CHAPTER 55 Endoscopic Dacryocystorhinostomy
Endoscopic dacryocystorhinostomy (DCR) was first described in the otolaryngology literature by McDonogh1 in 1989. Over the ensuing years, there has been a steady improvement in outcomes owing to advances in surgical technique, instrumentation, and comprehension of the anatomy. Specifically, once the superior extent of the lacrimal sac was recognized to extend significantly above the middle turbinate, surgical outcomes improved.2 Today’s endoscopic DCR is a reliable and effective technique that is comparable to external DCR in outcome measures.3–6 In 2007, endoscopic DCR was reported to be economically superior to the external technique.7
Pathophysiology
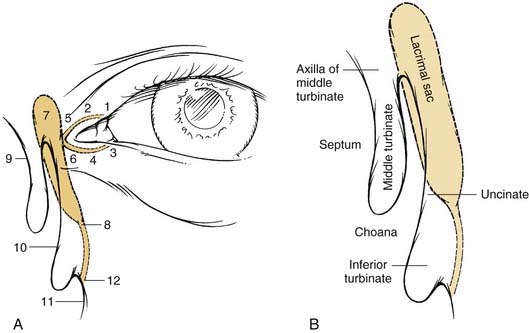
Obstructions of the lacrimal apparatus can occur anywhere along its course. DCR surgically bypasses the most distal portion of the lacrimal apparatus, creating a new outflow in the lateral wall of the nasal cavity instead of below the inferior turbinate. Thus, DCR is specifically designed to manage obstructions of the lacrimal sac and duct. It is important to note that DCR is not capable of reliably managing obstructions within the lacrimal apparatus proximal to and including the common canaliculus (Fig. 55-1). In selected cases, a stenosis of the common canaliculus immediately proximal to its entry into the lacrimal sac can be managed by temporary stenting with O’Donoghue tubes.
There are two principal categories of lacrimal obstruction, anatomic and functional. Anatomic obstructions are more common than functional obstructions, the approximate rates being 70% and 30% respectively.5 Anatomic obstructions are complete blockages most commonly noted between the lacrimal sac and nasal cavity. Functional obstructions are caused by either critical narrowings within the lacrimal system that delay normal lacrimal flow or a failure of the proximal pumping mechanism. Both anatomic and functional obstructions may be managed with endoscopic DCR; however, surgery of anatomic obstructions is noted to have superior outcome.
Evaluation
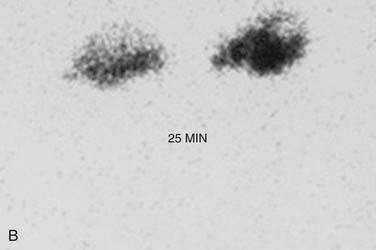
Radiologic evaluation of lacrimal obstructions begins with the dacryocystogram (DCG). Because it, like saline irrigation, causes elevated pressures within the lacrimal system, this study is capable of diagnosing only anatomic obstructions (Fig. 55-2). Failure of DCG to identify a blockage in a symptomatic patient necessitates lacrimal scintilligraphy. Unlike DCG, scintilligraphy is a physiologic test of the lacrimal system; thus functional obstructions cause delays in the flow of radioisotopes from the conjunctiva into the nasal cavity over the 30-minute duration of the test. If isotope delay is detected in the lacrimal sac during the test, a narrowed segment is more likely than a failure of the lacrimal pump mechanism (Fig. 55-3). However, if the isotope does not penetrate the lacrimal system, a pump failure is then more likely. Studies have shown that outcome of DCR performed for anatomic obstructions is superior to that of DCR done for functional obstructions.5 The ability to confirm an obstruction with scintilligraphy and to differentiate anatomic from functional obstruction with DCG allows the surgeon to better prepare the patient for the prognosis of the procedure.
Surgical Technique (Video clip available on website.)
Nasal preparation is performed with both pledget-applied vasoconstrictor and lateral nasal wall injection of 2% lidocaine with 1 : 80,000 adrenaline. The injection is performed in two places: superior to the axilla and well anterior to the uncinate process. If a septoplasty must be performed, the septum is likewise injected. Endoscopic septoplasty is performed in 48% of cases,8,9 because any narrowing of the anterior nasal cavity increases the complexity of the procedure dramatically. Generally, the septoplasty is very limited and specifically addresses the most anterior and superior portion of the bony septum. This area is checked for adequacy by gentle medialization of the septal mucosa to ascertain mobility in the region medial and anterior to the axilla (Fig. 55-4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree