7 Cornea / External Disease
Anatomy / Physiology
Precorneal Tear Film
Layers
Cornea (Figure 7-1)
Average measurements
Epithelium
50 µm thick (5% of corneal thickness); hydrophobic (hydrophilic molecules penetrate poorly)
Stroma
480 µm thick centrally, 900 µm peripherally; 78% water by weight
Descemet’s membrane
3 (birth) to 12 µm (adults) thick; PAS-positive basement membrane
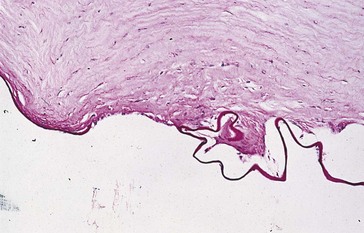
Figure 7-2 Hydrops demonstrating corneal edema (thickening) with breaks in Descemet’s membrane.
(From Yanoff M, Fine BS: Ocular Pathology, 5th edn, St Louis, Mosby, 2002.)
Endothelium
Stains
Conjunctival Disorders
Inflammation
Follicles
Gray-white round elevations with avascular center and vessels at periphery
Generally most prominent in inferior fornix (except in trachoma)
Papillae
Small to large elevations with central vascular tuft and pale avascular valleys
Nonspecific reaction to conjunctival inflammation (edema and leakage of fluid from vessels)
Degenerations
Concretions (Lithiasis)
Small, round, yellow-white deposits in palpebral conjunctiva
May erode through conjunctiva and abrade ocular surface causing foreign body sensation
Conjunctivochalasis
Redundant, loose, nonedematous inferior bulbar conjunctiva interposed between globe and lower eyelid
Pingueculum
Small nodule composed of abnormal subepithelial collagen; may calcify
Located at limbus, nasal more common than temporal; does not involve cornea
Caused by actinic (UV light) exposure
Allergy
Allergic Conjunctivitis
20% of the US population has allergies
90% of patients with systemic allergies will have ocular symptoms
Most commonly seasonal or perennial allergic conjunctivitis
Associated with allergic rhinitis
Atopic Keratoconjunctivitis (AKC)
Atopy
hereditary allergic hypersensitivity (10–20% of population)
Types I < IV hypersensitivity reactions
Onset usually between ages 30 and 50 years
Clinical diagnosis (atopic skin disease [eczema], hay fever, asthma)
Superior Limbic Keratoconjunctivitis (SLK)
Recurrent inflammation of superior bulbar and palpebral conjunctiva; unknown etiology
Associated with CL wear and thyroid dysfunction (50%)
Female preponderance (70%), onset usually between ages 30 and 55 years
Recurrent episodes; lasts 1–10 years, eventually resolves permanently
70% bilateral; symptoms worse than signs
Infectious Conjunctivitis
May be hyperacute, acute, or chronic
Usually viral in adults and bacterial in children
Findings
DDx of conjunctivitis with preauricular lymphadenopathy
EKC, HSV, Gonococcus, Chlamydia, Parinaud’s oculoglandular syndrome, Newcastle’s disease
Viral
Adenovirus
Epidemic keratoconjunctivitis (EKC)
adenovirus types 8, 19 and 37; bilateral in 75% to 90%
Newcastle’s Disease
Unilateral follicular conjunctivitis, pneumonitis, preauricular lymphadenopathy
Occurs in poultry handlers; self-limited, lasts 1 week
Bacterial
Hyperacute (<24 hours)
Copious purulent discharge, marked conjunctival injection and chemosis
Acute (hours to days)
Purulent discharge, not as severe as hyperacute
Streptococcus pneumoniae, Staphylococcus, Haemophilus influenzae, Pseudomonas
Chlamydial
Inclusion Conjunctivitis (TRIC – Trachoma Inclusion Conjunctivitis)
Chlamydia trachomatis serovars D to K
Chronic, follicular conjunctivitis
Associated with urethritis (5%)
Trachoma
Bilateral keratoconjunctivitis; leading cause of preventable blindness
Chlamydia trachomatis serovars A to C
Classification
Other Conjunctivitis
Staphylococcal Disease
Blepharitis, conjunctivitis, keratitis (SPK, marginal infiltrates), phlyctenule
Tumors
Cystic Tumors
Squamous Tumors
Squamous Papilloma
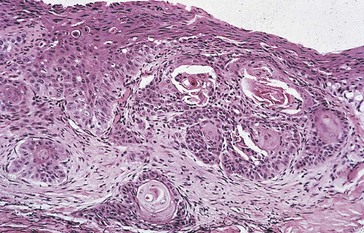
Pathology
vascular cores covered by acanthotic, nonkeratinized, stratified squamous epithelium (Figure 7-4)
Conjunctival Intraepithelial Neoplasia (CIN)
Replacement of conjunctival epithelium by atypical dysplastic squamous cells
Usually transluscent or gelatinous appearance; <10% exhibit leukoplakia (keratinization)
Carcinoma in situ
Usually begins at limbus and spreads onto cornea
Associated with HPV subtype 16 and 18 (check HIV in young patient), and actinic exposure
