CHAPTER 190 Early Detection and Diagnosis of Infant Hearing Impairment
Principles and Techniques of Newborn Hearing Assessment
History of Infant Hearing Screening
The importance of early identification of hearing loss has been recognized for many years.1–3 Undetected hearing loss present from an early age can impede acquisition of speech, language, cognitive, and social-emotional development.
Joint Committee on Infant Hearing
The Joint Committee on Infant Hearing (JCIH), of which the American Academy of Otolaryngology–Head and Neck Surgery is a founding member, was established in 1969 with the goal of developing more accurate and efficient methods of identifying neonatal hearing impairment. In 1972, the JCIH recommended the use of a High-Risk Registry (HRR) to identify neonates at higher-than-normal risk for hearing loss. It recommended these infants be referred for audiologic testing within the first 2 months of life. In 1982,4 1990,5 and 19946 the JCIH issued updated high-risk criteria. The 1994 HRR included family history of hereditary childhood sensorineural hearing loss, in utero infection (e.g., toxoplasmosis, other viral infections, rubella, cytomegalovirus infection, and herpes simplex [TORCH]), craniofacial anomalies, birth weight less than 1500 g, hyperbilirubinemia severe enough to necessitate an exchange transfusion, ototoxic medications including but not limited to use of aminoglycosides in multiple courses or in combination with loop diuretics, bacterial meningitis, Apgar scores of 0 to 4 at 1 minute or 0 to 6 at 5 minutes, mechanical ventilation lasting 5 days or more, and presence of stigmata or other findings associated with a syndrome known to include sensorineural or conductive hearing loss. However, the JCIH recommended HRR use only if universal newborn hearing screening (UNHS) was unavailable. Only 2% to 5% of neonates with one or more risk factors exhibit a moderate to profound hearing loss. Conversely, 95% to 98% of neonates with one or more risk factors have normal hearing.7 Furthermore, 50% of children with moderate to profound congenital hearing loss exhibit no risk factors for hearing loss.8 This means that use of the HRR alone, as an indication for hearing testing, would leave at least 50% of infants with congenital hearing loss undiagnosed. In 2007, the JCIH recommended hearing screening for all newborns, with formal audiologic assessment in those who fail the initial screening test by 3 months of age, followed by intervention by 6 months of age for children with significant hearing loss.9
Delay in Identification
A significant delay exists in the identification and intervention of hearing impairment for infants without risk factors. For infants with mild to moderate hearing loss, a 1996 survey showed that parents of high-risk infants first suspected the loss when their infants were at a median age of 8 months. By contrast, the parents of infants without risk factors first suspected their infant had a hearing loss when the child was 15 months old.10,11 Hearing loss was confirmed in infants without risk factors at 22 months of age, compared with 12 months of age for infants with risk factors, and infants were enrolled in intervention at 28 and 18 months, respectively. Ages of suspicion (7 to 8 months), diagnosis (12 to 13 months), and intervention (18 to 19 months) were essentially the same for infants with severe to profound hearing loss, regardless of whether risk factors were present. Recent retrospective studies indicate that infants with hearing loss enrolled in appropriate early intervention by 6 months of age incur significantly fewer delays than those who enroll after 6 months of age.10,12 These findings are for children with all degrees of hearing loss, as well as for children with other handicapping conditions.
Universal Newborn Hearing Screening
In 1993, the National Institute for Deafness and Other Communicative Disorders (NIDCD) Consensus Conference on Early Identification of Hearing Loss recommended UNHS for infants within the first 3 months of life, preferably before hospital discharge.13 Subsequently, several organizations and government agencies have endorsed UNHS as the best way to ensure early detection and habilitation of hearing loss. These groups include the Academy of Otolaryngology–Head and Neck Surgery, American Academy of Pediatrics, American Speech-Language-Hearing Association, American Academy of Audiology, and others. Despite considerable disagreement concerning the relative merits of specific measurement approaches for neonatal hearing screening and whether UNHS is even appropriate at this time,14 universal newborn and infant hearing screening statutes have been passed in 41 states (legislation is pending in two states), and all states have implemented newborn hearing screening programs.9 The goals of the U.S. Department of Health and Human Services’ initiative Healthy People 2010 include UNHS by 1 month of age, diagnostic confirmation of hearing loss by 3 months of age, and enrollment in appropriate early intervention for children with hearing loss and their families by 6 months of age.15 The Newborn Infant Hearing and Screening Intervention Act of 1999 provided funding to help states reach this goal. In 2008, the U.S. Preventive Services Task Force published a grade B recommendation to screen for hearing loss in all newborn infants.16
Prevalence of Sensorineural Hearing Loss in Children
Estimates of congenital sensorineural hearing loss (SNHL) vary, ranging from 1 per 1000 to 3 per 1000 live births, depending on the degree of hearing loss. Bilateral severe to profound hearing loss (70 dB HL or greater) occurs in 1 per 1000 live births. When the results of several studies are averaged, approximately 3 per 1000 infants have a hearing loss of 30 dB or greater.17–21 The incidence of significant hearing loss is 10 times greater for infants with one or more risk factors than for those with no risk factors.
