Surgical Anatomy
The size and shape of the external auditory canal (EAC) vary among individuals. The canal is approximately 35 mm long and 5 to 10 mm in diameter. It has a sigmoid shape and runs from behind and above downward and forward. It can be divided into two parts: the fibrocartilaginous part forms the outer one-third of the canal, while the bony part forms the inner two-thirds. An anterior bulging may be evident in the most medial part of the bony canal: this is due to the protrusion of the temporomandibular joint, which has close relationships with the anterior wall of the EAC, and can prevent adequate exposure of the anterior anulus during surgical procedures (particularly by microscope). The EAC is completely covered by skin.
The tympanic membrane, representing the fundus of the EAC, is shaped like a very shallow cone pointing medially and is made up of three layers: (1) skin, (2) collagen fibers, and (3) the mucosa of the middle ear. (▶ Fig. 15.1).
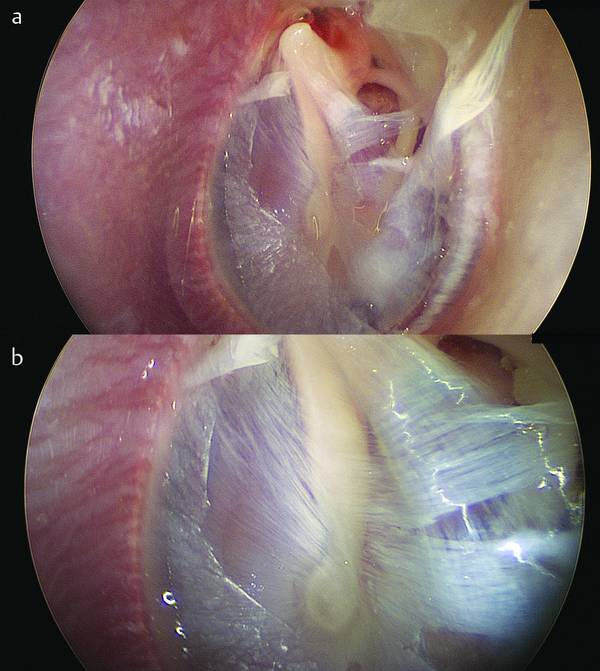
Fig. 15.1 a, b Left ear. Endoscopic view of the tympanic membrane after removal of the cutaneous layer. The organization of the fibrous middle layer is visible. a The eardrum after partial removal of the skin layer, exposing the organization of the fibrous layer. b An endoscopic magnification of the fibrous layers.
15.2 Surgical Concepts
Although in general microscopic myringoplasty is considered a safe operation, 1,2 the endoscopic technique is probably even safer due to the absence of an external incision, which minimizes the risk of postoperative wound infection or hematoma formation. The absence of bone drilling for widening purposes obviates the risk of postoperative EAC stenosis or anomalous healing processes. The direct visualization of the entire medial aspect of the middle ear (including the facial nerve) adds support to that concept.3 The advantages and disadvantages of this technique need to be considered in the surgical indication.
15.2.1 Advantages of Endoscopic Myringoplasty
In a tortuous EAC, with an endoscopic approach it is only rarely necessary to widen the canal.
Direct visualization of the entire eardrum.
Direct visualization of the tympanic cavity and related structures such as the ossicular chain, the chorda tympani, the seventh cranial nerve, and the round and oval windows.
Clear visualization of the anterior anulus and anterior limit of the eardrum perforation.
Endoscopic evaluation of the middle ear ventilation routes during surgery.
Absence of wide external incisions and dissection of periauricular tissues.
15.2.2 Disadvantages of Endoscopic Myringoplasty
The technique is more difficult than the traditional one, especially in the hands of inexperienced surgeons.
One-handed technique.
It is impossible to employ an overlay technique in relation to the fibrous layer of the tympanic membrane. Accordingly, although dissection of the skin layer from the underlying fibrous layer of the eardrum is possible, it is extremely complex and we do not recommend it.
15.3 Indications and Contraindications
The indications for the endoscopic technique are no different from those applicable to the traditional technique. Patient selection needs to consider some issues relating to the middle ear state to be treated.
