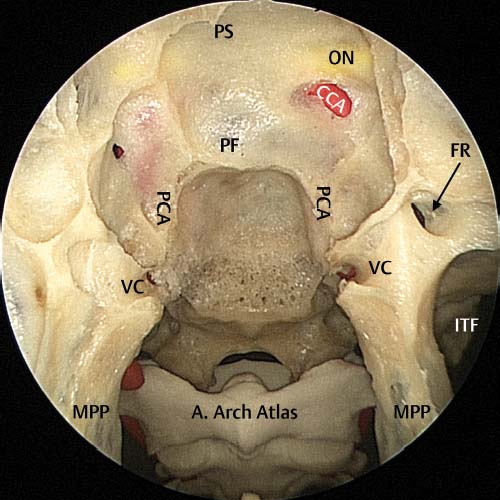
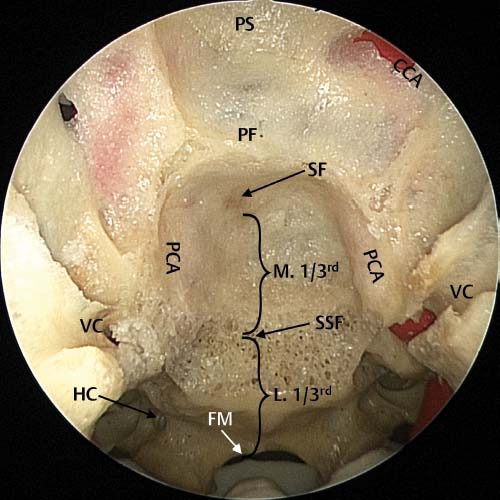
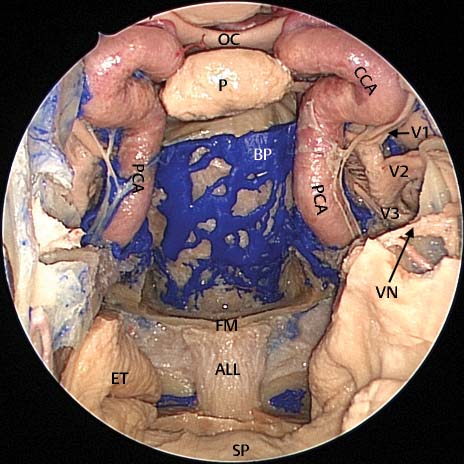
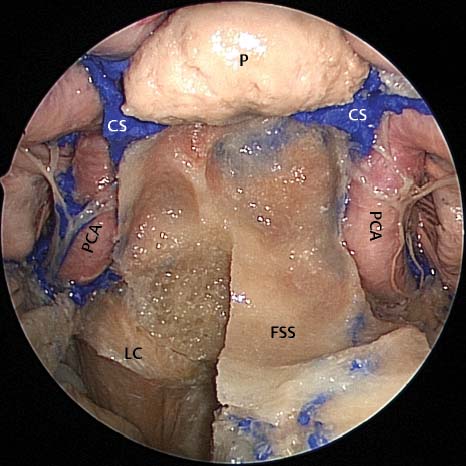
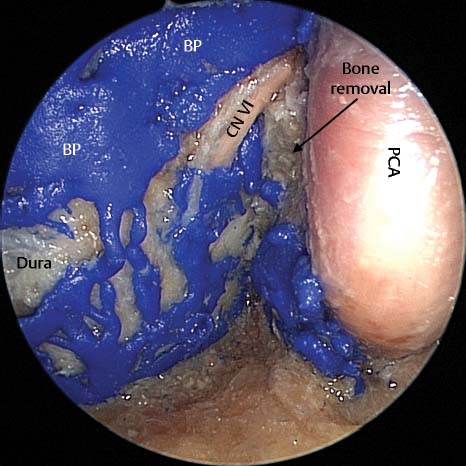
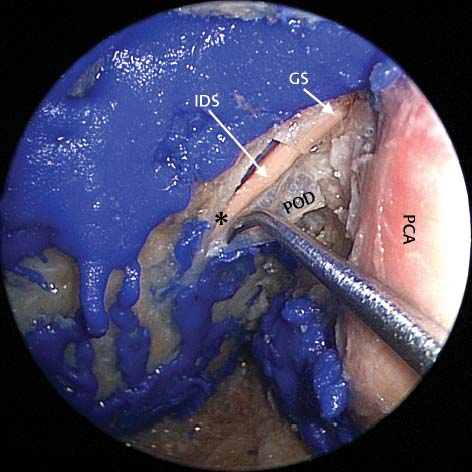
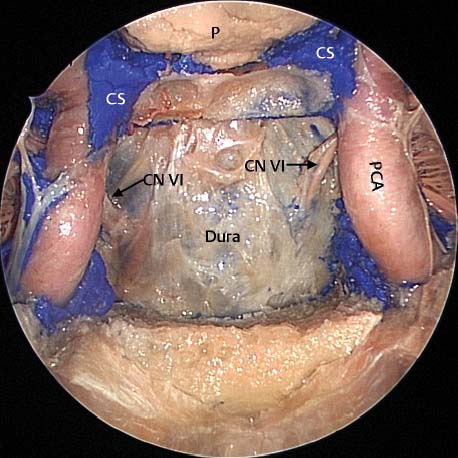
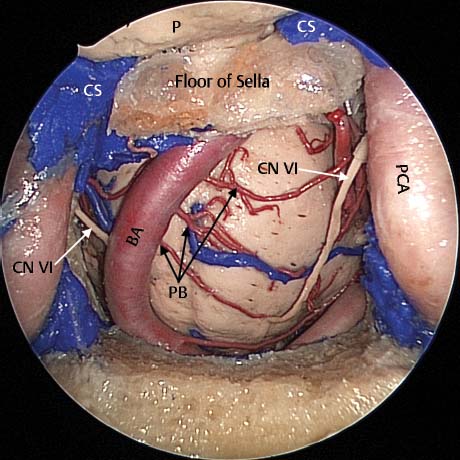
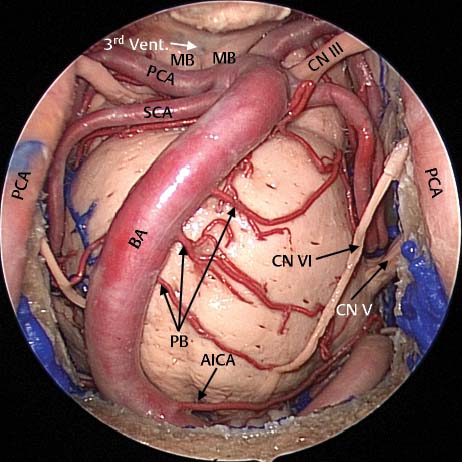
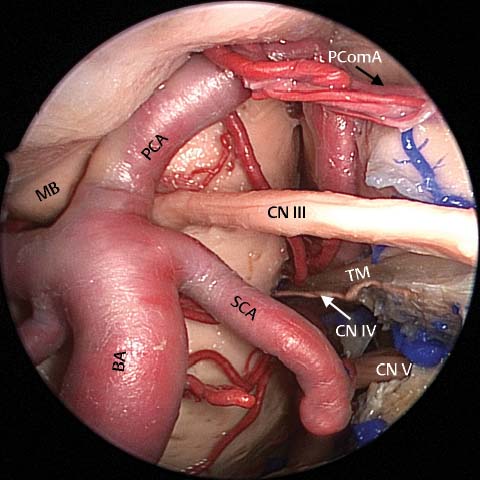
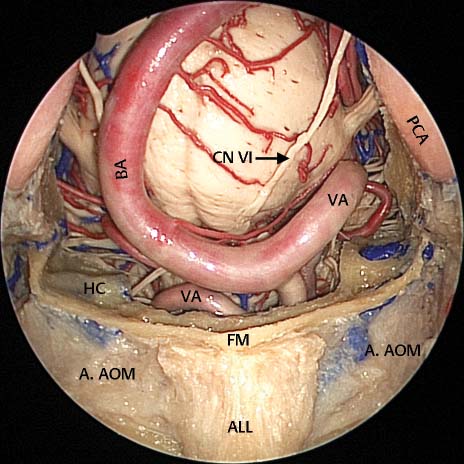
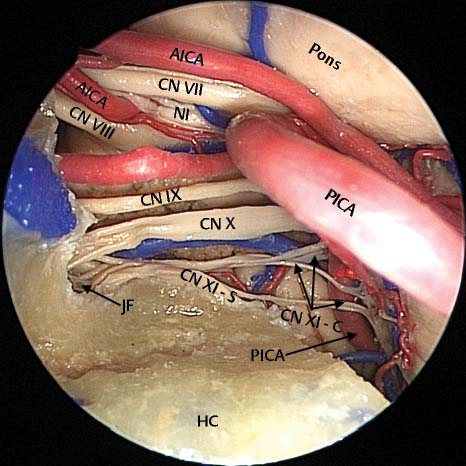
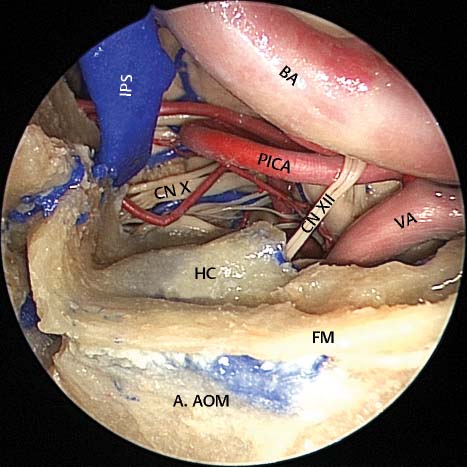
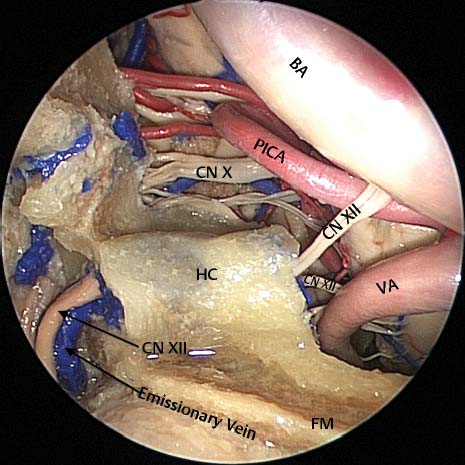
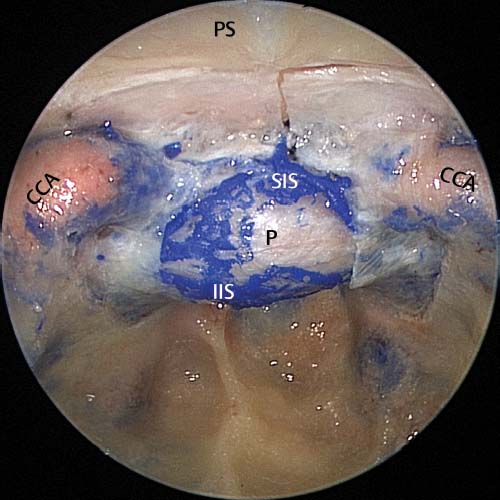
19 Tumors of the clivus and posterior cranial fossa are very difficult to access via traditional neurosurgical approaches. In the past skull base teams would approach the petroclival region either by a lateral or anterior route. The lateral route was via an extended middle cranial fossa approach1 whereas the anterior route could be transmaxillary, transoral, or trancervical.2,3 All of these approaches involve significant resection of normal structures with inevitable associated morbidity.1–4 Even after such a resection the final surgical access was usually limited. The operating microscope did not allow a view around the corner and, if the tumor extended beyond the exposed area, resection under direct vision was not possible. The advantages of the endoscopic transsphenoidal approach is that it allows access to the entire clivus down to the atlas of the cervical spine. It also allows early identification of the vital vascular structures with clear visualization of both carotid arteries and the cavernous sinuses and associated neurologic structures.4 The most common tumor presenting in the clival region is a chordoma. Although complete resection of the tumor and the surrounding bone is optimal, this is often not possible due to the location and surrounding vital structures.2,5 It is accepted that as complete a resection as is possible should be performed.5 In most cases clival chordomas are slow growing and if surgery can be combined with radiotherapy (especially proton beam radiotherapy), this gives the patient the best possible chance of prolonged survival.2,5 Because curative surgery is often not possible, the morbidity associated with tumor debulking should be as limited as possible. These factors make an endoscopic approach to these tumors attractive as it provides the best possible chance of complete surgical removal with the least surgical morbidity.4,5 To remove the clival tumor and any associated intracranial extension, a clear understanding of the anatomy of this region is essential. The clivus extends from the dorsum sella to the foramen magnum (Figs. 19.1 and 19.2). The thickness of the clivus depends on the pneumatization of the sphenoid and can vary significantly. When this bone is thick it may hold significant venous channels (Fig. 19.3). This makes removal of the bone a slow process as significant bleeding can occur as the cancellous bone is opened. This is generally quickly controlled by packing the area with Gelfoam paste (Pharmacia and Upjohn Company, Kalamazoo, MI). Further drilling will provoke more bleeding which requires repacking and this process can make bone removal tedious. However, there is no quick and easy solution to the control of the bleeding in this area. The lateral borders of the dissection of the clivus are the paraclival carotid arteries and these need to be exposed at the beginning of the dissection to avoid inadvertent damage (Fig. 19.4). The inferior limit of the dissection is usually the floor of the sphenoid but should access be required to the basiocciput, foramen magnum, or even lower to the first cervical vertebra, the entire sphenoid floor can be removed (Fig. 19.4). Complete removal of the clivus exposes the dura of the posterior fossa. Bone behind the inferior portion of the paraclival carotid arteries can be removed so that the arteries stand proud of the lateral margins (Fig. 19.5). The limit to which this bone can be removed is determined by the 45- degree angle that the carotid arteries make as they run in their canals through the petrous temporal bone. This region where the petrous portion of the carotid artery turns vertically in the floor of the sphenoid is where bone should be removed to access the petrous apex. In some patients a large cholesterol granuloma may thin down the bone separating the granuloma from the sphenoid allowing the granuloma to be drained through the sphenoid. Fig. 19.1 Dry skull dissection with the floor of the sphenoid sinus drilled away revealing the middle and lower thirds of the clivus. The vidian canals (VC) can be seen bilaterally at the level of the floor of the sphenoid sinus. PS, planum sphenoidale; PF, pituitary fossa; ON, optic nerve; CCA, anterior genu of the intracavernous carotid artery; FR, foramen rotundum; PCA, paraclival carotid artery; MPP, medial pterygoid plate; FR, foramen rotundum; A. Arch Atlas, anterior arch of atlas; ITF, infratemporal fossa. Fig. 19.2 Dry bone specimen demonstrating the middle and lower thirds of the clivus. The middle third (M. 1/3rd) begins at the sella floor (SF) and extends to the floor of the sphenoid sinus (SSF), and the lower third (L. 1/3rd) extends from the floor of the sphenoid sinus to the foramen magnum (FM). The upper third corresponds to the dorsum sella, and visualization is obstructed by the pituitary gland. A pituitary transposition allows visualization of the upper third of the clivus. VC, vidian canal; HC, hypoglossal canal; PCA, paraclival carotid artery; PF, pituitary fossa; PS, planum sphenoidale; CCA, anterior