Progressive, late-onset, and acquired hearing loss in childhood is a continuing challenge. In its survey of deaf and hard-of-hearing school-aged children, Gallaudet Research Institute found a prevalence of significant hearing loss of 1.8% in children 3 to 17 years of age.22 This figure is six times higher than the incidence of hearing loss in the neonatal period. Similarly, van Naarden and colleagues23 reported that the average point prevalence of hearing losses 40 dB or greater increased with age from 0.67% at 3 years of age to 1.38% at 10 years of age. It is important that hearing, speech, and language development be monitored because of the occurrence of progressive, late-onset, and acquired hearing loss in early childhood.
Increase in Early Identification
In those states with UNHS, the average age of identification of congenital hearing loss has dramatically decreased. Rhode Island mandated UNHS in 1993. In 1998, Vohr and colleagues24 reported that the average age at confirmation of permanent hearing loss in Rhode Island infants was 3 months. By contrast, in the absence of UNHS, the average age at diagnosis of permanent hearing loss in children was 31.25 months. In its 1999 Policy Statement, the American Academy of Pediatrics noted: “Reliance on physician observation and/or parental recognition has not been successful in the past in detecting significant hearing loss in the first year of life.”25 Long-term prospective studies of deaf and hard-of-hearing children identified through newborn hearing screening programs are needed to determine if in fact educational and vocational outcomes are significantly better for these children. A recently published controlled trial in the United Kingdom demonstrated that UNHS increased the proportion of 7- to 9-year-old children with permanent hearing loss who were identified before 6 months of age.26 Strong data illustrating improved speech and language development from early interventions are lacking, but one controlled trial found that early detection of childhood hearing impairment leads to higher language scores (but not speech scores) in mid-childhood.27
Principles and Techniques of Newborn Hearing Assessment
Testing Protocols
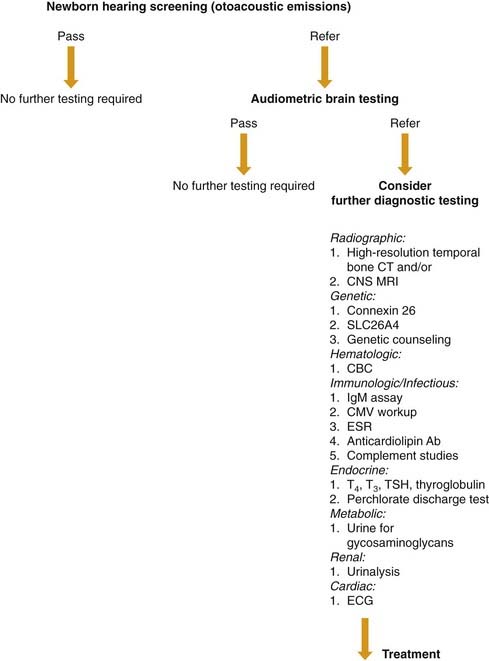
The goal of newborn hearing screening is to identify those infants who need diagnostic hearing evaluations because they are at risk for significant hearing loss. With current technology, screening outcomes are either “pass” or “refer” (Fig. 190-1). “Pass” indicates the infant is not at risk for significant hearing loss and needs no further testing at this time. “Refer” indicates the infant is at risk for hearing loss and requires a diagnostic hearing evaluation. It is important to emphasize to parents and health care providers that “refer” does not mean that the baby has a hearing loss; this designation indicates only that the child has a greater risk of having hearing loss.
Auditory Brainstem Responses
ABR has been used for many years to screen infants in the neonatal intensive care unit (NICU) before hospital discharge.28–32 Recent advances have resulted in the development of automated ABR detection algorithms.33–37 These systems replace the subjective impression of the tester as to the presence or absence of an ABR, with an objective statistical estimate of the likelihood or probability of a “response” distinct from the background “noise.”
Evoked Otoacoustic Emissions
Evoked otoacoustic emissions (EOAEs) are also used widely for newborn hearing screening. EOAEs are acoustic signals generated by the cochlea in response to auditory stimulation. They are a physiologically vulnerable indicator of cochlear status, specifically outer hair cells. EOAE generation is independent of neural activity, so EOAE testing measures cochlear status independent of CNS status. Transient evoked otoacoustic emissions (TEOAEs) occur after a brief click stimulus.38 TEOAEs provide information over a broad frequency range (approximately 500 to 6000 Hz). Distortion product otoacoustic emissions (DPOAEs) occur in response to simultaneous presentation of two pure tones with the appropriate frequency and amplitude ratios and provide frequency-specific information across a broad range of frequencies.39
Almost immediately after the first otoacoustic emissions (OAEs) reports by Kemp and Ryan40 and Kemp, several investigators suggested that one of the potentially most useful clinical applications of OAE is assessment of cochlear status in infants.41,42 In theory, OAEs were thought to (1) take less time to measure than an ABR, because OAEs do not require electrode attachment, (2) provide information over a broader frequency range than click-evoked ABR, and (3) provide cochlear-specific information unaffected by neurologic pathology.
Data from several groups of investigators indicate that robust, broadband TEOAEs can be measured in neonatal ears in the absence of external or middle ear pathology.40,43,44 Likewise, data indicate that DPOAEs are robust in neonates and infants.45–49
Comparison of Otoacoustic Emissions and Auditory Brainstem Responses
To predict hearing status in children 8 to 12 months of age, a multicenter longitudinal study compared the accuracy of click-evoked ABRs, TEOAEs, and DPOAEs. The results indicated no significant differences among the three measures.48 However, a recent study comparing two-step TEOAEs and ABRs found that ABR was more effective for UNHS because it yields fewer false-positive results and a lower referral rate compared with TEOAE, resulting in a smaller percentage of infants lost during follow-up.50
Typically, a simple pass-refer criterion is chosen for a screening tool. Many studies and these programs assume a priori that all infants who “passed” the screen had normal hearing. To determine the true accuracy of neonatal tests, however, it is necessary to follow all infants evaluated during the neonatal period, regardless of neonatal test outcome.48 Because the true hearing status of those infants who pass the screening test is not known, true sensitivity cannot be calculated. Errors made among infants with normal hearing can be known because these false-positive results are evaluated with additional testing. The fact that the “passes” may include infants with hearing loss will have little or no influence on the true-negative rate or specificity of the test, because the vast majority of infants have normal hearing. However, the errors among ears with hearing loss (false-negative results) cannot be known if only those infants failing the newborn hearing test are followed. This is because misses are not followed up. Assigning a “pass” to even a small number of babies with hearing loss can have a large effect on test sensitivity because of the small total number of those with hearing loss.
The sensitivity and specificity of ABR, TEOAE, and DPOAE testing alone or in combination depend on the target degree of hearing loss, the test parameters, and response criteria. For example, Hyde and associates51 reported ABR sensitivity of 98% and specificity of 96% if the average target hearing loss is 40 dB nHL at 2 and 4 kHz. If the target degree of hearing loss is 30 dB nHL, sensitivity and specificity were 100% and 91%, respectively. Norton and coworkers held specificity at 80% and determined sensitivity for TEOAE, DPOAE, and ABR alone and in combination for a target loss of 30 dB nHL. Sensitivity ranged from 80% to 90%. If those infants with known progressive hearing loss were excluded, sensitivity improved.48
OAE testing may miss inner hair cell and eighth cranial nerve hearing losses. OAEs are generated by the outer hair cells and are independent of neural status. Recently, there are concerns about auditory dyssynchrony,52 defined as robust OAEs and abnormal or absent ABR. This is an extremely heterogeneous population whose behavioral hearing status ranges from normal hearing to profound hearing loss. Good incidence data of this disorder in the neonatal population are scarce.
Some hospitals implement two-stage screening, in which OAE is used as the preliminary screening test. Infants failing this test are then screened with the automated ABR (AABR). Those who fail the AABR undergo more diagnostic testing to evaluate for permanent hearing loss, but infants who pass the AABR are not tested further. A multicenter evaluation of the two-stage screening revealed that many infants with hearing loss may be missed, because infants who pass only the AABR are not referred for further testing.53
Diagnosis and Treatment of Hearing Loss in Infants
History
In infants who fail hearing screening tests, a directed history to identify potential sources of hearing loss is appropriate.54 A careful family history looking for hearing loss, ocular abnormalities, congenital cardiac problems in first- and second-degree relatives, and any associated syndromes is essential. Prenatal history for possible maternal infection (i.e., TORCH), gestational diabetes, and hypothyroidism can help direct the evaluation. Maternal use of alcohol should be sought, because fetal alcohol syndrome is associated with auditory dysfunction. Other maternal illnesses and social habits (e.g., drug use and smoking) should be sought. Risk factors for hearing loss in the perinatal period are well known, as discussed earlier in this chapter.6,55