The patient’s age It is not recommended to perform an endoscopic myringoplasty for a patient under the age of 6 years (unless the patient needs a hearing aid or cochlear implant) for two reasons. The first is that below this age the immaturity of the rhinotympanic tube would affect the surgical results (and repair of the tympanic membrane below this age is considered only in the presence of recurrent otorrhea, which might damage the integrity of the ossicular chain when that is intact). The second reason is anatomical: In some cases, the limited dimensions of the EAC in children younger than 6 years may make the endoscopic transcanal approach difficult to accomplish. However ear canal orientation should also be taken into consideration, and the straight orientation of the external auditory canal at this age could be helpful in making the surgical endoscopic procedures easier.
Middle ear and perforation appearance Dry perforations without problems in the tympanic cavity, and/or marginal perforations involving the anulus (and therefore at risk of skin migration from the external auditory canal to the middle ear, with possible formation of a secondary cholesteatoma) must of course be treated and are the best indications for this technique (▶ Fig. 15.2). Unstable perforations, associated with recurrent otorrhea with or without the appearance of granulation in the tympanic cavity and/or nasopharyngeal problems, should be treated pharmacologically before surgery, since the percentage of failures in the inflammatory phases is considerable (▶ Fig. 15.3, ▶ Fig. 15.4).
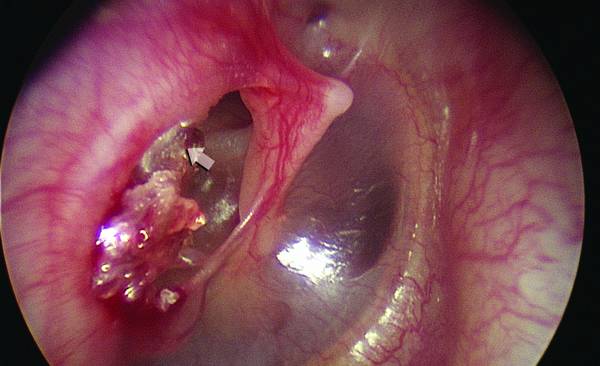
Fig. 15.2 Right ear. Marginal posterior eardrum perforation involving the anulus, with skin migration into the tympanic cavity. In this case epithelialization of the middle ear is anticipated.

Fig. 15.3 Right ear. Eardrum perforation with inflammatory mucosae in the tympanic cavity. In this condition pharmacological therapy must be applied before surgery. The percentage of failures in this inflammatory phase is considerable. a, b General view of the eardrum. c, d Endoscopic view of the mesotympanic (c) and protympanic (d) spaces.
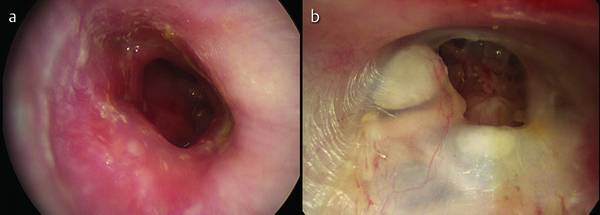
Fig. 15.4 Preoperative endoscopic evaluations. a Right ear. Unstable eardrum perforation, associated with recurrent otorrhea. b Right ear. Dry anterior perforation of the eardrum.
Tubaric function A test to evaluate tubaric function in an open tympanum should be considered in all patients with perforation and candidates for surgery. If the patient has good tubaric function, transcanal technique provides good surgical results with malleable grafts such as temporalis muscle fascia and tragal perichondrium. If the function of the eustachian tube is not good, postoperative outcomes are certainly poor and new perforations may be expected. Rigid materials such as tragus or concha cartilage are of course preferable for reconstructing the eardrum and can provide additional certainty of sealing of the graft.4 In those cases where the eustachian tube is not properly functional, however, one can consider an overlay traditional microscopic technique, which proves to be more effective than the underlay technique with either microscope or endoscope.
In addition to the above criteria related closely to the condition of the tympanic cavity, the tubaric function, and the appearance and position of the perforation to be repaired, selection of the patient for surgery and surgical indications cannot be divorced from analysis of other key issues that must be considered before surgery. The preoperative analysis must therefore consider the following tests.
Analysis of the external auditory canal The analysis of the external auditory canal before surgery should reveal the presence of inflammation, infection, or eczema, which may involve the skin of the external auditory canal and affect surgical results. A preoperative assessment of the caliber of the external auditory canal and the presence of osteomas should be evaluated as part of the selection of patients.