genu of the intracavernous carotid artery. Fig. 19.3 Cadaveric dissection demonstrating the large venous channels within the clivus that constitute the basilar plexus (BP) that can cause significant bleeding during surgery. OC, optic chiasm; P, pituitary gland; CCA, anterior genu of the intracavernous carotid artery; PCA, paraclival carotid artery; VN, vidian nerve; FM, foramen magnum; ET, Eustachian tube; ALL, anterior longitudinal ligament; SP, soft palate; V1, ophthalmic division of the trigeminal nerve; V2, maxillary division of the trigeminal nerve; V3, mandibular division of the trigeminal nerve. Fig. 19.4 Cadaveric dissection demonstrating the identification of the paraclival carotid arteries (PCA), the lateral borders of the dissection. If dissection is to continue to the lower clivus then the entire floor of the sphenoid sinus can be removed. The longus capitis muscle (LC) attaches firmly to the floor of the sphenoid sinus (FSS). CS, cavernous sinus; P, pituitary gland. Fig. 19.5 Cadaveric dissection image taken with a 30-degree endoscope. Bone has been removed behind the paraclival carotid artery (PCA) so that the arteries stand proud of the lateral margins. BP, basilar plexus; PCA, paraclival carotid arteries; CN VI, abducens nerve; *, gulfar segment of the abducens nerve. Fig. 19.6 Cadaveric dissection of the left middle clivus (taken with a 30-degree endoscope) demonstrating the different segments of the abducens nerve. The abducens nerve moves through the posterior cranial fossa (cisternal segment) before perforating through the meningeal layer of dura (marked by *). Then the nerve enters a channel between the meningeal layer of dura and the periosteal layer of dura (POD). This segment is called the interdural segment (IDS). In this dissection a “leaf” of periosteal dura has been incised and reflexed to clearly visualize the abducens nerve running within. The nerve then enters the confluence of dural sinus, made up of the superior and inferior petrosal sinuses, the basilar plexus, and the cavernous sinus. Here it is called the gulfar segment (GS). PCA, paraclival carotid artery. The dura has two layers: a periosteal layer and a meningeal layer. The extensive and rich venous plexus—the basilar plexus—runs between the periosteal and meningeal layers of the dura. Exposure of the clival periosteum can result in significant bleeding. In a patient with a recurrent meningioma previously removed through external approach, bleeding of 3 L was encountered. One of the ways to seal off these venous sinuses is to open the dura and bipolar the two layers together. This was done but it was felt that the patient had lost too much blood to proceed and surgery was stopped and rescheduled for 2 weeks later. At this operation there was minimal bleeding and the tumor was successfully addressed. Before the dura is opened the surgeon needs to have a clear understanding of where the sixth nerve is likely to be. As seen in Chapter 18, the sixth nerve enters Dorello’s canal (canal formed by the periosteal and dural layers about midway up the middle third of the clivus just below the posterior meningeal artery) and then progresses to the gulfar region behind the carotid artery (Figs. 19.5 and 19.6). The gulfar region is formed by the junction of the inferior and superior petrosal sinus, basilar plexus, and posterior region of the cavernous sinus. All of these sinuses are between the periosteal and meningeal layers of dura. A general landmark for this region is the junction of the floor of the pituitary with the vertical paraclival section of the carotid. Once the dura of the posterior cranial fossa has been opened, the contents of the posterior cranial fossa can be seen (Figs. 19.7 and 19.8). The first and most notable structure seen is the basilar artery which is usually covered with arachnoid (Fig. 19.8). Figs. 19.9, 19.10, 19.11, 19.12, 19.13, and 19.14 demonstrate the structures that are easily visualized. In most patients the segments of the brainstem that can be easily visualized are the upper part of the medulla, the pons, and the lower edge of the midbrain. The vessels that are seen are the basilar, posterior cerebral, superior cerebellar, and anterior inferior cerebellar arteries. Depending on the state of the brain, a variable number of the cranial nerves can be seen. Dehydration of the brain by the administration of mannitol may enlarge the space around the brainstem and allow easier visualization of the nerves. Fig. 19.7 Cadaveric dissection of the middle third of the clivus with removal of the basilar plexus and exposing the dura. The abducens nerves (CN VI) can be seen bilaterally as they perforate the meningeal dura and become the interdural segments of CN VI. CS, cavernous sinus; PCA, paraclival carotid arteries; P, pituitary gland. Fig. 19.8 Cadaveric dissection following removal of the middle third of the clivus and dura. The basilar artery (BA) can be seen very tortuous. Its pontine branches (PB) can be clearly seen. CN VI, abducens nerve; CS, cavernous sinus; P, pituitary gland; PCA, paraclival carotid artery. Fig. 19.9 Cadaveric dissection with removal of the upper third and middle third of the clivus with visualization of the posterior cerebral arteries (PCA), superior cerebellar arteries (SCA), and the occulomotor nerve in between (CNIII). 