 ales disease is an idiopathic obliterative vasculopathy that usually involves the peripheral retina in young adults. In 1880, Henry Eales first described it in healthy young men with abnormal retinal veins and recurrent vitreous hemorrhages.
ales disease is an idiopathic obliterative vasculopathy that usually involves the peripheral retina in young adults. In 1880, Henry Eales first described it in healthy young men with abnormal retinal veins and recurrent vitreous hemorrhages.
Clinical findings are characterized by avascular areas in the retinal periphery, followed posteriorly by microaneurysms, dilatation of capillary channels, tortuosity of neighboring vessels, and spontaneous chorioretinal scars. It is a diagnosis of exclusion, as many other retinal disorders can mimic Eales disease, especially conditions of retinal inflammation or neovascularization.
Pathophysiology and Clinical Presentation
The pathophysiology of Eales disease is mostly unknown. It is believed to be a primary, noninflammatory disorder of the walls of peripheral retinal vessels that often leads to vascular occlusions, peripheral neovascularization, and vitreous hemorrhage. The microvascular abnormalities are seen at the junction of perfused and nonperfused zones of the retina.
Patients often present with symptoms of floaters, cobwebs, and blurring or decreased vision associated with vitreous hemorrhage. Clinical findings usually involve the retina and the vitreous. Vascular sheathing and hemorrhages of the adjacent nerve fiber layer are the most common findings. The sheathing can range from mild to severe to causing vascular occlusions. Areas of vascular sheathing often leak on fluorescein angiography.
Anterior chamber and vitreous may exhibit cell flare and keratitic precipitates. Cystoid macular edema may occur because of low-grade inflammation. Epiretinal membranes are also a frequent occurrence.
Peripheral nonperfusion is a typical feature of Eales disease. The surrounding vasculature is tortuous with microvascular abnormalities, which include microaneurysms, arteriovenous shunts, venous beading, hard exudates, and cotton-wool spots. Fine solid white lines occasionally can be seen, indicating obliterated larger vessels.
Branch retinal-vein occlusion (BRVO) can be seen in patients with Eales disease; it may be limited to one area or may be multifocal, unlike BRVO alone, which is usually confined to a single affected quadrant and respects the anatomical distribution of the horizontal raphe.
Neovascularization of the disc (NVD) or neovascularization elsewhere (NVE) in the retina is observed in up to 80% of patients with Eales disease. The NVE usually is located peripherally, at the junction of perfused and nonperfused retina. Neovascularization is often the source of vitreous hemorrhage in these eyes. Rubeosis iridis, or neovascularization of the iris, can develop and may lead to neovascular glaucoma. Fibrovascular proliferation on the surface of the retina may accompany retinal neovascularization. These eyes have associated anteroposterior traction that could lead to retinal detachment.
CASE STUDY
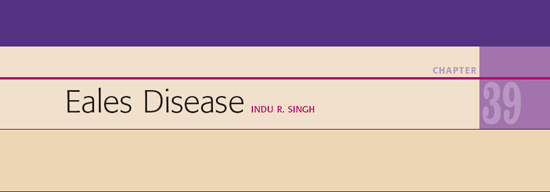
The patient had Eales disease with NVD, NVE, and retinal traction, and pars plana vitrectomy was performed to clear the vitreous hemorrhage and to clear the fibrovascular proliferative tissue created by the disease (Fig. 39.1).
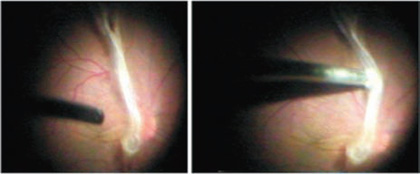
Figure 39.1. A fibrovascular band extends from the disc to the periphery. A vitrectomy cutter was abandoned in favor of a Fugo blade because it created traction on the macula.
Surgical Technique
- In our case, we first tried to use a vitrector to cut the band, but it created traction on the macula, so we abandoned this approach. We decided to use the Fugo blade to cut this band. For this purpose, an elongated 20-gauge Fugo tip was used because it could negotiate the 20-gauge sclerotomies and was long enough to reach the retina (Fig. 39.2).
- Activate the Fugo blade tip and start cutting by merely touching the tissue. No traction is produced while cutting. Cavitation bubbles will be seen while the band is being cut (Fig. 39.2 and 39.3).
- After bisecting the band, direct the Fugo blade to ablate the stubs of the band toward their attachment points on the retina (Fig. 39.4).
- Remove the stubs of the vasoproliferative tissue with a combination of a vitreous cutter, endoscissors, and endo-forceps.
- During this process, the only difficulty we encountered was that the cavitation bubbles rose up and made it hard to see the surgical field. We had to aspirate the bubbles often when they affected visibility beyond a certain point.
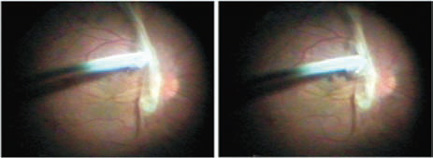
Figure 39.2. The Fugo blade tip is activated and touched to the lesion.
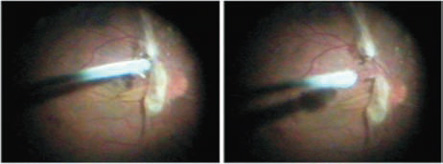
Figure 39.3. The proliferative band is bisected.
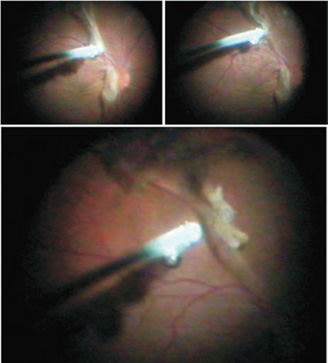
Figure 39.4. The stubs of the vasoproliferative tissue are ablated.
Summary
Although this case is of one of Eales disease, similar pathologic pictures of varying severity are seen in other diseases and similarly result in proliferative fibrovascular tissues. The Fugo blade is excellent in managing complex proliferative tissues.
Suggested Reading
Singh IR. Managing proliferative vitreo-retinopathy with the Fugo blade—a case report. Trop Ophthalmol. 2001;1: 13–16.
Singh IR, Singh D, Singh RK, et al. The plasma blade in vitreoretinal surgery. Ann Ophthalmol. 2001;33:12–20.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