ENT examination The presence of rhinopharyngeal and rhinosinusal tract pathology (chronic allergic and nonallergic rhinitis, nasal polyposis, adenoid hypertrophy or a history of cleft palate) should prompt extensive monitoring before the surgical decision. Radiation treatment for cancers (parotid or skin) should be considered before accepting the indication for surgery
15.3.1 Pure Tone Audiometry
The audiographic evaluation is of fundamental importance for the surgical indication and for the choice of candidates to undergo surgery. In all cases there is an evaluation of pure bone and air conduction tone frequencies of 250 Hz, 500 Hz, 1000 Hz, 2000 Hz, 4000 Hz, and 8000 Hz and vowel audiometry. The auditory values of the contralateral ear must always be considered before a surgical choice: in the case of profound contralateral sensorineural hearing loss, surgery may be ruled out.
15.3.2 Role of Imaging
A systematic middle ear CT scan is not always required before surgery. Preoperative middle ear CT should be reserved exclusively for those perforations associated with retraction pockets (pars flaccida and/or pars tensa), which are hard to explore even with endoscopes, to exclude an underlying hidden cholesteatoma.
15.4 Surgical Approach
15.4.1 Setup of the Patient and Surgeon
The setup of the patient and the surgeon is identical to that for the operation performed under the microscope (▶ Fig. 15.5, ▶ Fig. 15.6). For a right-handed surgeon the camera endoscope is held in the operator’s left hand, the right hand manipulates the instrument or aspiration (▶ Fig. 15.7).

Fig. 15.5 The arrangement of the patient for endoscopic ear surgery.

Fig. 15.6 a, b The arrangement of the surgeon during endoscopic ear surgery. The monitor is in front of the surgeon, and the microscope is also ready for use even if an exclusively endoscopic approach is planned.
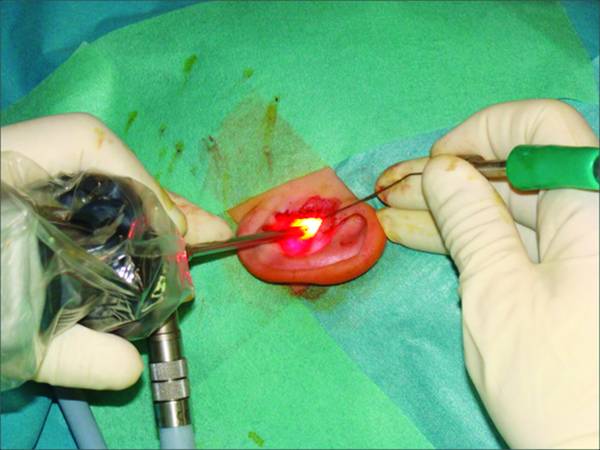
Fig. 15.7 Position of the hands of the surgeon during the endoscopic transcanal approach. The endoscope is held with the left hand, the instrument with the right hand.
Depending on the length of the endoscope used, the operator’s left hand is placed on the patient’s left shoulder for operation on a left ear. For a right ear, the left hand has to have a support so as to avoid uncomfortable tension in the surgeon’s shoulder.
Endoscopes commonly used are Karl Storz, 0°, 6 cm long, 4 mm diameter or 15 cm long, 3 mm diameter. The endoscope is coupled to a cold light source, an HD camera, and a monitor.
Depending on the characteristics of the perforation, the external auditory canal, and the middle ear–related findings (state of the tympanic cavity and eustachian tube function), the endoscopic transcanal technique can be performed in two ways:
Myringoplasty through the creation of a tympanomeatal flap
Direct myringoplasty without creating a tympanomeatal flap (myringoplasty with fat; butterfly myringoplasty with cartilage).
15.5 Myringoplasty Through the Creation of a Tympanomeatal Flap
This surgical technique can be performed using different grafts,5,6 depending on the condition of the perforation and the condition of the tympanic cavity and tubaric function.
We distinguish two types of grafts:
Fascial grafts
Cartilage grafts.
15.5.1 Sampling and Preparation of the Graft
Sampling of Temporalis Fascia
A 1.5-cm incision is made in the superior portion of retroauricular area and the temporal muscle fascia is exposed (▶ Fig. 15.8); a small fragment of fascia is harvested and appropriately shaped and thinned and placed as underlay.
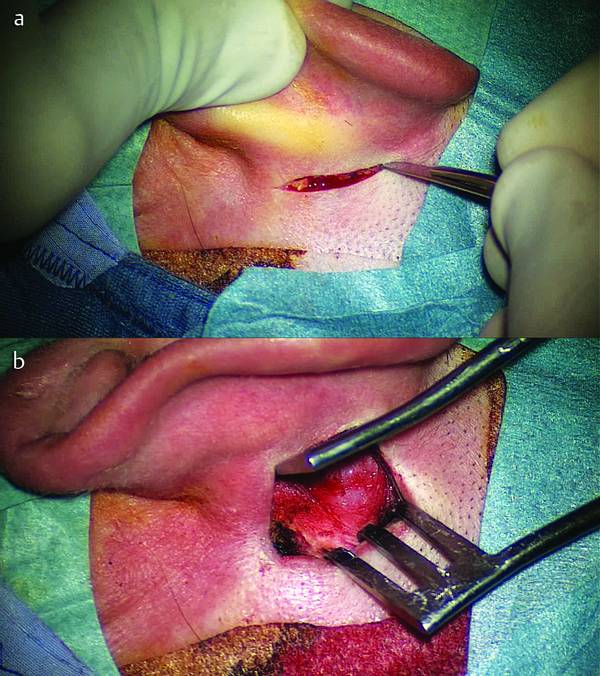
Fig. 15.8 a A small incision is made in the retroauricular sulcus. b Temporalis fascia is harvested.
The fascia is kept in air so that it will be dry and is subsequently modeled according to the defect to be repaired.
Harvesting of Cartilage or Tragal Perichondrium
A small incision is made in the posterior aspect of the tragus and the cartilage with the perichondrium is exposed. If only perichondrium is needed, it will be necessary to isolate the perichondrium from the underlying cartilage and to perform a delicate subperichondrial dissection of the perichondrium from the underlying cartilage, subsequently using a scalpel for a selective removal of perichondrium; this will be kept in air to dry and will then be modeled, according to the defect to be repaired. When cartilage is needed, it will be left adherent to the perichondrium of both faces of the cartilage (front and rear) and a portion of tragal cartilage will be isolated that more or less matches the defect to be repaired.
A fragment of cartilage is taken, with perichondrium, and appropriately thinned and tailored for reconstruction of the tympanic membrane.
The graft is then treated; the layer of perichondrium that covered the cartilage on the front side is gently removed, stripping the cartilage from this side. The perichondrium of the posterior surface of the cartilage is retained, however. In dissection, a circumferential island of cartilage is created that will be maintained at the center of the perichondrial package; this can be done by removing a piece of cartilage from the naked cartilage side, taking care to preserve the perichondrial bundle that covers the posterior surface. The island of cartilage is formed to accord with the defect of the tympanic membrane. Once the island cartilage has been obtained, the residual cartilage will be carefully thinned with a scalpel to produce a thin sheet of cartilage adherent to the perichondrium. The graft thus prepared is left to dry (▶ Fig. 15.9). In our practice, the type of perforation, the state of the middle ear, and the tubaric function must be considered to guide the surgeon in the choice and harvesting of the most suitable graft.
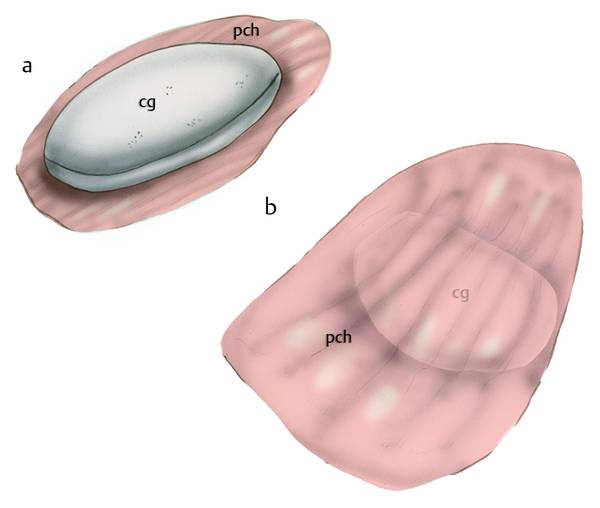
Fig. 15.9 Cartilage graft. a A circumferential island of cartilage is formed according to the eardrum defect. b The perichondrial layer on the posterior surface of the cartilage is modeled, maintaining the adherence of the cartilage. cg, cartilage graft; pch, perichondrial layer.
Graft of Temporalis Fascia or Tragal Perichondrium
Indications
Perforations of anterior or posterior sectors, limited to one sector with normal tubaric function tests, with or without retractions of the pars tensa.7,8
Relative Contraindications
Other failed myringoplasty procedures with fascia/perichondrium
Tubaric function tests suspicious for tubaric insufficiency
Subtotal perforations with involvement of both sectors with only anterior residual anulus.
Cartilage Graft
Indications
Perforations associated with tubal function tests suspicious for tubaric insufficiency, perforations associated with impaired quality of the middle ear mucosa (granulation, inflammation), with a history of recurrent otorrhea. Perforation of the eardrum with involvement of the anulus9–11
Several failed myringoplasty procedures with fascia/perichondrium
Subtotal or anterior sector perforations.
15.5.2 Surgical Technique
Depending on the position of the perforation and the co-presence of retraction areas of the pars tensa, the tympanomeatal flap will differ according to the type of detachment and the peduncle.
Posterior Perforations
Posterior perforations are typically most easily dealt with endoscopically using endoscopes with 0° view, 15 cm long and 3 mm in diameter.
Using a 0° endoscope, the EAC is infiltrated with a mixture of mepivacaine 2% with epinephrine about 3 minutes before the surgical approach.
A crescent-shaped scalpel is used to scratch the edges of the tympanic perforation circumferentially under endoscopic control.
Incision of the EAC is made about 0.5 to 1 cm lateral of the fibrous anulus. The incision is made from the 6 o’clock to the 12 o’clock position; it can be made with a molecular resonance scalpel (Vesalius), a flexible CO2 laser, or a round knife.
Key point: the use of molecular resonance scalpels and CO2 lasers reduces bleeding during surgery (▶ Fig. 15.10, see Clinical case 1 [▶ Fig. 15.11, ▶ Fig. 15.12]).
The tympanomeatal flap is detached from the bone using cottonoids soaked in epinephrine (50% with saline solution), to avoid excessive bleeding. Flap dissection proceeds medially, pushing the skin medially and anteriorly, encompassing the incision until the fibrous anulus is identified (see Clinical case 1 [▶ Fig. 15.12]) Curved elevators are used to dissect the flap, paying attention to the “feel” of the bone under the instrument, effectively “scraping” the skin from the bone.
Key point: Bleeding after incision of the skin of the EAC occurs in most cases, and should be controlled by the use of epinephrine-soaked cottonoids, placed on the point of bleeding in the skin for about 1 minute.
The fibrous anulus is raised using a microhook and once raised allows a good view of the middle ear. Dissection of the flap proceeds from posterior to anterior, keeping the flap adherent to the front edge of the handle of the malleus; the dissection of the flap from the handle of the malleus is performed with a crescent-shaped scalpel. During dissection of the tympanic membrane from the handle of the malleus, with particular care and sensitivity, the blade of the crescent-shaped scalpel cuts the periosteum region on the posterior edge of the handle of the malleus. Once the appropriate plane has been established, the tympanic membrane can be dissected from the malleus before it is isolated; the flap remains attached to the anterior edge of the malleus (▶ Fig. 15.13).
Key point: The umbus region is particularly adherent to the handle of the malleus for the presence of fibrous ligaments. We recommend dissection of these ligaments with microscissors in this area.
After pulling the flap anteriorly, releasing the posterior edge of the long process of the malleus and leaving it adhering to the handle of the malleus on its anterior edge, we proceed to the endoscopic inspection of the tympanic cavity. The use of a 45°, 15-cm-long, 3-mm-diameter endoscope allows inspection of the retrotympanic and isthmic regions; given the incomplete type of tympanomeatal dissection, the protympanic region is only partially exposed (see Clinical case 1 [▶ Fig. 15.14]). With careful maneuvers one may evaluate the protympanum, using the endoscope below the handle of the malleus, being careful not to bump into the bone itself as this could result in dislocation of the malleus.
The next step consists of introducing the chosen graft (there is no difference in the insertion technique for fascia and for cartilage) below the malleus with underlay technique, pushing the graft anteriorly, below the anterior segments, with a blunt hook. In this stage a 0° endoscope is useful because it gives a good view of the anterior segments and the anterior anulus (▶ Fig. 15.15; see Clinical case 1 [▶ Fig. 15.16]).
Once that is done, the fascia is internalized and lateralized to join the tympanomeatal flap, while the island cartilage can be positioned in two different ways. With small perforations we remodel the naked island of cartilage to the same size as the perforation in an attempt to obtain a join: the denuded portion of cartilage will be positioned laterally to the tympanic residues, fitting through the perforation, and the perichondrium will be medial to the tympanic residues and positioned below the malleus (see Clinical case 1 [▶ Fig. 15.16]).
This technique generates a more stable support but it requires considerable accuracy that is sometimes difficult to achieve. Alternatively, the island cartilage is placed medially and the tympanic contact will be between the residues and the perichondrium: this solution is patently easier to achieve.
The next step is positioning Gelfoam into the tympanic cavity, taking care not to block the eustachian tube and the isthmic region (as some fibrotic tissue may be formed as scar on the site of placement), so as to allow good ventilation (see Clinical case 1 [▶ Fig. 15.17]). The tympanomeatal flap is repositioned and good apposition of the graft with the tympanic membrane is checked through the endoscope (see Clinical case 1 [▶ Fig. 15.17, ▶ Fig. 15.18]). The endoscope permits particularly good control of the anterior anulus and its relationship with the graft, which will be very important for the success of surgery. There is virtually no drilling of the bone of the external auditory canal with the endoscopic technique; this is reserved only for cases of osteomas that block the exposure of the anulus.
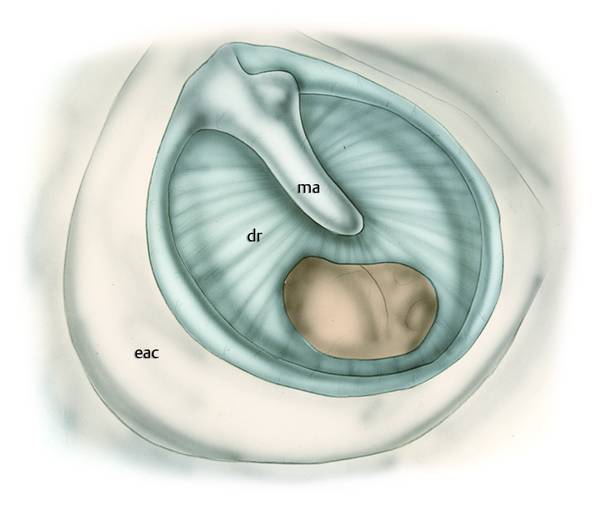
Fig. 15.10 Right ear. Posterior perforation of the eardrum; incision of the skin in the external auditory canal. ma, malleus; dr, eardrum; eac, external auditory canal.
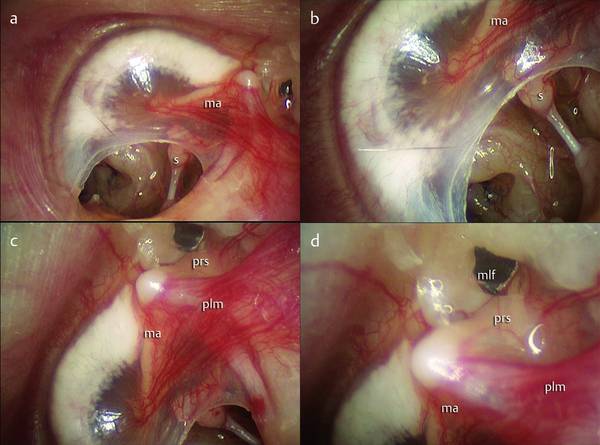
Fig. 15.11 Clinical case 1. Left ear. a, b Posterior perforation of the eardrum with involvement of the anulus. c, d The Prussak space is investigated endoscopically. ma, malleus; s, stapes; plm, posterior ligamental fold of the malleus; prs, Prussak space; mlf, malleolar lateral fold.
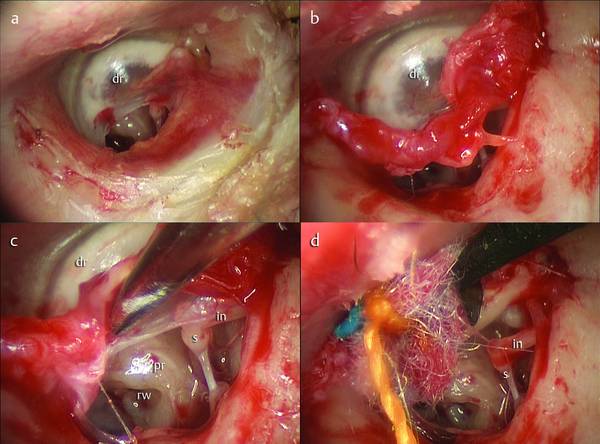
Fig. 15.12 Clinical case 1. Left ear. a An incision of the external auditory canal is made with a Vesalius. b, c The tympanomeatal flap is gently elevated using cottonoids soaked with epinephrine solution. d The dissection of the flap ends on the handle of the malleus. s, stapes; pr, promontory, rw, round window; in, incus; dr, eardrum.
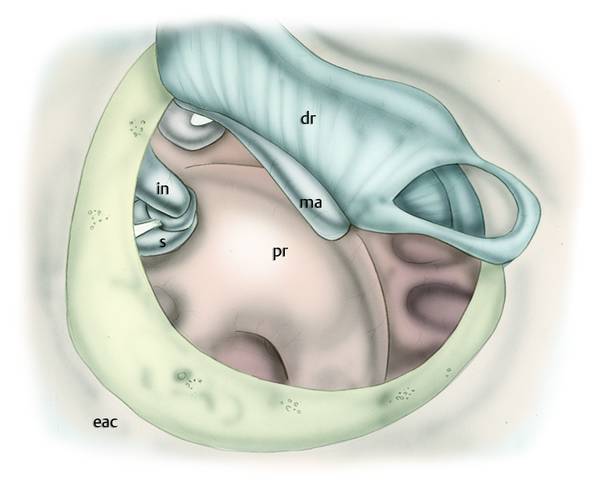
Fig. 15.13 Right ear. The dissection of the eardrum from the handle of the malleus is performed carefully, detaching the eardrum from the posterior aspect of the malleus. ma, malleus; s, stapes; pr, promontory; in, incus; eac, external auditory canal; dr, eardrum.
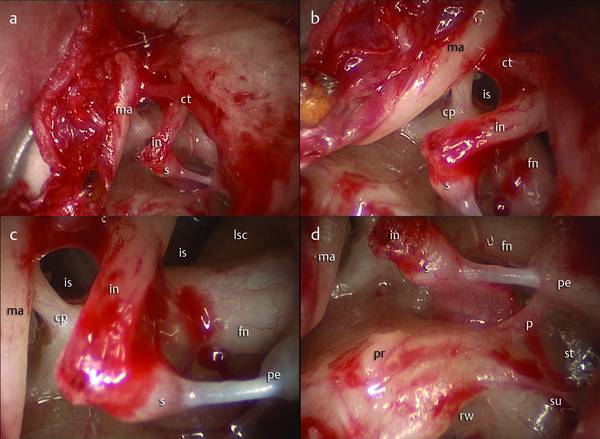
Fig. 15.14 Clinical case 1. Left ear. a After elevation of the tympanomeatal flap, the tympanic cavity can be inspected endoscopically. b, c Particular attention should be paid to exploring the ventilation routes of the middle ear; a 45° endoscope allows us to see the anterior and posterior isthmus, detecting the presence of an open isthmus (if one exists, as in this patient) or a blockage of the isthmus. d The retrotympanum is also detected endoscopically. ma, malleus; s, stapes; pr, promontory, rw, round window; in, incus; su, subiculum; p, ponticulus; st, sinus tympani; pe, pyramidal eminence; fn, facial nerve; is, isthmus; cp, cochleariform process; lsc, lateral semicircular canal; ct, chorda tympani.
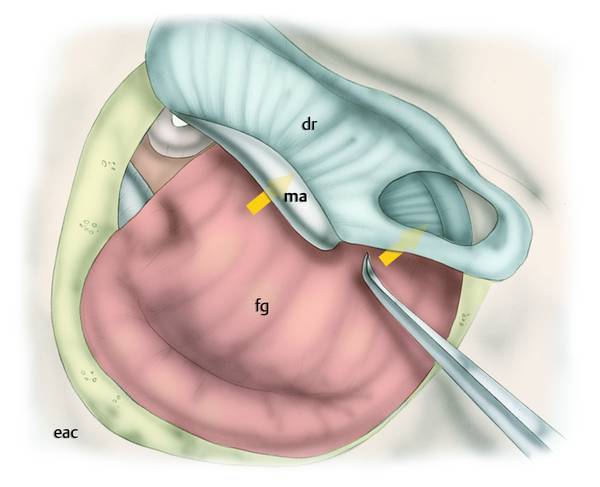
Fig. 15.15 Right ear. The graft is inserted under the malleus, paying attention to pushing the graft anteriorly to cover the entire eardrum defect (orange arrows). dr, eardrum; ma, malleus; eac, external auditory canal; fg, fascia graft.