3rd Vent, third ventricle; MB, mamillary bodies; PCA, posterior cerebral arteries; SCA, superior cerebellar arteries; CN III, occulomotor nerve; PCA, paraclival arteries; BA, basilar artery; PB, pontine branches; CN VI, abducens nerve, CN V, trigeminal nerve; AICA, anterior inferior cerebellar artery. Fig. 19.10 Cadaveric dissection image taken with a 30-degree endoscope following removal of the superior third of the clivus, visualizing the small trochlear nerve seen running along the tentorial membrane edge. BA, basilar artery; PCA, posterior cerebral artery; SCA, superior cerebellar artery; CN III, occulomotor nerve; CN IV, trochlear nerve; CN V, trigeminal nerve; TM, tentorial membrane; PComA, posterior communicating artery; MB, mamillary body. Fig. 19.11 Cadaveric dissection image demonstrating structures seen following dissection of the lower third of the clivus. Note how the basilar arteries and vertebral arteries can be extremely tortuous in their course. ALL, anterior longitudinal ligament; A. AOM, anterior atlantooccipital membrane; FM, foramen magnum; HC, hypoglossal canal; VA, vertebral arteries; BA, basilar artery; CN VI, abducens nerve; PCA, paraclival carotid artery. Fig. 19.12 Cadaveric dissection with image taken just above the skeletonized hypoglossal canal (HC) at the cerebellopontine angle. The anterior inferior cerebellar artery (AICA) can be seen intimately associated with the vestibulocochlear nerve (CN VIII), facial nerve (CN VII), and the nervus intermedius (NI). The posterior inferior cerebellar artery (PICA) can be seen running between the vagus (CN X) and spinal and cranial portions of the accessory nerves (CN XI – S, CN XI – C). Fig. 19.13 Cadaveric dissection image taken following dissection of the right lower third of the clivus. As the posterior inferior cerebellar artery (PICA) courses from the vertebral artery (VA) it frequently runs through the rootlets that make up the hypoglossal nerve (CN XII). It may tent these rootlets as it courses to the cerebellomedullary fissure to run intimately with the cranial nerves IX – XI. CN X, vagus nerve; HC, hypoglossal canal; IPS, inferior petrosal sinus; BA, basilar artery; FM, foramen magnum; A. AOM, anterior atlanto-occipital membrane. Fig. 19.14 Cadaveric dissection image showing the hypoglossal nerve exiting the hypoglossal foramen with its corresponding vein that communicates the internal jugular vein with the basilar plexus. HC, hypoglossal canal; CN XII, hypoglossal nerve and rootlets; FM, foramen magnum; VA, vertebral artery; PICA, posterior inferior cerebellar artery; BA, basilar artery; CN X, vagus nerve. Tumors extending behind the pituitary gland are usually unresectable unless the upper third of the clivus is removed. To do this the pituitary gland must either be translocated anteriorly or, in patients who are hypopit with a nonfunctional gland, removed. Before the gland can be translocated, space needs to be created for the gland to be positioned in the planum sphenoidale. The first step is to remove all the bone over the pituitary fossa onto the carotid arteries. The next step is to remove the bone overlying the tuberculum sella and over the posterior half of the planum sphenoidale (Fig. 19.15). This bone is removed from optic nerve to optic nerve and wider on the planum sphenoidale. The dura is incised and the subchiasmatic cistern inspected (Fig. 19.16). The diaphragm of the pituitary should be visualized and divided with skull base scissors up to the pituitary stalk (Fig. 19.17). Next, to translocate the gland, the periosteum and dura layers over the anterior aspect of the gland need to be separately identified and the plane between these layers clearly established. As the gland is mobilized the dentate ligaments that hold the pituitary gland in place are identified and divided (Fig. 19.18). The inferior hypophysial artery will need to be divided to allow mobilization of the gland (Figs. 19.19 and 19.20). Dissection needs to proceed carefully (Fig. 19.21), otherwise the thin layer covering the cavernous sinus can be easily penetrated resulting in substantial venous bleeding. This can be controlled by Gelfoam paste and pressure with a neuropattie but this should be avoided if possible. Once the gland is fully mobile it can be translocated into the region of the planum sphenoidale (Fig. 19.22). The upper third of the clivus is now visible and can be removed (Fig. 19.23). A inverted Y-shaped osteotomy is made with the stem in the midline. A 1- to 2-mm high speed stylus diamond burr (Medtronic ENT, Jacksonville, FL) is used to perform these osteotomies (Fig. 19.24). Once the posterior clinoids are fully mobile a combination of a blunt hook and dissector is used to gently peal the clinoids out of their periosteal layer. Remember that the posterior clinoid abuts both the intracranial carotid artery and the posterior genu of the intracavernous carotid artery simultaneously, and is at risk during this maneuver (Figs. 19.23 and 19.24). Now the dura can be opened and the suprasellar anatomy fully visualized. The first structure encountered is the Liliequist membrane, which is a condensation of arachnoid that attaches to the posterior clinoids and third nerves and has a semicircular aperture through which the basilar artery can pass (Fig. 19.25). Fig. 19.15 Cadaveric dissection of the sphenoid sinus demonstrating the removal of bone over the anterior genu of the intracavernous carotid arteries, sella, tuberculum sella, and the posterior half of the planum sphenoidale (PS). CCA, anterior genu of the intracavernous carotid artery; IIS, inferior intercavernous sinus; SIS, superior intercavernous sinus; P, pituitary gland.
Endoscopic Resection of Clival and
Posterior Cranial Fossa Tumors
 Anatomy
Anatomy
The Clivus
Posterior Cranial Fossa
Pituitary Translocation for Access to the Upper Third of the Clivus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree