cooperation, and engagement in the care process are essential.2 Finally, pictures can play a big part of the historical record. A few family good photographs can give enough clues to target the examination for a diagnosis of Duane’s retraction syndrome, or Brown’s syndrome. Retinoblastoma is sometimes detected by images of a white pupil in family photographs.
A no-touch approach at first
With children, simple observation should be the first priority. Simply watch, with a “hands off” approach before intervening. Start with the least intrusive tests. Specialized ancillary tests are usually done after the initial clinical assessment, based on specific diagnostic requirements (Chapters 8 and 9).
Observe
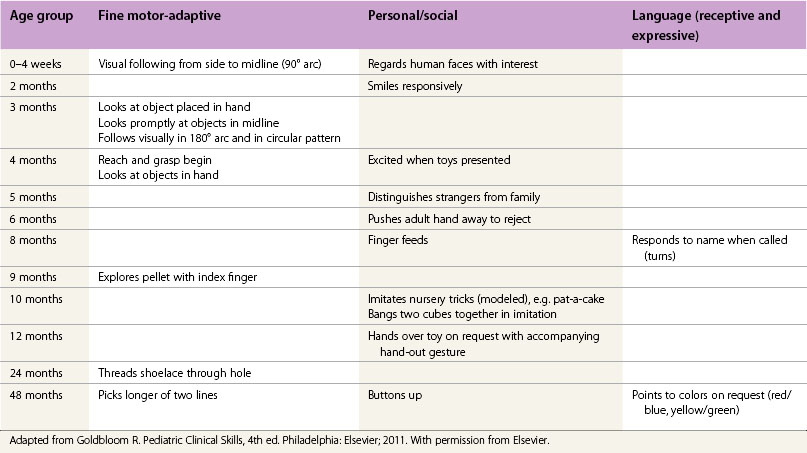
While greeting, observe the head position (incomitant strabismus, nystagmus, or a field defect), evidence of photophobia (corneal disease, retinal dystrophies, glaucoma), body language as evidence of a visual handicap or behavioral peculiarities (extreme hyperactivity, inattention, withdrawal, or violence of the abused child), and the possible clues of developmental delay, especially associated with abnormal visual functions (Table 7.2).
Where to sit for the examination
Many young children will be comfortable, quieter, and more cooperative on their parent’s lap. A few want to start the visit in their parent’s arms away from the usual diagnostic area with its strange machines. Infants can be assessed quite satisfactorily in this manner. Flexibility is essential (Fig. 7.1)!
Parents as a resource
Do not have too many in the room which may be a source of distraction and noise. The best scenario is to have just the child in the office with a cooperative parent or two. A good friend in the same age group can be calming for a 6- to 10-year-old. Someone might have to hold a non-cooperative child. In decubitus, a preferred position for drop instillation, or sitting and facing the examiner, the parents quickly learn how effective they can be to help and comfort their child (Fig. 7.3).
Get Clinical Tree app for offline access