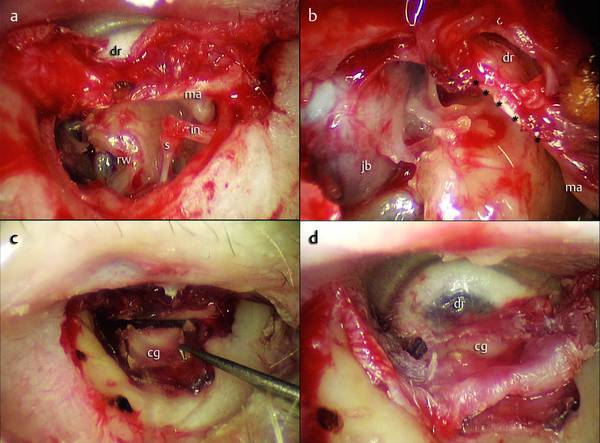
Fig. 15.16 Clinical case 1. Left ear. a The tympanomeatal flap is elevated and the posterior aspect of the handle of the malleus is exposed. b The anterior lip of the eardrum perforation (*****) can be inspected endoscopically. c In this case, where the anulus was involved by the perforation, a cartilage graft was harvested; the cartilage graft is pushed under and anteriorly to the handle of the malleus. d The tympanomeatal flap is then repositioned over the graft. dr, eardrum; ma, malleus; in, incus; s, stapes; cg, cartilage graft; jb, jugular bulb; rw, round window; *****, anterior lip of the eardrum perforation.
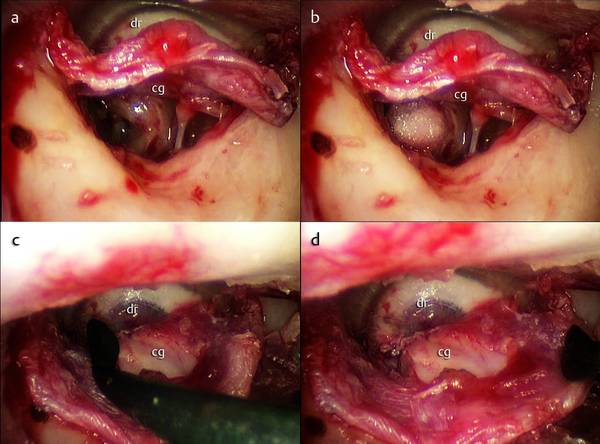
Fig. 15.17 Clinical case 1. Left ear. a, b The tympanic cavity is packed with Gelfoam to support the graft. c, d The tympanomeatal flap is repositioned on the cartilage graft. dr, eardrum; cg, cartilage graft.
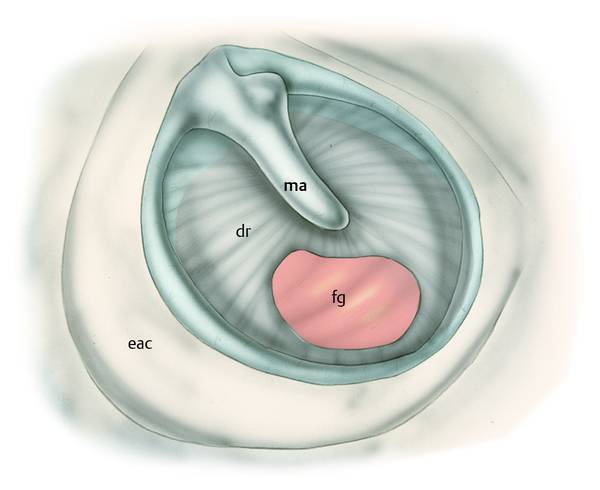
Fig. 15.18 Right ear. Final result after repositioning the tympanomeatal flap. ma, malleus; fg, fascia graft; dr, eardrum; eac, external auditory canal.
Alternative technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