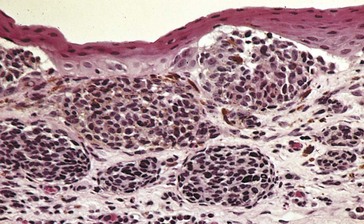
Pathology
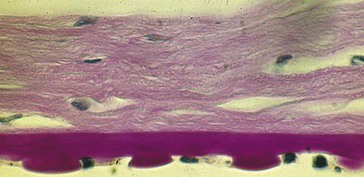
dysplastic epithelium spreads anterior to Bowman’s membrane, fine vascularity with hairpin configuration (similar to papilloma), anaplastic cells, dyspolarity (Figure 7-5)
Squamous Cell Carcinoma
Malignant cells have broken through epithelial basement membrane
Most common malignant epithelial tumor of conjunctiva; rarely metastasizes
Most common in Africa and Middle East
Appearance similar to carcinoma in situ
Mucoepidermoid Carcinoma
Rare, aggresive variant of squamous cell carcinoma with malignant goblet cells
Typically occurs in individuals >60 years old
Very aggressive, can invade globe through sclera
Suspect in cases of recurrent squamous cell carcinoma
Pathology
epidermoid and mucinous components; stains with mucicarmine, Alcian blue, and colloidal iron
Melanocytic Tumors
Racial Melanosis
Light brown, flat, perilimbal pigmentation; increased melanin in basal epithelium
Most common in pigmented individuals
Nevus
Congenital nests of benign nevus cells along basal epithelial and / or substantia propria
50% have epithelial inclusion cysts
Often enlarges or becomes more pigmented during puberty or pregnancy
Types (classified by location)
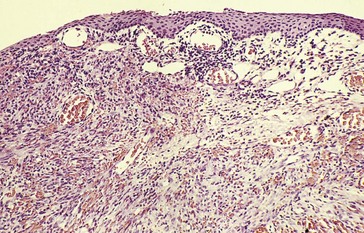
Primary Acquired Melanosis (PAM, Acquired Melanosis Oculi)
Unilateral, flat, diffuse, patchy, brown pigmentation; waxes and wanes
Proliferation of intraepithelial melanocytes; no cysts (Figure 7-8)
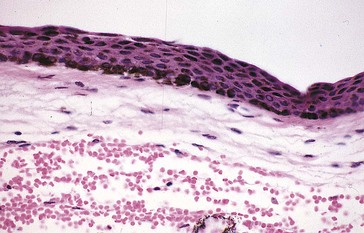
Figure 7-8 PAM with pigmentation throughout the epithelium.
(From Yanoff M, Fine BS: Ocular Pathology, 5th edn, St Louis, Mosby, 2002.)
Analogous to lentigo maligna of skin
Occurs in middle-aged to elderly whites
20–30% risk of malignant transformation, nodular thickening is indication for excisional biopsy
Secondary Acquired Conjunctival Melanosis
Addison’s disease, radiation, pregnancy, topical epinephrine
Malignant Melanoma
Rare, variably pigmented, elevated mass most commonly on bulbar conjunctiva
Arises from PAM (67%) or preexisting nevi (25%), or de novo
Pathology
intraepithelial pagetoid spread; need to bleach specimen to determine amount of atypia (Figure 7-9), stain with S-100 and HMB-45
Vascular Tumors
Kaposi’s Sarcoma
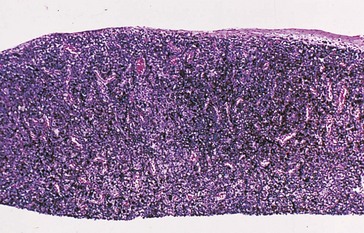
Lymphoid Tumors
(See Ch. 6, Orbit / Lids / Adnexa)
Smooth, flat, fleshy, salmon-colored mass; single or multiple
Occurs in substantia propria; overlying epithelium is smooth; can be bilateral
20% associated with systemic disease (but systemic lymphoma rarely presents in conjunctiva)
Requires systemic workup, including CT scan, bone scan, SPEP, medical consultation
Other Tumors
Fibrous Histiocytoma
Yellow-white mass composed of fibroblasts and histiocytes
Extends from limbus to peripheral cornea
Benign Hereditary Intraepithelial Dyskeratosis (BHID) (AD)
Originally seen in triracial families in Halifax County, North Carolina (Haliwa Indians)
Usually presents in 1st decade of life
Corneal Disorders
Trauma
Abrasion
Epithelial defect, most commonly traumatic (e.g. fingernail, plant branch)
Increased risk of infection, especially in contact lens wearer
Foreign Body (FB)
Often metal (usually associated with adjacent rust ring), glass, or organic material
Laceration
Partial- or full-thickness cut in cornea
Requires surgical repair and topical antibiotic and steroid
Burns
Alkali
denatures but does not precipitate proteins, also saponifies fat; therefore penetrates deeply
Radiation
thermal burn (similar to acid burn)
Grading systems
 to
to  of limbus; guarded prognosis
of limbus; guarded prognosisTreatment
Ocular Surface Disease
Causes tear film disturbance and dry eye
Due to deficiency in tear film component(s)
Keratoconjunctivitis Sicca
Adult women (95%), often associated with Sjögren’s syndrome

 OF CORNEA: lagophthalmos / exposure
OF CORNEA: lagophthalmos / exposure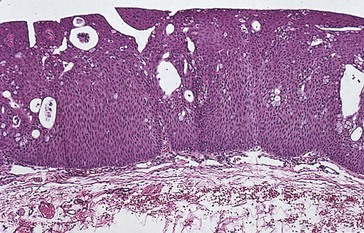

 of limbus; good prognosis, some scarring
of limbus; good prognosis, some scarring of limbus; poor prognosis, risk of perforation
of limbus; poor prognosis, risk of perforation


