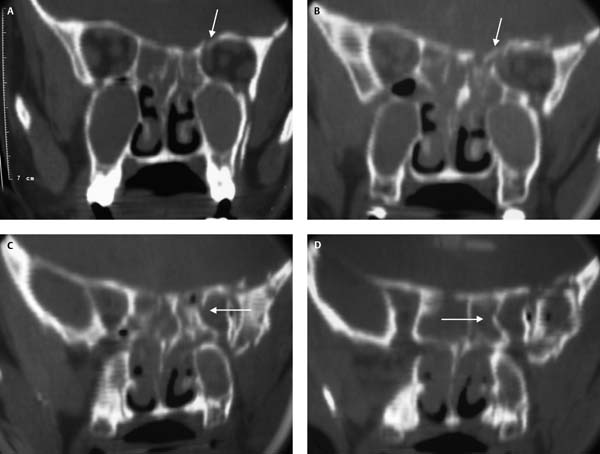
15 The most common indication for endoscopic optic nerve decompression is traumatic optic neuropathy.1 Currently it is thought that ~5% of severe head injuries will have a concomitant injury to the optic nerve, optic tract, or optic cortex.1–3 However, if the literature is reviewed, there are only a limited number of patients who have undergone this procedure.4 Major brain injury occurs in 40 to 72% of patients with traumatic optic neuropathy5 and the management of this injury obviously takes precedence. This may result in the optic nerve injury only being diagnosed some time after the original injury. Some authors feel that early diagnosis and treatment of traumatic optic neuropathy may be of greater benefit to the patient6,7 and advocate diagnosis of the optic nerve deficit by the presence of an absolute or relative afferent pupillary defect supported by disc edema and congestion of the vessels.6 These findings, in combination with the computed tomography (CT) scan, possibly a magnetic resonance imaging (MRI) scan and visual evoked potentials, may provide sufficient evidence to undertake optic nerve decompression.6,7 However, the patient management protocol suggested in this chapter is more conservative as there is still considerable debate as to the value of both high-dose steroid treatment and surgical optic nerve decompression.3–5,7 Currently there are no properly conducted randomized controlled trials comparing high-dose steroid therapy, surgical decompression, and observation.8 In a meta-analysis of all published cases in the literature, Cook et al. concluded that treatment in the form of high-dose steroids or surgery or both was better than no treatment.4 Tandon et al. evaluated the role of steroids with and without surgery in a large study of 111 patients who were placed in two groups: one group of patients had high-dose steroids and if they failed to improve underwent an optic nerve decompression whereas the second group had steroids alone.1 This study showed that the patient group treated with steroids and surgery had significantly better outcome than the patient group treated with steroids alone.1 Sofferman, in a study on an animal model of traumatic optic neuropathy, showed that injury to the optic nerve results in a progressive loss of myelin but with preservation of axons so that in theory the progression of the injury may be reversed with steroid or surgical decompression.7 Traumatic optic neuropathy is thought to result from two distinct injuries to the nerve. The primary injury results from either a direct contusive force on the optic canal and nerve or as a result of elastic deformation of the sphenoid with a transfer of force into the intracanalicular optic nerve disrupting the axons and blood vessels.5 This primary injury may result in compression of the nerve by bony fragments or in hemorrhage into the nerve sheath. If this injury is not treated a secondary injury may occur. As the nerve swells in its dural sheath and bony canal, compression of the blood supply to the nerve occurs with resultant ischemia and continued axon loss.5,7 Our department has adopted a conservative approach to traumatic neuropathy with all patients undergoing high-dose steroid treatment first before being offered surgical intervention. The exception is when bony fragments are seen to impinge on the optic nerve. Currently, mega-dose intravenous methylprednisolone is used following the spinal cord injury management protocol. Methylprednisolone 30 mg/kg intravenous (IV) loading dose is given followed by an infusion of 5.4 mg/kg/hour thereafter.4 The patient’s visual acuity is monitored hourly and surgical intervention is considered if the patient fills any of the criteria listed below: The standard preparation of the nose is performed with decongestion and infiltration. An uncinectomy with exposure of the maxillary ostium is performed. An axillary flap is performed and the agger nasi cell removed. This improves access to the skull base. The fovea ethmoidalis is exposed in the region above the bulla ethmoidalis. If there is disruption of the cells of the frontal recess or reason to suggest that the frontal recess is obstructed then this will be cleared; otherwise, the cells in the frontal recess are left untouched. In some patients with severe sinus fractures, the entire skull base may be mobile. In the patient presented in Fig. 15.1, the entire posterior skull base was mobile. In most patients the posterior ethmoid cells will be full of blood and, when this is combined with mobility of the lamina papyracea and skull base, the surgeon can become disorientated. Therefore this surgery should only be undertaken by very experienced endoscopic sinus surgeons. A posterior ethmoidectomy and sphenoidotomy should be performed as described in Chapter 8. In the posterior ethmoids, the posterior lamina papyracea and fovea ethmoidalis should be identified (Fig. 15.2). If significant disruption of the posterior ethmoids and lamina papyracea has occurred, then a large middle meatal antrostomy provides an extra reference point and lessens the likelihood of surgeon disorientation (Fig. 15.2). The natural ostium of the sphenoid sinus should be identified and the anterior face of the sphenoid widely opened. It is important for the surgeon to be fully aware of the anatomy of the lateral wall of the sphenoid (Fig. 15.3). If available the computer-aided surgery (CAS) navigation system may help in patients where there has been significant anatomical disruption. The anterior face of the sphenoid needs to be taken as high as possible so that the roof of the sphenoid and the posterior ethmoids is continuous.3,9,10 The sphenoid should be inspected and the optic nerve, carotid artery, and pituitary fossa identified.9,10 If there has been significant disruption of the orbital apex or the lateral wall of the sphenoid, then identification of these basic structures can be difficult (Fig. 15.4). In these cases image guidance may help. Fig. 15.1 (A–D) Sequential coronal CT scans from (A) the posterior ethmoids to (D) the sphenoid sinus. The white arrows indicate fractures and note the blood in the ethmoids and sphenoids. (B) In addition, the white arrow indicates the loose segment of skull base. The scans are of relative poor quality due to patient movement from confusion from an associated head injury.
Endoscopic Optic Nerve
Decompression
 Medical Therapy for Traumatic Optic Nerve Injury
Medical Therapy for Traumatic Optic Nerve Injury
 Fracture of optic canal on CT scan with vision less than 6/60
Fracture of optic canal on CT scan with vision less than 6/60
 Fracture of the optic canal with vision > 6/60 but the patient’s vision deteriorates on steroids
Fracture of the optic canal with vision > 6/60 but the patient’s vision deteriorates on steroids
 Vision is < 6/60 (or there is a deterioration of vision) after 48 hours of steroid treatment with probable canal injury (indicated by the presence of fluid levels in the posterior ethmoids and sphenoid and/or the presence of fractures of the ethmoids, orbital apex, and sphenoid)
Vision is < 6/60 (or there is a deterioration of vision) after 48 hours of steroid treatment with probable canal injury (indicated by the presence of fluid levels in the posterior ethmoids and sphenoid and/or the presence of fractures of the ethmoids, orbital apex, and sphenoid)
 Surgical Technique for Traumatic Optic Neuropathy (Video 49)
Surgical Technique for Traumatic Optic Neuropathy (Video 49)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree